New developments on HIV viral load tests




HIV trials


22 July 2015
22 July 2015 22 July 2015Innovation in HIV diagnostics is urgently needed if the world hopes to achieve the 90–90–90 target for access to antiretroviral therapy, leading scientific experts advised this week. The call for intensified effort and innovation on HIV diagnostics occurred during two sessions at the 8th International AIDS Society Conference on HIV Pathogenesis, Treatment and Prevention, held in Vancouver, Canada.
“It is clear that we can’t accept business as usual when it comes to HIV diagnostics,” said UNAIDS Deputy Executive Director Luiz Loures, who moderated a special satellite session on enhancing diagnostic access. “We must do things differently if we are to reach the 90–90–90 target.”
Global experts focused on three key diagnostic challenges: ensuring timely diagnosis of HIV among children, rapidly increasing knowledge of HIV status among adults living with HIV and scaling up essential viral load testing. These three focus areas are key priorities for the Diagnostics Access Initiative, a multi-stakeholder global initiative that aims to fully leverage the potential of laboratory medicine to lay the groundwork to end the AIDS epidemic as a public health threat.
Diagnosing children living with HIV
Unlike adults, who can be diagnosed with HIV through a simple antibody test, very young children require more expensive molecular tests, which use centralized laboratories that are remote from clinical sites. This creates substantial delays in diagnosing HIV-exposed children and also increases both costs and the risks that specimens or results will be lost. Even when early infant diagnostic services are available, many HIV-exposed children only receive their HIV test results after the time when peak mortality occurs, at six to eight weeks old, according to Trevor Peter, of the Clinton Health Access Initiative (CHAI).
Relatively simple, point-of-care diagnostic tests for early infant diagnosis are now emerging, Mr Peter reported, and these will need to be rapidly scaled up. In addition, mobile health technologies have the potential to reduce delays in the communication of test results and help ensure that test results for HIV-exposed children are actually received at the clinical site. At the Vancouver conference, UNAIDS and its partners in the Diagnostics Access Initiative announced with Roche Diagnostics a 35% decline in the global price for early infant diagnostic testing.
Ensuring 90% knowledge of HIV status among adolescents and adults living with HIV
UNAIDS sponsored a separate session at the conference on democratizing HIV testing to reach the 90–90–90 target. Joseph Amon of Human Rights Watch advised that all people should feel empowered to choose where, when and how they want to be tested for HIV. Consistent with this human rights approach, there is growing interest in HIV self-testing tools.
New international guidelines on HIV testing services, launched by the World Health Organization (WHO) in Vancouver this week, indicate that WHO envisages widespread access to self-testing as an important component of a comprehensive HIV testing effort. Several countries in different regions currently allow HIV self-testing, but most countries have yet to adapt their laws and regulatory frameworks to permit it.
The new WHO guidelines on HIV self-testing emphasize the importance of moving testing access closer to communities. In particular, the new guidelines recommend steps to enable lay workers to administer HIV tests. Results from the Sustainable East Africa Research for Community Health (SEARCH) trial in more than 30 rural communities in Kenya and Uganda indicate that population-level knowledge of HIV status approaching or exceeding 90% can be achieved through community-owned, multidisease testing campaigns.
Presenting modelling work, John Stover of Avenir Health said that 90% knowledge of HIV status is achievable more broadly through a strategic combination of testing strategies, such as provider-initiated testing in diverse health settings, outreach to key populations, fixed centres for HIV testing and counselling, and various community-based approaches, such as HIV self-testing, mobile testing and door-to-door, home-based efforts.
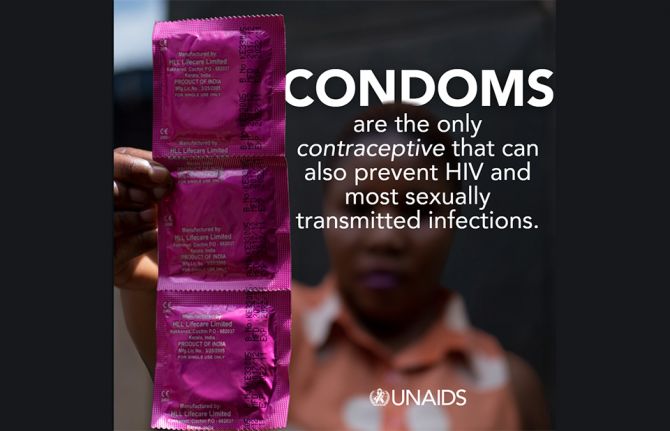
Ensuring universal access to viral load testing
Conference participants also heard urgent calls to expand access to viral load testing. Not only is access to viral load testing essential for monitoring the 90-90-90 target, but viral load testing is an essential clinical tool to detect early treatment failure and permit intervention to improve treatment adherence. However, projections by CHAI indicate that current trends in the uptake of viral load testing are insufficient to ensure achievement of the 90–90–90 target.
During the diagnostics-focused sessions, several ways forward were suggested to close the viral load testing gap. Partners in the Diagnostics Access Initiative, along with the Government of South Africa, last year concluded an agreement with Roche Diagnostics to reduce the price of viral load testing by 40% worldwide. In addition, steps need to be taken to maximize the effective use of the viral load platforms that presently exist, as many viral load technologies are severely under-utilized at present.
13 April 2015
The report is divided into an overview section that articulates the views of the Chair of the Scientific Expert Panel on the top 10 biomedical research advances in 2014 and five important research findings anticipated in 2015. Thereafter, the report provides brief summaries written almost entirely by Scientific Expert Panel members. The topics are divided into three main categories, advances in the treatment of HIV and comorbidities; advances in HIV prevention; and advances in HIV pathogenesis, diagnostics and cure. Linked to each summary is a bibliography that provides a list of key articles for further reading.
01 July 2024
01 February 2024
01 February 2024
01 February 2024
17 January 2024

23 January 2023
01 April 2015
This document is intended for epidemiologists, statisticians and laboratory technicians responsible for the use of HIV incidence assays for surveillance and epidemic monitoring purposes. People that are not technical experts in this field may prefer to first read the UNAIDS/WHO Working Group on Global HIV/AIDS and STI Surveillance published guidelines on When and How to Use Assays for Recent Infection to Estimate HIV Incidence at a Population Level for a basic introduction to this topic.
17 December 2024
17 December 2024
16 December 2024
02 December 2024

19 August 2024
22 July 2024
22 July 2024


21 November 2014
21 November 2014 21 November 2014Results from a major clinical trial released on 17 November provide further evidence that triple antiretroviral medicine combinations are more effective than single-medicine regimens in preventing mother-to-child transmission of HIV. Named PROMISE—Promoting Maternal and Infant Survival Everywhere—the trial was conducted in India, Malawi, South Africa, United Republic of Tanzania, Zambia and Zimbabwe.
The findings show that pregnant women with a CD4 count of 350 cells/mm3 or higher receiving a protease inhibitor containing triple antiretroviral regimen were 70% less likely to transmit HIV to their infants than women receiving a single-medicine regime of zidovudine.
Overall transmission rates, measured at two weeks of age, were low across the study, estimated at 0.5% and 0.6% among the mothers using each of the two triple-medicine regimens studied and 1.8% with the single-medicine regimen.
As expected with multiple medicine regimens, the study also revealed more side-effects in women taking the triple combination. While overall the number of women and babies experiencing side-effects was low, there was a higher incidence of maternal liver toxicity, low-birth weight and preterm deliveries with the triple regimen. According to the researchers, balancing the lower risk of HIV infection being passed from mother to baby with the increased rate of side-effects, the triple antiretroviral combination is the more favourable option.
These results confirm the WHO guidelines for the prevention of mother-to-child transmission and are reassuring for the many developing countries that are changing from single (WHO option A) to triple regimens (WHO option B/B+). UNAIDS supports rigorous research, such as the PROMISE trial, which was designed to inform policy and guidelines to enhance the global response to eliminate HIV infection among children.
Since 2011, UNAIDS and partners have been working with countries to reduce new HIV infections among children and strengthen maternal health through the Global Plan towards the elimination of new HIV infections among children and keeping their mother alive, which covers the 22 countries in which 90% of newborn infections occur. By the end of 2013, the participating countries had already registered a 43% reduction in new HIV infections, and eight have reduced new infections by 50% or more. For the first time, all the 22 countries have now adopted the option B triple medicine regimen for the prevention of mother-to-child transmission of HIV.
“The outcome of the PROMISE trial provides clear evidence for countries that are still implementing option A to move as rapidly as possible to option B/B+.”

27 February 2025





Independent monitoring bodies of two PrEP trials recommend offering antiretroviral therapy to all study participants
GENEVA, 29 October 2014—UNAIDS warmly welcomes strong indications from two ongoing trials of the effectiveness of antiretroviral therapy in preventing new HIV infections among men who have sex with men.
The IPERGAY trial, conducted by the ANRS, the French National Agency for Research on AIDS and Viral Hepatitis, enrolled 400 men who have sex with men in France to establish the efficacy of taking the antiretroviral combination of tenofovir/emtricitabine as pre-exposure prophylaxis (PrEP) before and after sex rather than daily. The data safety and monitoring board for the IPERGAY trial reviewed data for the study and found a “very significant” reduction in the risk of HIV infection in the group of participants using tenofovir/emtricitabine as PrEP compared to the placebo group. The monitoring board subsequently recommended that the placebo group be stopped and that all trial participants should be offered tenofovir/emtricitabine as PrEP.
This announcement follows a recent decision to amend the PROUD study in the United Kingdom. In the PROUD study, the participants were initially placed at random into two groups—one group that used PrEP from the start of the study and another group that was due to receive PrEP after 12 months. However, the independent data monitoring committee found that the effectiveness seen in the trial exceeded the threshold set for trial continuation and recommended that the researchers offer daily PrEP to all study participants immediately.
Neither study is ready to present the full data for review. However, both independent monitoring bodies were clear that the results were so convincing that it would be unethical to allow the participants to continue without receiving PrEP. The final results of the IPERGAY and PROUD trials are expected to be presented in early 2015. Once the results are confirmed, antiretroviral therapy taken as PrEP before and after sex could become an additional HIV prevention option for men who have sex with men.
UNAIDS underlines that no single intervention is completely protective in preventing HIV transmission, which is why UNAIDS advocates strongly for combination HIV prevention. This includes correct and consistent use of condoms, delaying sexual debut, having fewer sexual partners, male circumcision, access to antiretroviral therapy, reducing stigma and discrimination, and the removal of punitive laws.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Download the printable version (PDF)
01 January 2015
The organization leads the global health sector response to the HIV epidemic. As a Cosponsor of UNAIDS, WHO takes the lead on HIV treatment and care and HIV/tuberculosis coinfection, and jointly coordinates work on the elimination of mother-to-child transmission of HIV with the United Nations Children’s Fund (UNICEF).

27 February 2025
30 January 2025

21 January 2025


















22 February 2013
22 February 2013 22 February 2013
Study confirms the urgent need for rapid and wide-scale roll out of antiretroviral therapy to communities which have been most affected by the epidemic.
The full results of a study on the effects of antiretroviral therapy in preventing new HIV infections have been published this week in the journal Science. The study, led by Professor Frank Tanser from the Africa Centre, spanned a seven year period (2004-2011), and followed nearly 17 000 people, the largest ever study completed at a population-level in a rural sub-Saharan African setting.
It was conducted in the sub-district of Hlabisa in the rural Province of KwaZulu-Natal, South Africa. The rolling hills of KwaZulu Natal are perhaps one of the most beautiful places on earth but it is also an area which has been particularly affected by the AIDS epidemic. KwaZulu Natal has one of the highest HIV prevalence rates in the world––one in four people over the age of 15 are living with HIV.
The province of KwaZulu Natal has been widely acknowledged as leading a strong provincial response to HIV. In Hlabisa for example, by mid-2012 the Hlabisa HIV Treatment and Care Programme had rolled-out antiretroviral treatment to more than 20 000 people across the area.
The 16 667 participants enrolled in the Professor Tanser’s study did not have HIV at the start of the trial and were regularly tested on average every two years. By the end of the study period 1 413 people had become infected with HIV. The people who tested HIV positive were offered antiretroviral therapy when they became eligible for treatment under national South African guidelines. Initially, adults with a CD4 count of 200 were offered treatment, this was extended to people with CD4 counts of 350, pregnant women and TB patients by April 2010.
What the study found was that the risk of acquiring HIV declined significantly if a person was living in an area where antiretroviral coverage was highest. For example in the areas where treatment coverage was between 30%-40% of all people living with HIV (which corresponds to about 60% of people eligible for treatment under current guidelines) people were nearly 40% less likely to become infected with HIV than in communities where coverage was much lower, at less than 10%. These results are yet further confirmation of the enormous impact antiretroviral therapy could have on morbidity, mortality and new HIV infections if access to treatment was scaled up to full impact levels in populations most affected by HIV.
This large scale population based study, the first in a hyper epidemic region in Africa, delivers powerful evidence that treatment is prevention and is an essential part of our combination prevention tool kit.
Bernhard Schwartlander, Director of Evidence, Innovation and Policy at UNAIDS
"This study is extremely significant. It is another piece in the puzzle that shows how treatment keeps people healthy and productive, and at the same time significantly reduces the likelihood to transmit the virus,” said Bernhard Schwartlander, Director of Evidence, Innovation and Policy at UNAIDS. “This large scale population based study, the first in a hyper epidemic region in Africa, delivers powerful evidence that treatment is prevention and is an essential part of our combination prevention tool kit.”
Concerns relating to the uptake of testing and treatment, retention, adherence, the development of drug resistance and other factors such as the capacity of health systems to deliver antiretroviral therapy have been long-debated, particularly since the findings of the HPTN052 trial were announced in 2011. The HPTN052 trial gave rise to great optimism amongst the HIV community––it showed that if a person living with HIV adheres to an effective antiretroviral regimen the risk of transmitting the virus to their uninfected sexual partner could be reduced by 96%. However larger, population based studies were yet to confirm how these findings apply to community settings.
While it is not unexpected that such a large scale and longer term population level study would pack the percentage punch of the HPTN052 trial, what it lacked in percentage points it made up for in the sheer scale and depth of the trial. What it has done is to bring us one step closer to finding out the true potential of antiretroviral therapy and the enormous impact it could have on preventing new HIV infections in real settings where HIV is part of daily life.
It has given further confirmation of the urgent need for rapid and wide-scale roll out of antiretroviral therapy to communities which have been most affected by the epidemic. And it has given yet another strong reason for countries to keep their commitments and meet the targets set out in the 2011 United Nations General Assembly Political Declaration on HIV/AIDS––to scale up access to treatment to reach 15 million people by 2015––and to halve the numbers of sexually transmitted HIV infections by 2015.