Epidemiology



Update
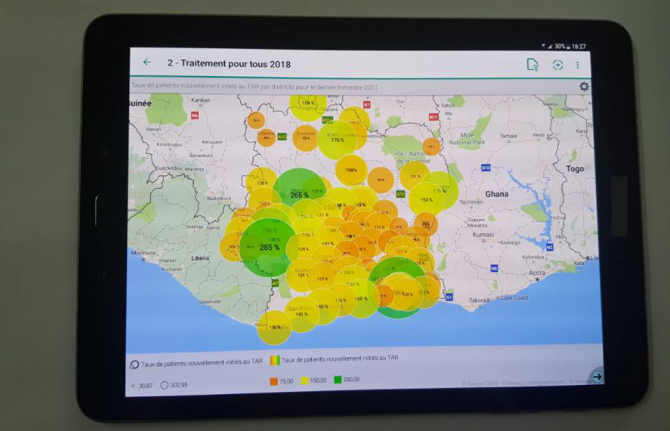
Launch of HIV situation room in Côte d’Ivoire
27 March 2018
27 March 2018 27 March 2018Côte d’Ivoire has become the first francophone country, and the first in western and central Africa, to launch an HIV situation room, a software platform designed to support informed decision-making.
This innovative tool strengthens national information systems through real-time visualization of information from multiple data sets. It will enable leaders and programme managers to make timely decisions to improve health programmes to achieve the 90–90–90 targets, whereby 90% of people living with HIV know their HIV status, 90% of people who know their HIV-positive status are accessing treatment and 90% of people on treatment have suppressed viral loads, by 2020.
The situation room is the result of a collaboration between the Côte d’Ivoire Ministry of Health and Public Hygiene, the United States President’s Emergency Plan for AIDS Relief through the Centers for Disease Control and Prevention, and UNAIDS. It was launched by Raymonde Goudou Coffie, the Minister of Health and Public Hygiene of Côte d’Ivoire, and Michel Sidibé, Executive Director of UNAIDS, on 26 March in Abidjan.
Quotes
“The situation room will allow the use of epidemiological data, strategic information and community-based data in real time to assist decision-making.”
“The Ebola epidemic was only ended in Côte d’Ivoire thanks to a real-time information system. The development of health in the future will depend on our ability to show information in real time and the local level.”
“I congratulate UNAIDS for the situation room, which will help to improve the response in order to achieve the 90–90–90 targets.”
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025

Feature Story
Checking HIV data at every step
22 March 2018
22 March 2018 22 March 2018No disease has the same level of timely and accurate data collection, analysis and distribution as HIV. With credible and up-to-date data, countries and the international community can plan effective AIDS responses. They can focus services on the locations and populations that most need them, increasing impact and decreasing costs.
The responsibility for producing what is acknowledged to be the gold standard information on the global HIV epidemic rests with UNAIDS. For the information to be useful, though, it must be credible. And to be credible, it must be collected properly, thoroughly checked and proven to be accurate.
All HIV-related estimates published by UNAIDS are based on data collected in the countries and communities where the people who are living with and affected by HIV reside. In each country, teams of experts—epidemiologists, demographers, monitoring and evaluation specialists and others—use UNAIDS-supported software called Spectrum once a year to make estimates of the number of people living with HIV, the number of new HIV infections, the number of AIDS-related deaths, the coverage of antiretroviral therapy, etc. The data files produced by the software in the countries are then sent to UNAIDS.
How the data are estimated depends on the nature of the HIV epidemic in the country. In countries where HIV has spread to the general population, data are obtained from pregnant women attending antenatal clinics. In the past, only a sample of pregnant women who went to one of a network of clinics would be tested for HIV as part of surveillance efforts. Increasingly, however, countries have moved to using programmatic data about the level of HIV infection among all pregnant women tested at health facilities. These data, combined with data from nationally representative population-based surveys—which have broader coverage and include men, but are conducted less frequently—are used in the model, together with a set of assumptions, to calculate HIV prevalence, HIV incidence, AIDS-related deaths, the coverage of antiretroviral therapy and more.
Other countries have low-level HIV epidemics. If HIV transmission occurs mainly among key populations (people who inject drugs, sex workers, gay men and other men who have sex with men, transgender people and prisoners), data from HIV prevalence studies—which are usually focused on key populations—are most often used to calculate national estimates and trends. Estimates of the size of key populations are being calculated in more and more countries. If studies are not available, estimates are made based on data from the local region and with agreement among experts. Other sources of data—including population-based surveys and testing of pregnant women—are used to estimate HIV prevalence among the general population. HIV prevalence and the number of people on antiretroviral therapy are then used to derive national HIV trends. An increasing number of countries are using the number of deduplicated HIV case reports to estimate HIV incidence.
UNAIDS doesn’t just take data from countries uncritically and publish, though. The files submitted by the countries are reviewed by UNAIDS to ensure that the results are comparable across regions and countries and over time.
There is also ongoing validation of the Spectrum outputs with other data to check how accurately the estimates match with reality. For example, researchers compared Spectrum data with data on women attending antenatal clinics, census data and population survey data from a study in Manicaland, Zimbabwe. The Spectrum estimates of HIV incidence and prevalence were found to be generally in good agreement with the data, although some discrepancies were found.
In 2016, UNAIDS compared the quantities of medicines exported by generic medicine producers and found those to be broadly similar to programmatic reports of medicine usage and stocks in countries. Also, the recent Population-Based HIV Impact Assessments surveys allow a comparison of the coverage of antiretroviral treatment, as they collect self-reported adherence to antiretroviral therapy and also aim to measure the presence of antiretroviral medicines directly in blood samples. In many countries, the resulting coverage confirms the coverage reported by programmatic data—where results don’t seem to concur, further investigations at the facility level are undertaken. Such research and triangulations help to make data more precise and refine the Spectrum model.
How well estimates on access to antiretroviral medicines agree can be seen in the two graphs on HIV treatment in South Africa. The first shows how close the procurement data for antiretroviral medicines match the number of people reported to be accessing the medicines. The second shows how the UNAIDS estimate of the percentage of people living with HIV accessing HIV treatment agrees with the percentage estimated by the South Africa Human Sciences Research Council in 2012.
There are several situations in which UNAIDS won’t publish data, because of uncertainty around the quality of the information. For example, UNAIDS does not give estimates in some countries that have concentrated epidemics of mother-to-child transmission of HIV and of the number of children living with HIV unless there is proper supporting evidence. Where historical data can’t back up trends in HIV incidence, UNAIDS doesn’t publish the past data. And UNAIDS also doesn’t publish country estimates if further data or analyses are needed to produce valid estimates.
The integrity of UNAIDS data is also ensured through an annual update of the Spectrum model. The model is refined as new data become available, such as updated information on the probabilities of mother-to-child transmission of HIV, the age at which children start antiretroviral therapy, age and sex patterns of HIV infection, the effectiveness of antiretroviral therapy in reducing mortality and incidence, etc. These changes in the model can, however, lead to changes in estimates for both the current year and past years, resulting in the need to issue a full new set of historical data each year.
By continually refining the data collection and validation process, UNAIDS is making sure that the data it publishes continue to be valued and respected by the people and organizations that are working towards ending AIDS by 2030.
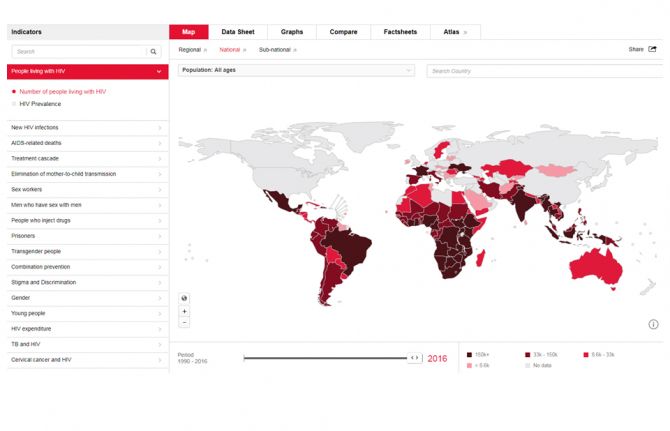
AIDSinfo
Publication
Resources
Documents
Recent infection testing algorithm technical update — Applications for HIV surveillance and programme monitoring
01 March 2018
This technical update provides public health officials with guidance on applying HIV incidence assays and testing algorithms for recent HIV infection in order to monitor the HIV epidemic and assess the impact of interventions. A major theme of this update is the importance of calibrating two of the key performance characteristics of recent testing infections algorithms—mean duration of recent infection and false recent ratio— to account for the context in which the testing is being done. This technical update also describes several emerging use cases in the application of recent infection testing algorithms and tests, including those for individual-level use. A final section on further research directions is provided to highlight areas that still require investigation.
Related
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
UNAIDS data 2024
02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
Domestic revenues, debt relief and development aid: Transformative pathways for ending AIDS by 2030, Report on Western and Central Africa
18 September 2024
Domestic revenues, debt relief and development aid: Transformative pathways for ending AIDS by 2030, Report on Eastern and Southern Africa
18 September 2024
UNAIDS information/guidance note on the mpox response
30 August 2024
Documents
2017 Global AIDS update - Ending AIDS: progress towards the 90–90–90 targets
20 July 2017
This report clearly demonstrates the power of the 90–90–90 targets and what can be achieved in a short time. It shows that innovations are possible at every level—from communities to research laboratories, from villages to cities. It illustrates the power of political leadership to make the impossible possible.
Related
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
UNAIDS data 2024
02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
Domestic revenues, debt relief and development aid: Transformative pathways for ending AIDS by 2030, Report on Western and Central Africa
18 September 2024
Domestic revenues, debt relief and development aid: Transformative pathways for ending AIDS by 2030, Report on Eastern and Southern Africa
18 September 2024
UNAIDS information/guidance note on the mpox response
30 August 2024


Press Release
The scales have tipped—UNAIDS announces 19.5 million people on life-saving treatment and AIDS-related deaths halved since 2005
19 July 2017 19 July 2017The 90–90–90 targets are galvanizing global action and saving lives. Eastern and southern Africa leading the way in reducing new HIV infections by nearly 30% since 2010—Malawi, Mozambique, Uganda and Zimbabwe have reduced new HIV infection by nearly 40% or more since 2010. Concerted efforts still needed for children, adolescents, men and key populations, and in certain regions.
GENEVA/PARIS, 20 July 2017—UNAIDS has released a new report showing that for the first time the scales have tipped: more than half of all people living with HIV (53%) now have access to HIV treatment and AIDS-related deaths have almost halved since 2005. In 2016, 19.5 million of the 36.7 million people living with HIV had access to treatment, and AIDS-related deaths have fallen from 1.9 million in 2005 to 1 million in 2016. Provided that scale-up continues, this progress puts the world on track to reach the global target of 30 million people on treatment by 2020.
“We met the 2015 target of 15 million people on treatment and we are on track to double that number to 30 million and meet the 2020 target,” said Michel Sidibé, Executive Director of UNAIDS. “We will continue to scale up to reach everyone in need and honour our commitment of leaving no one behind.”
The region showing the most progress is eastern and southern Africa, which has been most affected by HIV and which accounts for more than half of all people living with HIV. Since 2010, AIDS-related deaths have declined by 42%. New HIV infections have declined by 29%, including a 56% drop in new HIV infections among children over the same period, a remarkable achievement resulting from HIV treatment and prevention efforts that is putting eastern and southern Africa on track towards ending its AIDS epidemic.
WHAT’S ON TRACK
90–90–90 progress
The report, Ending AIDS: progress towards the 90–90–90 targets, gives a detailed analysis of progress and challenges towards achieving the 90–90–90 targets. The targets were launched in 2014 to accelerate progress so that, by 2020, 90% of all people living with HIV know their HIV status, 90% of all people with diagnosed HIV are accessing sustained antiretroviral therapy and 90% of all people accessing antiretroviral therapy are virally suppressed.
The report shows that in 2016 more than two thirds (70%) of people living with HIV now know their HIV status. Of the people who know their status, 77% were accessing treatment, and of the people accessing treatment, 82% were virally supressed, protecting their health and helping to prevent transmission of the virus.
Eastern and southern Africa, western and central Europe and North America and Latin America are on track to reach the 90–90–90 targets by 2020. In eastern and southern Africa, 76% of people living with HIV know their HIV status, 79% of people who know their HIV-positive status have access to antiretroviral therapy and 83% of people who are on treatment have undetectable levels of HIV—this equates to 50% of all people living with HIV in eastern and southern Africa with viral suppression. The Caribbean and Asia and the Pacific can also reach the 90–90–90 targets if programmes are further accelerated.
Seven countries have already achieved the 90–90–90 targets—Botswana, Cambodia, Denmark, Iceland, Singapore, Sweden and the United Kingdom of Great Britain and Northern Ireland—and many more are close to achieving it.
“Ending AIDS is possible - it is a shared engagement and aspiration. One that cities can lead while promoting inclusive societies for all,” said Anne Hidalgo, Mayor of Paris.
The most significant impact of 90–90–90 scale-up has been in reducing AIDS-related deaths, which have been reduced by almost half in the past 10 years. As a result, life expectancy has increased significantly in the most affected countries. In eastern and southern Africa, life expectancy increased by nearly 10 years from 2006 to 2016.
“Communities and families are thriving as AIDS is being pushed back,” said Mr Sidibé. “As we bring the epidemic under control, health outcomes are improving and nations are becoming stronger.”
90-90-90: more work to do
Progress against the 90–90–90 targets has, however, been poor in the Middle East and North Africa and in eastern Europe and central Asia, where AIDS-related deaths have risen by 48% and 38%, respectively. There are exceptions within these regions showing that when concerted efforts are made, results happen. For example, Algeria has increased HIV treatment access from 24% in 2010 to 76% in 2016, Morocco from 16% in 2010 to 48% in 2016 and Belarus from 29% in 2010 to 45% in 2016.
Globally, progress has been significant, but there is still more work to do. Around 30% of people living with HIV still do not know their HIV status, 17.1 million people living with HIV do not have access to antiretroviral therapy and more than half of all people living with HIV are not virally suppressed.
Eliminating new HIV infections among children
Global solidarity to stop new HIV infections among children has produced results. Around 76% of pregnant women living with HIV had access to antiretroviral medicines in 2016, up from 47% in 2010. New HIV infections among children globally have halved, from 300 000 [230 000–370 000] in 2010 to 160 000 [100 000–220 000] in 2016. Five-high burden countries—Botswana, Namibia, South Africa, Swaziland and Uganda—have already met the milestone of diagnosing and providing lifelong antiretroviral therapy to 95% of pregnant and breastfeeding women living with HIV.
New HIV infections are declining, but not fast enough
The report also shows that, globally, new HIV infections are declining, but not at the pace needed to meet global targets. Globally, new HIV infections declined by 16% from 2010 to 2016, to 1.8 million [1.6 million–2.1 million]. Declines were estimated in 69 countries, in the majority of which treatment scale-up has been implemented alongside an increase in the availability of combination HIV prevention services and in some countries condom use. However, alarming increases have been seen in new HIV infections in eastern Europe and central Asia.
Tuberculosis
Major gains in the global response to tuberculosis and HIV led to a 33% decline in tuberculosis deaths among people living with HIV. As of 2015, only 11% of the 10.4 million cases of tuberculosis globally were among people living with HIV. However, nearly 60% of tuberculosis cases among people living with HIV were not diagnosed or treated.
Community health workers needed
Ending AIDS shows that providing services closer to where people live and work will be a key factor in ending the AIDS epidemic. UNAIDS is championing an initiative recently backed by the African Union to recruit and train 2 million community health workers in Africa to further bolster the capacity of health systems to deliver health-care services across the region.
“When health services reach the doorsteps, the health of families and communities is transformed,” said Mr Sidibé. “Community health workers will become the backbone of strong and resilient health systems across Africa.”
"I am not alone living with HIV, there are millions of us and we are determined to put an end to AIDS," said Christine Kafando, community health worker and founder of Association Espoir pour Demain. "We have the will to do it and must continue our concerted efforts."
WHAT’S OFF TRACK?
Treatment for children living with HIV
Only 43% of children living with HIV have access to antiretroviral therapy, compared to 54% of adults. Ending AIDS also reveals that as many as two thirds of children under two years old are diagnosed late and start treatment with advanced immunodeficiency, resulting in a high mortality rate for children of this age group. More action is needed to diagnose and treat children living with HIV.
Young people are lagging behind
Young people (15–24 years) are lagging behind on multiple fronts—knowledge of HIV, HIV testing, treatment and prevention. Young people continue to be at great risk of HIV infection, especially young women in sub-Saharan Africa. New HIV infections among young women in sub-Saharan Africa are 44% higher than among young men of their age in the region. Around 610 000 new HIV infections occurred among young people aged 15–24 years; 59% of those new infections occurred among young women age 15–24 years.
In Malawi, Zambia and Zimbabwe, half of young people do not know their status and more than half do not have access to HIV treatment. Only 36% of young men and 30% of young women in sub-Saharan Africa had a basic knowledge of how to protect themselves from HIV. Population-based HIV Impact Assessments (PHIAs) conducted in Malawi, Zambia and Zimbabwe, and supported by the United States President’s Emergency Plan for AIDS Relief, found that less than 50% of young people living with HIV were aware of their HIV status, compared to 78% of adults aged 35–59 years.
Men not being reached
The report reveals that less than 50% of young men know how to protect themselves from HIV infection, that men are much less likely to know their HIV status or start treatment than women and that less than 50% of men living with HIV are accessing antiretroviral therapy. Many men who are diagnosed with HIV are diagnosed late and start treatment only when they fall ill, making them much more likely to die of AIDS-related illnesses than women. Deaths from AIDS-related illnesses were 27% lower among women than among men.
Key populations
Outside of sub-Saharan Africa, key populations and their sexual partners accounted for 80% of new HIV infections in 2015 and even in sub-Saharan Africa key populations account for 25% of new HIV infections. The report outlines that efforts to reach key populations with integrated HIV services are essential and that a combination approach is needed that includes harm reduction services.
Regions off track
Eastern Europe and central Asia is the only region in the world where new HIV infections and AIDS-related deaths are both rising. New HIV infections increased from 120 000 [100 000–130 000] in 2010 to 190 000 [160 000–220 000] in 2016. People who inject drugs accounted for 42% of new HIV infections in the region. In the Russian Federation, newly reported cases of HIV increased by 75% from 2010 to 2016. Several other countries in the region—including Albania, Armenia and Kazakhstan—also have rapidly growing epidemics.
Even though access to HIV treatment in eastern Europe and central Asia has more than doubled in the past six years, still only 28% of people living with HIV have access to antiretroviral therapy, despite two out of three people living with HIV knowing their HIV status. AIDS-related deaths have increased by 38%.
In the Middle East and North Africa, just over half of people living with HIV knew their HIV status, with less than half of those on HIV treatment. Only one out of five people living with HIV was virally suppressed.
UNAIDS has been working with Doctors Without Borders and the African Union on a catch-up plan for western and central Africa, which is lagging far behind the rest of the continent. Only 42% of the 6.1 million people living with HIV in the region knew their HIV status, just 35% were accessing HIV treatment and only one in four people living with HIV were virally suppressed in 2016.
“I would like to reiterate our support for the catch-up plan for western and central Africa, launched by UNAIDS and now joined by partners. The adoption of this plan by the heads of state of the African Union is an essential step for mobilization and the efficient implementation of this plan by the countries in the region.” said Michèle Boccoz, French AIDS Ambassador.
Resources for the AIDS response continue to flatline
Resources for the AIDS response remain flat. At the end of 2016, around US$ 19 billion was available in low- and middle-income countries, with domestic resources accounting for 57% of the global total. An estimated US$ 26 billion will be needed for the global response to HIV by 2020.
“We are maximizing the use of every dollar available, but we are still US$ 7 billion short,” said Mr Sidibé. “With more international assistance, increased domestic funding, innovative financing and effective programming can end the AIDS epidemic by 2030.”
|
In 2016 an estimated: 19.5 million people were accessing antiretroviral therapy 36.7 million [30.8 million–42.9 million] people globally were living with HIV 1.8 million [1.6 million–2.1 million] people became newly infected with HIV 1.0 million [830 000–1.2 million] people died from AIDS-related illnesses |
Ending AIDS: progress towards the 90–90–90 targets can be downloaded from unaids.org. UNAIDS is the global leader and repository of AIDS-related programme data. The full data set can be accessed at http://aidsinfo.unaids.org/
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Press centre
Download the printable version (PDF)
Documents
UNAIDS DATA 2017
20 July 2017
UNAIDS has collected and published information on the state of the world’s HIV epidemic for the past 20 years. This information has shaped and guided the development of the response to HIV in regions, countries and cities worldwide. This edition of UNAIDS data contains the highlights of the very latest data on the world’s response to HIV, consolidating a small part of the huge volume of data collected, analysed and refined by UNAIDS over the years.
Related
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
UNAIDS data 2024
02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
Domestic revenues, debt relief and development aid: Transformative pathways for ending AIDS by 2030, Report on Western and Central Africa
18 September 2024
Domestic revenues, debt relief and development aid: Transformative pathways for ending AIDS by 2030, Report on Eastern and Southern Africa
18 September 2024
UNAIDS information/guidance note on the mpox response
30 August 2024
Related
UNAIDS data 2024
02 December 2024
Slide deck - 2024 global AIDS update
22 July 2024
Core epidemiology slides
22 July 2024
Related
UNAIDS data 2024
02 December 2024
Slide deck - 2024 global AIDS update
22 July 2024
Core epidemiology slides
22 July 2024


Feature Story
Accurate and credible UNAIDS data on the HIV epidemic: the cornerstone of the AIDS response
10 July 2017
10 July 2017 10 July 2017Once a year, UNAIDS releases its estimates on the state of the worldwide HIV epidemic. Since the data can literally affect life and death decisions on access to services for treatment and prevention—and are used to decide how to spend billions of dollars a year—they need to be as accurate as possible and be regarded as credible by everyone who uses the information.
How we collect and interpret HIV data has huge consequences—a pregnant woman visiting an antenatal clinic can help calculate the size of the country’s HIV epidemic, can help shape national policies for the response to HIV and can influence the size of grants to respond to HIV from the Global Fund to Fight AIDS, Tuberculosis and Malaria, the United States President’s Emergency Plan for AIDS Relief and others.
So, how do we do it?
Collecting data on the ground
We don’t count people. We can’t—many people who are living with HIV don’t know that they are, so can’t be counted. And everyone in a country can’t be tested every year to calculate the number of people living with HIV. Instead, we make estimates.
The data that are published in our reports, quoted in speeches and used by governments around the world to plan and implement their AIDS responses originate on the ground, in a clinic, in a hospital or anywhere else that people living with HIV access, or need, HIV services.
Take the example of a pregnant women visiting an antenatal clinic as part of her routine antenatal care. She will be offered an HIV test, which will show her to be either HIV-positive or HIV-negative. An HIV-positive result will, of course, open up for the individual mother the range of prevention of mother-to-child transmission of HIV services available to keep her well and her baby HIV-free, but the result, whether negative or positive, will also be used to determine the wider impact of services and the success of country programmes.
Some countries operate a so-called sentinel survey system, in which a network of reporting sites collect data. If the clinic is one of these, a sample of blood will be anonymized and collected with results from the other sentinel sites, resulting in a large set of data to estimate trends from the sentinel sites over time.
In other countries, data from all women who are being tested routinely at all antenatal care sites are used to estimate HIV prevalence. Her test result will be recorded and passed on to the country’s national-level HIV reporting agency.
Data from antenatal clinics, when combined with information from broader, but less frequently collected, population-based surveys, are the basis for HIV data collection in countries where HIV has spread to the general population.
For countries that have HIV epidemics mainly confined to key populations, data from HIV prevalence studies among those key populations are most often used. These prevalence studies are combined with the estimated number of people in those key populations—an estimate that is difficult to make, given that behaviours of key populations are outlawed in many countries.
In countries in which doctors are required to report cases of HIV, and if those data are reliable, those direct counts are used to estimate the epidemic. An increasing number of countries are setting up systems that use reported cases of HIV diagnoses.
Survey types
Population-based survey: a survey that is conducted in a random selection of households in a country. The survey is designed to be representative of all people in the country.
HIV prevalence study: a study of a specific population that collects blood samples from the population to determine how many people in that population are living with HIV. Typically, the results of that test are provided to the survey respondent.
Number crunching
Once a year, the country’s reporting agency will, helped by UNAIDS and partners, make estimates of the number of people living with HIV, the number of people on HIV treatment, the number of new HIV infections, etc., using software called Spectrum, which uses sophisticated calculations to model the estimates.
For estimates relating to children, a whole range of information, such as fertility rates, age distributions of fertility and the number of women in the country aged 15–49, is taken into account when computing the final numbers.
Estimates for different populations and age groups are calculated by Spectrum, taking into account different types of demographic and other data, building up a comprehensive picture of the country’s HIV epidemic.
The Spectrum estimates are sent to UNAIDS at the same time as the collection of the annual Global AIDS Monitoring reporting on the response to the HIV epidemic in the country. UNAIDS compiles and validates all the Spectrum files and uses the country-level data to make global estimates of the HIV epidemic and response.
UNAIDS publishes estimates for all countries with populations greater than a quarter of a million people. For the few countries of that size that do not develop Spectrum estimates, UNAIDS develops its own data, based on the best available information.
Ranges are important
In 2015, there were 36.7 million [34.0 million–39.8 million] people living with HIV in the world. The numbers in the brackets are ranges—that is, we are confident that the number of people living with HIV is somewhere within the range, but can’t say for sure what the definite number is.
All UNAIDS data have such ranges, but why can’t we be more accurate? UNAIDS data are estimates, which vary in their accuracy, depending on several factors. The size of sample taken for the estimate affects the range—a large sample means a small estimate range, and vice versa; if a population-based survey is conducted in a country, the estimate range will be smaller; and the number of assumptions made for an estimate has an impact on how narrow the range will be.
If it’s found to be wrong, it’s fixed
UNAIDS’ models are regularly updated in response to new information. For example, this year’s data will show a slight rise in the reported number of children becoming infected with HIV. This isn’t a real rise in young children acquiring HIV, but an adjustment in our knowledge of how infections occur in real life—in fact, once we apply this updated knowledge to previous years, we see that the number of new HIV infections among infants was higher then too.
Our new knowledge shows us that, after childbirth, higher numbers of women who are breastfeeding are becoming infected with HIV and hence passing the virus on to their children. Models had not fully captured the length of time for which women breastfed and were therefore at risk of passing on the virus through their milk if they became infected with HIV. With the model adapted to take into account women breastfeeding for longer than one year, the number of infants contracting HIV increased slightly for all years since the start of the epidemic.
Because of such finetuning, estimates from one year can’t be compared with estimates from a previous year. When UNAIDS publishes its yearly data, we revise all previous years’ estimates, taking into account the revised methodology. For example, the estimate published in 2006 for the worldwide number of people living with HIV in 2005 was 38.6 million—this was before we had incorporated national household surveys into estimates. By 2016, with the additional information from surveys, the number for 2005 had been revised to 31.8 million. Likewise, the estimate for AIDS-related deaths in 2005 was 2.8 million, which, by 2016, had been revised down to 2.0 million in 2005.
This finetuning has steadily improved the accuracy of our estimates, with the result that recent revisions are becoming smaller—the estimated number of people living with HIV in 2013 made in 2014 was 35.0 million, not far off the current estimates of 35.2 million.