PLHIV
Documents
The path that ends AIDS: UNAIDS Global AIDS Update 2023
13 July 2023
The 2024 global AIDS report The Urgency of Now: AIDS at a Crossroads, released 22 July 2024, is available here.
This report makes clear that there is a path to end AIDS. Taking that path will help ensure preparedness to address other pandemic challenges, and advance progress across the Sustainable Development Goals. The data and real-world examples in the report make it very clear what that path is. It is not a mystery. It is a choice. Some leaders are already following the path—and succeeding. It is inspiring to note that Botswana, Eswatini, Rwanda, the United Republic of Tanzania and Zimbabwe have already achieved the 95–95–95 targets, and at least 16 other countries (including eight in sub-Saharan Africa) are close to doing so. Also available: Additional resources (regional and thematic factsheets) | Annex 1: Progress towards the 2025 targets | Annex 2: Methods | Slide set | Press release | Microsite
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025

Feature Story
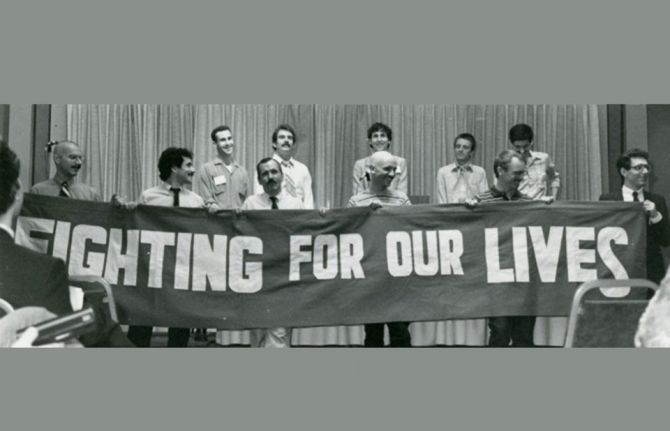
The Denver Principles: 40 years on
26 June 2023
26 June 2023 26 June 2023Text based on A Brief History of the Self-Empowerment Movement by Sean Strub, former Executive Director, The Sero Project
Forty years ago, visionary activists developed the Denver Principles manifesto, which shaped the active involvement of people living with HIV in the AIDS response. This was a historic first step towards the Greater Involvement of People with HIV (GIPA) principle, which promotes the meaningful participation of people living with HIV in decision-making, not as passive subjects but as protagonists fully involved in the response to AIDS.
This manifesto, written in June 1983, launched the self-empowerment movement for people living with HIV. As Sean Strub, former Executive Director of The Sero Project, writes, The Denver Principles document is historic in its assertion that those who have HIV have a fundamental and inalienable right to participate in decision-making that significantly impacts their lives and survival.” In language that has inspired people living with HIV over the last forty years, the manifesto asserts:
“We condemn attempts to label us as ‘victims,’ a term which implies defeat, and we are only occasionally ‘patients,’ a term which implies passivity, helplessness, and dependence upon the care of others.”
The Denver Principles outlined rights and responsibilities for people living with HIV and provided recommendations to healthcare professionals, family, and friends.
Today, our world has undergone important changes. Despite progress made in many areas of the AIDS response, stigma, discrimination and pervasive inequalities continue to harm the lives of millions of people living with and affected by HIV. So, have the Denver principles had an impact on the lives of the populations most affected by HIV over the last 40 years? Will the new challenges of our time demand a review and an update of the GIPA Principle? This is what leading HIV activists and UNAIDS have to say about it:
Erika Castellanos, Executive Director, Global Action for Trans Equality (GATE)
"The Denver Principles were the foundation of the GIPA Policy, which placed us, people living with HIV, at the center of the response. It gave us a voice; it gave us a seat at the table. Today, it is no longer enough; it is time to evolve from having a seat at the table to being the leaders of the table, the leaders in the HIV response."
Alex Garner, Director of Community Engagement, MPact Global
The Denver Principles were a watershed moment in the movement for the rights of people living with HIV. It’s been 40 years and the world, our communities, and the epidemic have fundamentally changed. A clear understanding of the intersectional issues that people living with HIV (PLHIV) face is essential for protecting and defending our rights. Key populations have been the most disproportionately impacted by this disease and an evolution of the Denver Principles needs to integrate the challenges faced by our communities and the structural homophobia and transphobia that have sustained this 42-year pandemic. PLHIV have a fundamental right to pursue a fulfilling sexuality and have control over their own bodies. An update of the Denver Principles requires advancing the audacity of a sexuality of people living with HIV, regardless of their viral load.
Rodrigo Olin, Board Co-chair, GNP+
Forty years on from this declaration, people living with HIV are still continuously treated and addressed as patients; passive entities who have no say about our treatments and the effects on our bodies – as though we are passive agents. People around the world are still diagnosed late, even in developed countries where tools to prevent and treat HIV are available. Challenges remain to effectively embrace and apply the GIPA principles in co-designing community interventions and HIV-care frameworks alongside physicians and researchers. HIV research at all levels requires the involvement of people living with HIV to continue moving forward the quality of life of people living with HIV, wherever they are in the world.
Joyce Ouma, Advocacy and Campaigns Officer, Y+ GLobal
I just learned of the Denver principles, and I am glad I did as through my advocacy journey, I have constantly been told by the seasoned advocates that I and other young people are lucky to be living with HIV now, now that there is minimal stigma, now that HIV has been differentiated, and now that we have access to antiretroviral treatment. This made me reflect on the journey that PLHIV have taken to belong.
The Denver principles are the cradle of the meaningful engagement of people living with HIV in all our diversity. As young people living with HIV, we have built upon the GIPA principles to advance our call for the ethical and meaningful engagement of young people in key decision-making spaces to ensure that the mistakes of the past are not repeated now. We now have people living with HIV clustered into networks to structure our engagement in key platforms. The Denver principles are still as relevant to us now as they were in 1983, and while we have a lot of milestones to celebrate 4 decades later, we are still lagging on the meaningful engagement of young people living with HIV.
The principles need to be revisited to reflect the modern challenges faced by populations living with HIV. Populations of young PLHIV and LGBTIQ are still blamed for the rising incidence rates despite us playing our role to maintain viral loads below detectable levels. Imagine being queer and living with HIV. We all still need to live with dignity.
Midnight Poonkasetwattana, Executive Director, APCOM Foundation
The adoption of the Denver Principles in the Asia Pacific region has been uneven. In our region, HIV prevalence is over five times higher for gay men and other men who have sex with men, transgender persons, and people who inject drugs. We did not reach the 2020 targets and sadly most countries and communities are not yet on-track to end AIDS by 2030.
Political leadership is needed to ensure that key populations and people living with HIV are part of the solutions and to ensure increased funding to adequately support key population-led and community-led organizations, networks, and services.
Sean Strub, Mayor of Milford, Pennsylvania, and Former Executive Director, The Sero Project
The Denver Principles impact goes far beyond the HIV epidemic, as the document has inspired people with various life-threatening or stigmatizing conditions around the world to assert their voices in the decision and policy-making that so profoundly affects their lives. Its fundamental message will not change, even as the document may be modified to reflect today's HIV epidemic and/or be made more broadly inclusive of other conditions. Integration of the Denver Principles ideals into healthcare, policy development and service delivery over the past 40 years has been remarkable, yet it is just the beginning. Change is slow and any paradigm shift as radical as that envisioned by the Denver Principles will meet resistance. But there is no stopping the movement that begun in that hotel room in Denver in 1983.
Vanessa Johnson, Co-Executive Director, RIBBON
We honor the courageous efforts of a group of men living with HIV who gave voice to a community of people who, in the early days of the AIDS epidemic, at times, were too fragile, too fearful, or were rendered invisible due to stigma, discrimination, and other systematic challenges.
Like most foundational or governing documents, the Denver Principles are applicable regardless of who is in leadership. Over the 40 years, we have witnessed a transition in national leadership in the United States from white gay men living with HIV to leadership that has grown more racially and ethnically diverse and inclusive of African Americans/Black, Latinx, Asian, Native American, etc., as well as sexual identities, sexual orientation, cultural expressions, and experiences, and with varying levels of accessibility.
Linda Scruggs, Co-Executive Director, RIBBON
As we celebrate the momentous 40th anniversary of the Denver Principles, we pay homage to a transformative document that has left an indelible mark on the AIDS response. Today, we stand on the shoulders of those courageous individuals who, in the face of adversity, gave voice to a community silenced by stigma, fear, and discrimination.
These principles have inspired countless individuals, empowering them to assert their rights and demand inclusion in decision-making processes that shape their lives. We must recognize that the journey toward achieving the vision of the Denver Principles is far from over. It is our collective responsibility to ensure that their voices are not only heard but amplified, as we strive for a more just and inclusive society.
In commemorating this milestone, we stand united in our commitment to uphold the principles' fundamental message: that every person, regardless of their background, deserves respect, dignity, and equal access to comprehensive care. The Denver Principles have become a cornerstone of our fight against stigma, discrimination, and structural inequalities, igniting a movement that refuses to be silenced.
Yvette Raphael, Executive Director, Advocates for the prevention of HIV
As we reflect on the past 40 years, we acknowledge the progress made and the lives touched by the principles' profound impact. Yet, we must also acknowledge the work that lies ahead. Change, especially transformative change, takes time and unwavering dedication. But together, as activists, advocates, and leaders, we have the power to shape a future where the Denver Principles become a reality for all. People living with HIV globally have benefitted from this vision of those who came before us. It is through their vision that we are able to live full and productive lives and we must never forget that. We are able to engage meaningfully in the response because of this declaration. Over the years women living with HIV become leaders in fighting for HIV prevention because of the Denver declaration showed us it could be done.
We are at a pivotal point in the fight against HIV. Our daughters, our children may face the same challenges as us. The focus now has to be on the prevention of HIV infection. We need to build on the GIPA principles to include the prevention of new HIV infections among adolescent girls and young women.
Why has the recognition and adoption of these principles been so uneven in the world? Because some countries still criminalize and stigmatize those living with HIV with impunity.
Immaculate Owomugisha, ICW Global
The Denver Principles are foundational to our human right to participate in the decision making that impacts our lives. GIPA has created opportunities for vibrant and meaningful engagement of communities of people living with HIV that have propelled the HIV response, however, persistent misogyny, intersectional stigma and discrimination continue to result in harmful tokenization of women living with HIV and spur lack of sufficient investments in networks of people living with HIV, particularly women’s networks around the world.
Neil McCulloch, Senior Policy Officer, Global Network of Sex Work Projects (NSWP)
Forty years on, little has shifted for sex workers and other key populations, who remain disproportionately impacted by HIV and accounting for over 70% of all new infections globally. The criminalisation of sex work, HIV status, drug use, same-sex sexual activity, and diverse gender identities, as well as persistent violence, stigma and discrimination, prevents the true meaningful involvement envisioned in the Denver Principles. With anti-rights narratives and regressive laws on the rise again, and increasingly shrinking funding available, we must re-double our efforts to remove these structural and societal barriers and ensure we prioritise key population-led activities, in order to realise the GIPA principles and truly move the dial in the HIV response.
Aditia Taslim, Advocacy Officer, International Network of People Who Use Drugs (INPUD)
“The HIV self-empowerment movement, catalyzed by the Denver Principles manifesto, has been important in galvanising the drug user movement. Although drug user activism has existed for decades, the Vancouver Declaration (2006) titled “Why the World Needs an International Network of Activists who Use Drugs,” not only served as the birth of International Network of People who Use Drugs (INPUD) but also, underlined the roots of all other harms and violations that people who use drugs experience—which are criminalisation, and the repressive and oppressive laws and policies that are fueled by prohibition, moralism, stereotypes and lies. The HIV crisis has provided legitimacy as well as resources for people who use drugs through provision of harm reduction services. Despite its success in bringing down number of new HIV infections in some regions, harm reduction has mostly become co-opted by a medicalised and pathologising approach, removing the rights to make choices regarding own bodies and lives. Only by dismantling prohibition, we will have a society that respects, protects, and promotes the right to self-determination over one’s body, decision and consciousness of people who use drugs.”
Christine Stegling, UNAIDS Deputy Executive Director, Policy, Advocacy and Knowledge.
“The Denver Principles continue to serve as a powerful reminder of the importance of the greater and meaningful participation by people living with HIV in shaping the policies and programs that affect their lives. As we commemorate the 40th anniversary of this groundbreaking document, UNAIDS remains committed to following this leadership, and continuing to put the voices and experiences of people living with HIV at the center of our efforts to end the epidemic.”
Related


Press Release
UNAIDS welcomes announcement by Colombian government that will enable people access to the most appropriate HIV treatment for them
12 June 2023 12 June 2023UNAIDS welcomes the issuance of Resolution 881 of 2023 by the Ministry of Health of Colombia, which initiates the administrative procedure to evaluate the existence of reasons of public interest for issuing a compulsory license for dolutegravir (DTG)-based regimens. According to the ministerial resolution, the impact of this measure could mean a significant reduction of more than 80% of DTG’s price.
Dolutegravir (DTG) is an antiretroviral integrase inhibitor, recommended by the World Health Organization (WHO) as a first-line treatment option for people living with the human immunodeficiency virus (HIV). Regarding viral suppression and disease reduction, treatments incorporating DTG-based regimens have demonstrated greater adherence due to their lower incidence of adverse events while presenting enhanced effectiveness, safety, and reduced likelihood of resistance development.
Compulsory licensing is a provision in the World Trade Organization (WTO) Agreement on Trade Related Aspects of Intellectual Property Rights (“TRIPS Agreement”), that enables governments to supply its citizens with generic versions of patented treatments either through domestic production or imports, ensuring drug prices are affordable. WTO Inter-ministerial 2001 Doha Declaration reaffirmed the rights of member states to make use of all flexibilities in the agreement to protect public health, including compulsory licenses, “and the freedom to determine the grounds upon which such licenses are granted.” More recently, in the 2021 Political Declaration of the United Nations General Assembly High-level Meeting on AIDS, countries have committed to make use of TRIPS flexibilities “specifically geared to promoting access to medicines.”
"This resolution is a step forward to provide equal and sustainable access to best HIV treatment options for all people living with HIV in Colombia, nationals and migrants. This action shows the government’s commitment to close the treatment gap with assured quality affordable essential medicines which are easy to take and very well tolerated.”, says Andrea Boccardi, UNAIDS Director for the Andean Countries (Peru, Ecuador, Bolivia, and Colombia. "The government issued national guidelines in 2021, in line with WHO recommendations, but until now high prices of DTG have remained an obstacle to make it widely accessible to people living with HIV in Colombia."
The Colombian League for the Fight against AIDS and the IFARMA Foundation also celebrated the decision from the Colombian government. Both institutions participated on behalf of civil society in the updating of the Clinical Practice Guidelines (CPG) based on scientific evidence for the care of HIV/AIDS infection in adults, pregnant women and adolescents.
"The decision validates past initiatives of civil society in Colombia to achieve greater coverage of simplified treatments with fewer adverse effects at the lowest possible price, while at the same time it will reinvigorate the efforts of community-based organizations in education and promotion of adherence to ARVs, recognizing that structural barriers are factors that facilitate or hinder adherence to antiretroviral treatments", says Jorge Pacheco, Director of the Colombian League for the Fight against AIDS.
“Through this measure Colombia is taking an important step to guarantee people’s access to the most appropriate medication for them in line with international recommendations and commitments”, says Luisa Cabal, UNAIDS Regional Director for Latin America and the Caribbean. "Timely access to effective HIV treatment can save lives, improve health outcomes, enhance the quality of life, and contribute to the overall well-being of individuals living with HIV. This measure shows commitment to the global effort to combat inequalities in access to health."
UNAIDS commends and supports the Ministry of Health for its proactive approach to pursuing public interest and urges all stakeholders to collaborate in implementing Resolution 881 of 2023.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS Latin America and the CaribbeanDaniel de Castro
tel. +507 6998 3175
decastrod@unaids.org
Region/country




Feature Story
How working with providers of natural and holistic medicine for complementary self-care techniques is helping Nicaragua increase adherence to HIV medicines and reduce new infections
29 May 2023
29 May 2023 29 May 2023Right after taking his HIV treatment each morning, Antonio Hooker prepares a kit of fresh herbs and fruits he has bought at the local market to cross the Bilwa area, a village on the northern Caribbean coast of Nicaragua, as a health promoter for the Association of People Living with HIV (ASONVIHSIDA). He strengthens HIV prevention knowledge among vulnerable groups in his indigenous Miskitu community. He also teaches community leaders and people living with HIV or other health problems to use the power of natural medicine in conjunction with antiretroviral medicines to improve their immune systems.
Antonio is one of the dozens of volunteers and community promoters who have been certified by the Nicaraguan AIDS Commission, the Ministry of Health and the Institute of Natural Medicine and Complementary Therapies through training in "Self-Care in Sexual Reproductive Health and HIV from the Perspective of Natural Medicine".
Since his diagnosis 17 years ago, Antonio has learned the importance of self-care. He now shares his knowledge and training experiences with family members and others living with HIV in remote communities along the Nicaraguan coast.
"The course opened my mind to the importance of natural medicine and traditional practices, such as massage and meditative activities," says the health promoter. "We know these techniques work because we see improvement in our health while seeing progress in adherence to HIV treatment, as well as strengthening social, community networks and relationships within the families of people living with HIV."
The course "Self-care in Sexual Reproductive Health and HIV from the Perspective of Natural and Holistic Medicine" aims to provide guidelines on self-care for people living with HIV or similar conditions and their families. Through the appropriate use of medicinal plants, reflexology (a system of massage used to relieve tension and treat illness, based on the theory that there are reflex points in the feet, hands and head linked to each part of the body) and complementary therapies, such as the practice of the Chinese martial art and system of callisthenics well known as Tai Chi Chuan, which consists in sequences of slow controlled movements.
"The objective is to build skills and abilities among people living with HIV, volunteers and active community members to develop a comprehensive approach to sexual and reproductive health, sexually transmitted infections (STIs) and HIV," explains Dr Enrique Beteta, Nicaragua's Deputy Minister of Health. "It also allows people to access information and linkage to health services at the local level to take care of their health and the well-being of those around them."
The services harnessing natural medicine are complementary, not alternative, to HIV medicines. Indeed, the programmes have helped increase uptake of and adherence to HIV medicines.
Nicaragua’s comprehensive approach and partnership with communities has helped it to advance progress on treatment and prevention. Since 2010, Nicaragua has experienced a 20% decrease in new HIV infections, while in Latin America, new infections have increased by 5% in the same period. About 11 000 people live with HIV in the country, and 90% have been tested and know their positive diagnosis, above regional (82%) and global (85%) rates.
The course offers 84 hours of theoretical and practical training, a quarter of which is focused on Sexual and Reproductive Health and HIV modules. The certification also focuses on putting people at the centre, not only as beneficiaries but also as key protagonists, participating, exercising and demanding access to their rights for equality and equity.
"The course also aims to identify in people the autonomy to make decisions, as transformative agents, in a framework of respect, solidarity and social justice," explains Marie Engel, Director of the UNAIDS Multi-country Office for Guatemala, Honduras and Nicaragua. "Working to eliminate stigma and discrimination is also an important outcome of this initiative."
Watch
Region/country




Feature Story
Brazil announces its commitment to the global initiative against HIV-related stigma and discrimination
19 May 2023
19 May 2023 19 May 2023Brazil has joined the 34 countries that are part of the Global Partnership to take action to eliminate all forms of HIV-related stigma and discrimination. The country's entry into this group of nations was announced at a celebratory event of the International Day Against Homophobia, Biphobia, and Transphobia, held in Brasilia, Brazil’s capital and organized in partnership by UNAIDS, ILO, and the Ministry of Human Rights and Citizenship.
The Global Partnership is an initiative launched through a call for action from the NGO Delegation to the UNAIDS Programme Coordinating Board (PCB) in 2018 to remove HIV related stigma in six settings: healthcare, justice, community, workplace, educationa and humanitarian. It is co-convened by UNAIDS, UN Women, the United Nations Development Programme (UNDP), the Global Network of People Living with HIV, and the Global Fund to Fight AIDS, Tuberculosis, and Malaria. It is also supported by a technical working group composed of 10 United Nations agencies and 24 partners and civil society organizations.
With Brazil, now 35 countries have formally joined the Global Partnership, committing to act against HIV-related stigma and discrimination in the contexts of healthcare services, educational settings, workplaces, justice systems, domestic and community environments, emergency systems, and humanitarian crises.
According to Luisa Cabal, the Regional Director of UNAIDS in Latin America, Brazil's entry into the Global Partnership is a significant step in the collective response against HIV-related stigma and discrimination in Latin America and the world. "By joining this initiative, Brazil reaffirms its commitment to defending human rights, promoting social inclusion, and eliminating barriers to access prevention, diagnosis, treatment, and ongoing response to HIV," she explains.
By joining the Global Partnership, Brazil will have access to a platform that will allow the country to share experiences and best practices with the other participating countries, creating opportunities for collective learning, strengthening the joint response to HIV-related stigma and discrimination.
"It is important to highlight that by joining the Global Partnership, Brazil will also reinforce its leadership role in the region and global diplomacy for health and human rights, demonstrating its commitment to equity and social justice," emphasizes Luisa Cabal.
It is indeed a precedent for the GP that commitment to join the Global Partnership has been witnessed by two Ministers.
Minister of Human Rights and Citizenship Silvio Almeida reiterated his unrestricted support and commitment to public policies promoting and protecting the rights of LGBTQIA+ people. ”For those who suffer violence, and are killed simply for being who they are, these people will be protected in a public commitment, and I renew this commitment not only as Silvio Almeida, but as Minister of State for Human Rights of Brazil” emphasized H.E.
Representing the Ministry of Health Helvécio Miranda, Secretary of Specialized Health Care, similarly shared the Ministry's commitment to embrace the agenda of LGBTQIA+ rights and ensure comprehensive healthcare access for all people emphasizing on a gender approach, and with a special focus on those at risk, with specific needs, or experiencing different forms of violence.
Vinícius Pinheiro, Director for Brazil at ILO, embraced the significance of the Global Partnership in promoting social justice and decent work with inclusion and opportunities for all people so that no one is left behind.
Region/country




Feature Story
Leave no one behind and that includes people who use drugs
04 May 2023
04 May 2023 04 May 2023Daouda Diouf comes daily to the Fann Hospital compound daily. He is one of 250 people enrolled in CEPIAD*’s opioid substitution therapy programme (OST). OST is a globally recognized intervention to reduce injecting behaviours that put people who inject drugs at risk of contracting HIV and other blood-borne diseases, such as viral hepatitis.
“I am here to take my treatment and I am also a tailor, so I teach a few other users of drugs how to sew,” Mr Diouf said, cutting fabric in his makeshift outdoor workshop. Keeping occupied and selling his wares has helped him stay healthy for the last seven years.
Another enrollee agrees. He has found a passion for gardening and now oversees other patients at the centre’s green area.
For El Hadj Diallo, planting seeds, pruning trees is like a type of therapy. “When we are here, we forget our problems, I am happy doing it and it’s therapeutic for me,” he said.
Their other therapy consists of a daily dose of methadone. Mangane Boutha, the centre’s pharmacist carefully measures and distributes each dose in his office.
“Methadone is a medicine that acts as a heroin substitute, in our case it’s a syrup that is dosed in 10mg/ml portions with doses varying from patient to patient,” he explained.
Founded in 2014, CEPIAD has cared for more than one thousand people and is one of the first harm reduction centres in West Africa. Aside from opioid substitution, clean needle exchange and psychosocial support, they also offer health care.
“CEPIAD has become a testing and diagnostics center for HIV, and also tuberculosis as well as hepatitis and we distribute condoms,” said Dr Idrissa Ba, who coordinates the centre.
In Senegal, HIV prevalence among people who inject drugs is 9%, well above the 0.5% among the general population. Globally, due to stigma and criminalization, people who inject drugs face a 35 times higher risk of acquiring HIV than people who do not inject drugs.
Three-quarters of patients here are men but CEPIAD has been working hard to reach more women. Among people who use drugs, women are more likely to live with HIV, according to Dr Ba.
Mariama Ba Thiam, who formerly used drugs, lived for years on the streets. She is now a peer educator in Dakar. “I go out into the community and visit colleagues to raise awareness about getting off drugs and also how to reduce health risks so I refer them to CEPIAD and they can do like me, stop drugs,” she said.
Her plea: Get more funds to get more women and young people to come to the centre.
In Senegal, whilst drug use is a criminal offense, CEPIAD’s work has the support of the government, the United Nations as well as other partners.
On international Harm Reduction day, UNAIDS firmly believes that if we are to end AIDS by 2030, we can’t leave anyone behind. And that includes people who use drugs.
*The Centre de Prise en Charge Intégrée des Addictions de Dakar (CEPIAD)
Watch video
Region/country
Related




Feature Story
The power of visibility — My story as the first person who came out as a person living with HIV in Fiji
18 April 2023
18 April 2023 18 April 2023Jokapeci Cati is the Program Manager and founder of the Fiji Network for Positive People (FNP+). This is her self-told story of how she became the first person living openly with HIV in Fiji.
I grew up in the harbour town of Suva. I was brought up in the Seventh Day Adventist Church. During youth camps we had two sessions on HIV. To me it was just a session. I had this perception that I am not promiscuous so I can’t become HIV positive.
I got married at 21 and got infected in my marriage. I was diagnosed in 2000 but I suspect I was living with HIV since 1999. My husband was sickly and became bed ridden. I did not blame him. I felt like he got infected before we were married and did not know he was living with HIV. In 2003 he died due to AIDS-related causes. He was 31.
We did not have treatment in Fiji at that time. People living with HIV were just monitored. When I was diagnosed they told me “you have to look after yourself because you can die”. In the initial stages there was depression, denial and stress. But as soon as I got diagnosed one of my dreams was to meet another person living with HIV.
With my family there was no change in the way they treated me. It was support from the word go. I did not see any element of discrimination from my parents and siblings.
Going public
Coming out was not an overnight decision for me. It took me six months to juggle the pros and cons. Somehow my mind was not dwelling on the negative. Because there was no support system in place at the time, I felt the need to speak out.
So I started with the church. I went to the pastor and told him of my diagnosis. Then I had to disclose to my church community. The hardest bit was opening up to your very own people. Once I gained the support of the church I spoke to the Council of Chiefs, Fiji’s traditional leaders forum. Because those platforms gave me a positive reception I then went to the media because I felt I was ready to speak to the nation.
Organising and advocating
In 2003 I was privileged to meet the right people at the Ministry of Health and we coordinated the first meeting of FNP+. By 2004 I got the organisation registered, up and running.
From the start I was advocating for treatment because I could see my first husband dying. The Ministry of Health’s HIV coordinator at the time, Maire Bopp Dupont, connected us to the Asia Pacific Network of People Living with HIV. That is how I got to know that other countries in the region were offering treatment. We went to the Council of Chiefs and Parliamentarians to advocate. The Health Ministry at the time was saying “we are not ready… we need to put the systems and structures in place”. I think because we came out publicly it put some pressure on them. The very next year, in June, treatment was available.
It was exciting. For the first time we felt the advocacy was worth the sacrifice. Our work involved talking to nurses, doctors and civil society organisations that were part of the care team. I started antiretroviral therapy five years ago when we adopted the “treat all” policy. It is so exciting that we are able to take treatment with the assurance that we would live! And it is for free!
Living life fully
I did not let HIV decide my future. Because of being part of the FNP+ management team I found the need to venture into education. I got a degree in psychology and social work from the University of South Pacific.
When I lost my first husband I was in this dilemma about whether to have children. I met my current husband in the HIV organisation. When we decided to have children, it was a public affair in Fiji. I was an HIV positive, pregnant woman. It was a learning curve for me and the entire nation.
The UNAIDS Goodwill Ambassador for the Pacific, Ratu Epeli Nailatikau, was Fiji’s President at the time. He made it his business to come to the hospital during my delivery and my first son’s HIV test. He wanted a copy of my son’s HIV negative test result. This became his advocacy document. He has been spreading the message since then that there is no need to discriminate against women living with HIV who want to have children. It’s time we support them through prevention of mother-to-child transmission (PMTCT) treatment. I am now the mother of three HIV negative children.
The way forward
We are working to get FNP+ funding from the Global Fund to continue our national activities and regional support. I’m glad the focus is now on community-led monitoring and services and that it’s coming from the donor’s mouth.
Other Pacific countries don’t have networks of people living with HIV. Fiji is the only one. People throughout the region are living in isolation. Our second piriority is to organise at the regional level.
Our third challenge is that although everyone who is living with HIV is encouraged to take treatment, we have stockouts. At one point we weren’t getting Dolutegravir so people had to change to a combination of drugs until it became available. Labs are also a challenge, especially the turnaround time for viral load tests. If FNP+ does not continue to apply pressure to address these issues people would suffer silently.
HIV in a small island developing state
For sure people living with HIV from key population communities have had a more difficult time. They were ostracised, they were discriminated against. I did not face that. There was a time, around 2004 and 2005, when people who died due to AIDS had to be burned at night before the sun rose! The stigma and discrimination are not as bad as that now, but they still exist.
I think in the Pacific it is really hard to come out with your HIV status because of our small size. We have these connected communities and if someone comes out it is easy to trace who else could be HIV positive. We have this communal upbringing so people don’t want any negative repercussions for their families.
When other people living with HIV meet me, they are happy. They want to come out and speak, but they don’t know how. Now there is funding for this community engagement in more Pacific countries. We just need to give them support and a bit of time.
Fiji recently received technical support for the seventh cycle of Global Fund applications and the Indo Pacific HIV Prevention Program supported by the Australian Department of Foreign Affairs and Trade (DFAT). UNAIDS Pacific supports peer network meetings to encourage sharing among PLHIV. UNAIDS also recently collaborated with Rainbow Pride Fiji Foundation, the Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM) and the National Association of People with HIV Australia (NAPWHA) to develop a PLHIV booklet in the local languages. This booklet provides information on living with HIV and helps empower PLHIV to take control of their health and wellbeing. This project is supported by the New Zealand Ministry of Foreign Affairs and Trade and DFAT.
Region/country
Related

Press Statement
UNAIDS Executive Director Message on World TB Day – Yes, we shall and we can end TB among people living with HIV!
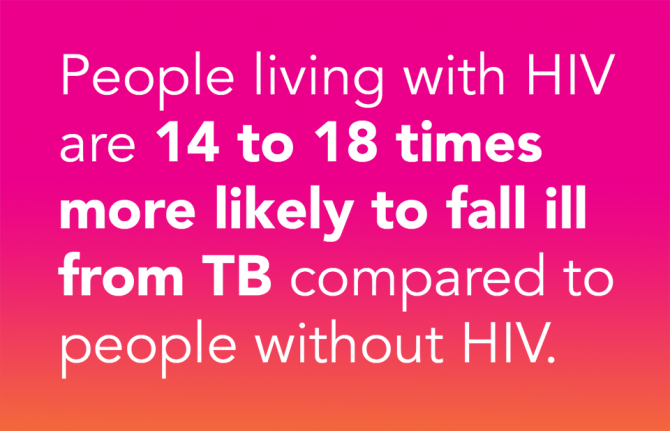
24 March 2023 24 March 2023Today, on World TB Day, we must recognize the urgent need to end the TB epidemic around the world, especially among people living with HIV.
TB remains a leading cause of severe illness and death among people with HIV. According to the World Health Organization Global TB Report 2022, people with HIV are 14-18 times more likely to fall ill from TB compared to people without HIV. About one in three AIDS related deaths were in 2021 were due to TB. We cannot allow this to continue. We must ensure that all people living with HIV and those vulnerable to TB have access to TB prevention, diagnosis, and treatment services.
We continue to miss opportunities to deploy the tools we have against HIV / TB co-infection. Almost half of people living with HIV who developed TB in 2021 were not diagnosed or reported to have TB and coverage of TB preventive therapy among eligible HIV positive persons remains at only 42%.
Like in the responses to HIV and COVID 19, inequalities are the root cause making some people at higher risk of TB, due to social economic, geographic, gender factors and humanitarian and crisis situations. Legal and policy environments also affect access to health services for those who need them the most. We shall not forget that for any health programs to work, we need to put people at the center and engage beneficiaries, particularly the less served communities, to be part and parcel of the planning, implementation and monitoring the response.
Today on World TB Day, I would like to call on all our partners to redouble efforts to ensure early identification, treatment, and prevention of TB in people living with HIV by scaling up the recommended screening and diagnostic tools, providing integrated quality treatment and care, rolling out short-course TB preventive treatments, and removing barriers that affect the smooth implementation of programs.
By ending TB among people living with HIV, we will save more lives, reduce suffering, and move closer to ending both epidemics for good.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work




Press Statement
One year on: We must sustain the HIV response in Ukraine
23 February 2023 23 February 2023One year on, the war in Ukraine continues to inflict massive suffering and destruction. Since the start of the war on 24 February 2022, more than 13.5 million people have been internally displaced or forced to flee to neighboring countries as refugees, including people living with HIV and key populations.
Ukraine, the country with the second-largest AIDS epidemic in the Eastern Europe and Central Asia region, has been hit hard by the war.
The country was making strong progress in the AIDS response by: 1) increasing the number of people living with HIV on life-saving medicine (more than 150 000 people are on treatment out of 240 000 living with HIV); 2) working hand in hand with community-based organisations and 3) reaching full state financing of innovative HIV prevention services among key populations.
The shock of the war pushed all stakeholders to protect those precious gains.
The government of Ukraine and civil society partners have received enough anti-retroviral therapy (ARV), tuberculosis medicine, and opioid substitution therapy (OST) to provide uninterrupted treatment for everyone with the support of the Global Fund to Fight AIDS, Tuberculosis and Malaria, the United States President’s Emergency Plan for AIDS Relief (PEPFAR), UNAIDS, and other partners.
Civil society has been the engine of the national HIV response along with the Ukrainian Public Health Centre before the war and throughout the year. They have delivered services, medicines, and humanitarian aid to those in need without fail despite bombings, attacks, lack of electricity and reduced access to the east and south of the country.
This effort needs our ongoing support and funding. We cannot let Ukraine’s HIV response fall back.
UN agencies and partners on the ground have been working closely with local authorities to reach and help people in need. More recently they have delivered humanitarian assistance to hard hit territories in the country that have only now become accessible.
“Delivering essential aid and assistance relies on collaboration,” said Winnie Byanyima, UNAIDS Executive Director. “A coalition of government, civil society and international organisations has been and continues to be a cornerstone of the effective HIV response in Ukraine during the war. UNAIDS stands in solidarity with all the people and our partners working so hard on the frontlines.”
A UNAIDS Emergency Fund has enabled partners across the country to sustain HIV care and support services, as well as providing direct humanitarian assistance and targeted support to the most vulnerable. This has meant, for example, creating dozens of shelters for internally displaced persons, including people who use drugs, LGBTIQ+ people, and other key populations linking HIV service providers with available humanitarian assistance programmes. The Fund has received support from the Red Cross Monaco, the United States of America and Germany.
With further funding from Germany, civil society organizations in Moldova, Poland, and other neighboring countries united their efforts to improve access to services for Ukrainian refugees living with HIV.
UNAIDS has issued an urgent call to the international community for additional funding for civil society organisations to keep providing essential HIV support services in Ukraine and in countries receiving refugees in need of HIV services.
UNAIDS will continue to support HIV prevention, testing, treatment, care and support for people across Ukraine affected by the war and people displaced by the conflict.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Key humanitarian messages
War in Ukraine and the HIV response
Region/country




Feature Story
Thailand partners develop community-led HIV care curriculum
23 February 2023
23 February 2023 23 February 2023For 20 years Kochaphan Wangtan has been a community health worker, serving other people living with HIV (PLHIV) in Thailand.
“I’ve seen many friends living with HIV come to care very late with opportunistic infections,” she said.
“I focus on helping to bring them in and provide support to start antiretroviral treatment right away and I also conduct home visits, counselling and psychosocial screening so I can link them to services they need,” Ms Wangtan explained.
Ms Wangtan is from the Jai-Prasan-Jai Comprehensive Continuum of Care Center (CCC) from the Phan District Hospital in Chiang Rai province. She is one of almost one thousand PLHIV health workers who are embedded in more than 230 Thai hospitals and serve almost 60,000 PLHIV annually.
For the first time, the country has rolled out a national community health worker certification for these volunteers. The initiative is called “A Comprehensive Continuum of HIV/AIDS Care and Support for and by People living with HIV.” The curriculum was developed by the Ratchasuda College of the Mahidol University through close collaboration with the Thai Network of People Living with HIV/AIDS (TNP+) as well as support from the Health Ministry’s Division of AIDS and STIs and the National Health Security Office. USAID-PEPFAR via the III Unify Collaboration Programme and UNAIDS provided technical and financial support.
“PLHIV volunteers have provided the first community engagement in the HIV response since the start of the epidemic in Thailand,” said UNAIDS Country Director, Patchara Benjarattanaporn. “Peer-led support boosts treatment initiation and retention and is central to the HIV response,” she said. This initiative ensures that PLHIV-led health services are standardized, recognized and valued.
Two modules are delivered over 90 hours. The first module focuses on theoretical training, including on holistic follow-up care, treatment adherence counselling and developing a comprehensive service plan. The second module is practical. Along with its HIV focus, the curriculum also integrates tuberculosis, sexually transmitted infections, Hepatitis C and non-communicable diseases. Earlier in the month the first cohort of 46 PLHIV health workers received their certification.
Dr. Wachara Riewpaiboon, a rehabilitation physician and former Ratchasuda College Dean, developed the curriculum.
“The health system is not only for health professionals… It belongs to everyone,” she said. “Getting an HIV diagnosis does not help clients understand what they are facing. When people living with HIV tell their story, it is very different knowledge they are imparting. The knowledge that helps people make decisions for themselves usually comes from peers, not doctors.”
For her, care goes beyond medicine.
“It is not only biology that we are dealing with, but also psychology and our interaction with our social environment—how people look at people living with HIV and how they perceive themselves,” Dr Riewpaiboon continued. “It is very important to help people see the positive side of their experience.”
According to Nurse Chulaporn SingPae, an HIV Coordinator at the Phan District Hospital, PLHIV volunteers help with counselling, adherence, missed appointment follow-up, home visits, treatment deliveries, overcoming stigma including self-stigma and promoting understanding of U=U, undetectable equals untransmittable. (An undetectable viral load means the virus is not transmittable aka untransmittable.) The training ensures that these contributions are recognized by the health system as meeting quality standards.
Now that the course has been developed and tested, the curriculum has been recognized by the National Health Security Office (NHSO). Thai civil society organizations, who provide HIV and STI services with certified community health workers have been accredited and are eligible to register as health service units in the Universal Health Coverage scheme. Having supported the development and pilot of the curriculum, UNAIDS is now supporting a study to cost these services. The office is also working to promote sufficient and sustainable financing for community-led health services for PLHIV and key populations.
“This training is going to become the guarantee that a peer educator provides a high quality of service, in a holistic way, which encompasses not just the physical but also the mental, emotional and social aspects,” said Apiwat Kwangkeaw, Chairperson of the Thai Network of People living with HIV/AIDS. “As this becomes institutionalized, we are sending a message to the health system as a whole to let the community of peer educators be an equal partner,” he said. Mr Kwangkeaw hopes this will translate into sustainable domestic financing for community-led health services and better quality of life for PLHIV.