PLHIV



Feature Story
Community health workers strengthen HIV and COVID-19 responses
02 December 2021
02 December 2021 02 December 2021In 2001, Micheline Léon felt unwell. The then 33-year-old mother of three journeyed from her home in the small town of Corporand in central Haiti to a clinic in Cange. There she was diagnosed with HIV and tuberculosis.
Fortunately, three years earlier an organization called Zanmi Lasante—Haitian Creole for Partners in Health—had launched the HIV Equity Initiative. (Zanmi Lasante is the sister organization of the United States-based nonprofit health-care group Partners in Health.) This was one of the first projects in the world to effectively deliver antiretroviral therapy in poor, rural settings.
Twenty years later, Ms Léon is one of 2000 community health workers called accompagnateurs in the Zanmi Lasante network. Multiskilled teams of accompagnateurs are the link between patients and health facilities. They are also part of all HIV Equity Initiative discussions regarding patient care, treatment and social support.
Community health workers live in the areas where they work. They help to ensure that patients recover and stay healthy. Their main roles include medicine distribution and home visits, as well as linking people to care. They accompany patients to clinics and track those who have missed appointments. During the COVID-19 pandemic, the accompagnateurs were key to Zanmi Lasante’s care and treatment work. The home-based care and contact tracing skills refined in response to HIV are now being used for COVID-19.
Zanmi Lasante has a holistic approach to care that includes social services such as providing accommodation, food and transport. Community health workers help to coordinate all the support needed. They also serve the wider community by running educational campaigns on topics such as mental health and sexually transmitted infections.
Critically, the accompagnateurs empower and inspire people to take charge of their own health. Ms Léon is a role model within reach. Since starting treatment she has stayed adherent to it and her HIV viral load has remained undetectable since she began receiving viral load tests in 2017. She owns a small fruit and poultry business and sometimes spends time in Port au Prince, where she has a new grandson. She takes part in various group activities at the Zanmi Lasante site in Cange, including support groups, viral load classes and mothers’ clubs.
“The psychosocial support I received from Zanmi Lasante made me realize that my diagnosis was not a death sentence and I could go on and live a healthy and fulfilled life,” Ms Léon said.
Another stalwart Haitian HIV programme employs a community health approach. GHESKIO, the Haitian Study Group on Kaposi’s Sarcoma and Opportunistic Infections, was founded in 1982, the year before HIV was formally discovered. It is the world’s oldest HIV organization and has conducted research and provided clinical care over the past four decades.
GHESKIO has leveraged a community-based model to help Haiti respond to HIV and other public health crises. When the COVID-19 pandemic reached the country in March 2020, GHESKIO reinforced an existing programme—Distribution of ART in the Community—to ensure that clients living with HIV were provided with a three-month supply of medication. From a small room at the National Solidarity Association (ASON), a team packages medicines into plastic bags and pours over their client list. If a person is unable to come for their medicines, they’ll receive a home delivery.
GHESKIO also strengthened training activities for their multiskilled community health workers. In this way they provided social support for patients as well as home care for cases that did not require hospitalization.
“Our Community Unit played an essential role in the acceptance of new COVID-19 treatment centres in the impoverished, crowded slums,” said GHESKIO’s Program Coordinator, Patrice Joseph. “In collaboration with the Ministry of Health, we have strengthened contact tracing, case investigation and outbreak management for COVID-19.”
One of the newest community health workers is CV, a 35-year-old mother of three from Village de Dieu, a slum south of Port au Prince. She herself survived COVID-19. When she began feeling ill a community health worker accompanied her to get tested. Following five days at GHESKIO’s COVID-19 hospital, a community team conducted home visits to ensure her full recovery.
Now she works as a greeter at GHESKIO. She is also a GHESKIO community health agent, encouraging patients to come to scheduled visits. CV supports community sensitization around COVID-19 prevention by promoting sanitation and educating people about the importance of COVID-19 vaccination.
“I don’t take one day for granted,” she said.
Region/country
Related




Feature Story
Supporting people living with HIV with income generation in the Central African Republic
17 November 2021
17 November 2021 17 November 2021On 11 November, a project to support the empowerment of nearly 400 people living with HIV through training and involvement in agropastoral activities was launched in the seventh arrondissement of Bangui, Central African Republic.
According to Joseph Tagbale, the Mayor of the seventh arrondissement, “This project is timely and comes as a breath of fresh air, as people living with HIV have paid a heavy price during the COVID-19 pandemic, firstly because of their high risk of infection due to their weak immune systems and secondly because of the collapse of their means of subsistence due to repeated confinements.”
The Multi-Partner Trust Fund granted the UNAIDS Country Office for the Central African Republic US$ 150 000 to support activities for people living with HIV in the context of COVID-19. These activities were chosen in collaboration with the Comité National de Lutte Contre le Sida (CLNS), the Ministry of Health and the Central African Network of People Living with HIV (RECAPEV) and will be implemented by the United Nations Food and Agriculture Organization and the international nongovernmental organization Solidarité pour la Paix et le Développement Intégré.
The activities consist of agropastoral activities (small-scale livestock farming and other farming activities), the production of face masks and income-generating activities, such as sewing, catering and the sale of soap and kitchen utensils. All these activities will enable people living with HIV to sustainably meet their needs and better adhere to their antiretroviral therapy, since due to the COVID-19 pandemic many people living with HIV have stopped taking their treatment because of problems in accessing food. “COVID-19 has destroyed all our progress in adherence to treatment, and people living with HIV have a lot of difficulty feeding themselves, as many are unemployed,” said Bienvenu Gazalima, the National Coordinator of RECAPEV.
The income-generating activities will be supported in four arrondissements of Bangui and in two surrounding communes, Bimbo and Bégoua, which were selected because they have large numbers of people on antiretroviral therapy.
Throughout the project, peer educators will educate people living with HIV on treatment adherence and other health issues, such as COVID-19 prevention and vaccination. Emphasis will be placed on involving women in the activities. “I am delighted that women living with HIV are so strongly integrated in this project, because it is they who have paid the highest price during this crisis,” said Marcelline Seremandji, adviser to civil society associations at CLNS.
“In the Central African Republic we are witnessing how structural inequalities and lack of income have direct impacts on health and HIV outcomes. The lower someone’s social and economic status, the poorer their health is likely to be. Addressing food insecurity and malnutrition, keeping adults earning an income and keeping children in school helps to ensure the efficacy of HIV treatment,” said Marie Engel, the Director, a.i., of the UNAIDS Country Office for the Central African Republic.
Region/country
Related

Press Statement
UNAIDS welcomes New Zealand’s decision to lift travel restrictions for people living with HIV
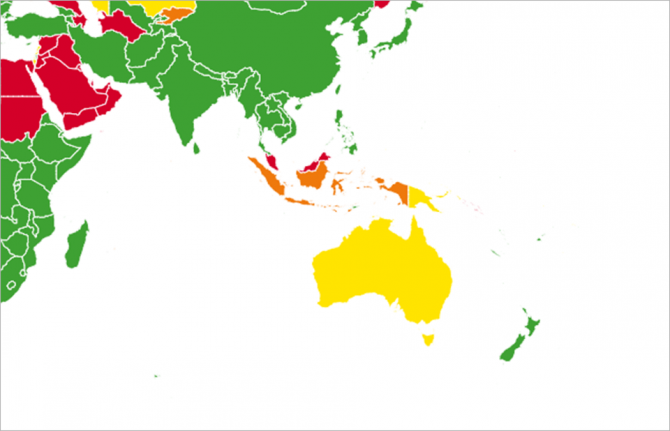
25 October 2021 25 October 2021GENEVA, 25 October 2021—UNAIDS welcomes the announcement by New Zealand that it has removed all travel restrictions for people living with HIV. The recent decision by Immigration New Zealand to remove HIV from the list of medical conditions deemed likely to impose significant costs or demands on New Zealand’s health services means that the blanket ban for people living with HIV to get a resident visa has officially been removed.
“I commend New Zealand for taking this important step and hope that it will encourage other countries to remove all travel restrictions and other policies that discriminate against people living with HIV,” said UNAIDS Executive Director, Winnie Byanyima.
Legislation, policies and practices that prohibit the movement of people living with HIV are discriminatory and frequently limit their opportunity to travel, work and study abroad. UNAIDS advocates for the right to freedom of movement and non-discrimination to end the inequalities faced by people living with HIV. There is no evidence that restrictions on the entry, stay or residence of people living with HIV protect public health.
With the removal of New Zealand’s restrictions, UNAIDS counts 46 countries, territories and areas that continue to impose some form of restriction on the entry, stay and residence of people living with HIV based on their HIV status.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Region/country


Feature Story
Adapting to keep people living with HIV taking their treatment in the Central African Republic
31 October 2021
31 October 2021 31 October 2021To counter the low level of people living with HIV in Central African Republic (CAR) on treatment, the country has been testing new treatment approaches.
One is distributing up to 6 months of medicine, known as multi-month dispensing. The other is community ARV dispensation. CAR’s 2021-2025 National HIV Strategic Plan, identified these differentiated approaches at the community and hospital level and has been trying it out.
In the capital, Bangui, four pilots opened and 15 sites will progressively offer MMD (multi-month dispensing), health check-ups and community outreach thanks to funding from the Global Fund. This follows on the success of community-based treatment groups (CAGs) introduced by the Ministry of Public Health and Population and the National AIDS Control Council (CNLS) in 2015, with the support of the NGO Médecins Sans Frontières.
Certain community members deliver antiretroviral treatment to people living with HIV, especially in rural or conflict-stricken areas. Results showed that treatment intake was much more regular and people living with HIV had a rate of 75% viral suppression.
In addition, with UNAIDS support under a Luxembourg grant, the country has set up a steering committee to oversee the scale up of differentiated services, developed and validated national guidelines on the provision of differentiated services and two guides on multi month dispensing and the possibility of getting refills in a non-hospital setting.
At the end of October, clinicians, lab technicians, health care providers, community health care workers from the four pilot health centers participated in a workshop to go over the new approaches and guidelines. The CNLS and the country’s Division of Communicable Disease Control (DLMT) were confident adapting to the HIV epidemic in this way was a right step to keep patients on treatment. Currently, less than half of the people living with HIV take life-saving medicine (88,000-100,000 people live with HIV in CAR.)
Dr Marie-Charlotte Banthas from the DLMT said that "differentiated treatment models have demonstrated consistent improvement in patient engagement and retention of care, while freeing up time for the care of people with advanced disease.” She then added, ”It's a model of care for people living with HIV and staff working in the HIV field, a model of life."
These approaches came at the right time considering the lockdowns due to COVID-19, remarked UNAIDS CAR Country Director a.i. Marie Engel.
"With the long projected trajectory of the Covid pandemic, there is an even greater need to adapt the system to reduce service disruptions and not have recent gains in the HIV response stymied,” she said.
Region/country
Related
Documents
Still not welcome — HIV-related travel restrictions
27 June 2019
Mandatory HIV testing and bans on entry, stay and residence based on HIV status not only do not protect public health but undermine HIV prevention and treatment efforts. For millions of people living with HIV around the world, these are repeated violations of their right to privacy, equality and non-discrimination and a constant reminder of HIV-related stigma. In 2016, United Nations Member States agreed to eliminate HIV-related travel restrictions. In 2019, around 48 countries and territories still maintain some form of HIV-related travel restriction.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment
Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment

21 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
UNAIDS data 2024
02 December 2024




Feature Story
Helping Haiti build a sustainable HIV response
11 October 2021
11 October 2021 11 October 2021At the GHESKIO (Groupe Haïtien d'Étude du Sarcome de Kaposi et des Infections Opportunistes) clinic in Port au Prince, Haiti, a young woman learns that she is HIV-positive. Along with counselling, she is offered immediate enrolment into a treatment programme at the facility.
Same-day treatment initiation is among the approaches Haiti has used to turn the tide on its HIV epidemic. HIV prevalence among adults is now 1.9%, down from a high of 3.2% in the mid-1990s. According to government statistics, of the estimated 154 000 people living with HIV, 89% know their status. Ninety-three per cent of diagnosed people are on antiretroviral therapy and 87% of people who are on antiretroviral therapy are virally suppressed. Over the past decade, deaths due to AIDS-related illnesses fell by 63% in the Caribbean country.
These achievements are the result of collaboration between the Government of Haiti, civil society and international development partners.
But they are also due to considerable donor investment. The vast majority of total HIV expenditure in Haiti comes from international sources.
The UNAIDS Country Office for Haiti is currently supporting the United States President’s Emergency Plan for AIDS Relief (PEPFAR) and the Ministry of Public Health and Population to conduct the Sustainability Index and Dashboard (SID) exercise in Haiti. This is a tool completed every two years to sharpen understanding of countries’ sustainability landscapes and inform HIV investment decisions. Through the exercise, stakeholders assess national HIV responses from the point of view of sustainability and across four thematic areas. This is Haiti’s fourth SID.
“The impressive gains Haiti has made over the past decade can be compromised in the future by overreliance on external funding. UNAIDS is pleased to support the Ministry of Public Health and Population along with PEPFAR and the Global Fund to Fight AIDS, Tuberculosis and Malaria through this exercise to build a more sustainable response,” said the UNAIDS Country Director for Haiti, Christian Mouala.
UNAIDS will continue to work together with the national leadership, PEPFAR, the Global Fund to Fight AIDS, Tuberculosis and Malaria, civil society and other key partners of the HIV response to ensure that national interventions are equitable. The focus is on reaching the most vulnerable communities through coordinated programming and implementation and consistent inclusion of people living with HIV and key populations, including in humanitarian contexts.
The Executive Director of the Unit for the Control of Infectious and Transmissible Diseases (UCMIT), Pavel Desrosiers, noted that the SID exercise is crucial to identifying weaknesses in the current HIV response.
According to Hamfrey Sanhokwe, the PEPFAR Coordinator for Haiti, the SID also helps donors, “Measure progress on programmatic and financial sustainability and focus efforts for an optimal HIV national response.”
The optimum participation of all HIV stakeholders is key to the process. “People living with HIV were represented in and contributed to all the thematic meetings during the week and the exchanges were productive,” said Maria Malia Jean, a representative of the Haitian Federation of the Associations of People Living with HIV (AFHIAVIH).
The results of Haiti’s 2021 SID will be finalized and validated by all stakeholders before the end of October. HIV stakeholders will then be able to visualize and focus on areas that need further strengthening, while noting the successes they have worked so hard to achieve.
“Haiti has achieved much progress in the fight against HIV; however, efforts must be sustained and increased to ensure that targets are achieved by 2030,” said the Director-General of the Ministry of Public Health and Population, Lauré Adrien.
Region/country
Related

Update
People living with HIV at higher risk of COVID-19 illness but have lower access to COVID-19 vaccines
11 October 2021
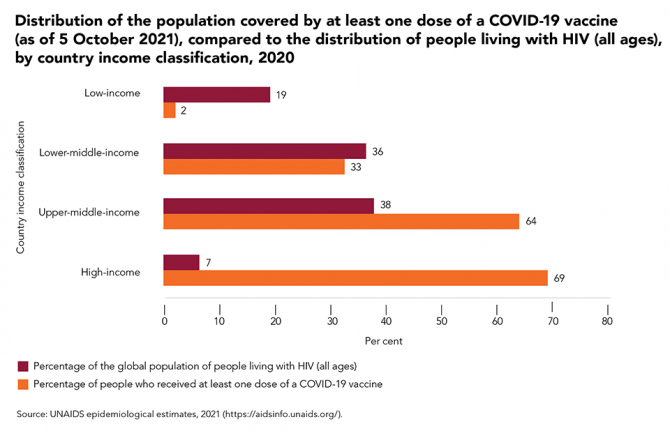
11 October 2021 11 October 2021An increasing body of evidence indicates that people living with HIV who acquire SARS-CoV-2 infection are at heightened risk of requiring hospitalization and having poor clinical outcomes.
Data from the United States of America show that people living with HIV who acquired SARS-CoV-2 infection were much more likely to require hospitalization and suffer severe illness than people who were HIV-negative, while studies from England and South Africa have found that the risk of dying from COVID-19 among people with HIV was double that of the general population. Advanced HIV disease and/or the presence of chronic comorbidities—which tend to be common in people living with HIV—appear to be strongly associated with poor COVID-19 outcomes in people living with HIV.
However, access to COVID-19 vaccines around the world remains exceedingly unequal and unjust. At the beginning of October 2021, there were still low levels of access to vaccines in the low-income and lower-middle-income countries that are home to more than half (55%) of people living with HIV globally.
Our work
Related




Feature Story
Multicountry People Living with HIV Stigma Index 2.0 study launched in Latin America
05 October 2021
05 October 2021 05 October 2021The Latin America and Caribbean region has deep and widespread inequalities and includes countries that are more unequal than those in other regions with similar levels of development. This affects access to health and HIV services, particularly by key populations. Social and structural barriers are important drivers of inequalities.
To understand these social and structural barriers better, Alianza Liderazgo Positivo y Poblaciones Clave (ALEP) is leading the multicountry People Living with HIV Stigma Index 2.0 study in four countries in the region: the Plurinational State of Bolivia, Ecuador, Peru and Nicaragua. Another five similar studies funded by the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) and in coordination with civil society, the United States President’s Emergency Plan for AIDS Relief, Global Fund principal recipients, the United Nations Population Fund and UNAIDS are independently under way in El Salvador, Honduras, Guatemala, Panama and Paraguay.
The results of the joint initiative are expected to strengthen regional and global efforts to eliminate HIV-related stigma and discrimination through community-centred policies and programmes that are informed by evidence.
“For the first time since the first People Living with HIV Stigma Index study in 2008, nine countries in the same region will be conducting the study in coordination and within the same time frame. This is unprecedented and will be instrumental in addressing HIV-related stigma and discrimination both at the country and regional level,” said Rodrigo Pascal, ALEP’s People Living with HIV Stigma Index 2.0 Study Coordinator.
The People Living with HIV Stigma Index 2.0 gathers evidence on how stigma and discrimination impacts the lives of people living with HIV, including key populations. It was developed to be used by and for people living with HIV, including key populations, and was created to support the principle of the greater involvement of people living with HIV, under which networks are empowered to lead the implementation of the study. The study is a first, as it is the first time that networks of people living with HIV have coordinated action with networks of key populations to promote human rights and access to comprehensive and differentiated HIV care in Latin America.
“The motivation I have is to be part of the solution regarding the challenges imposed by stigma and discrimination, which are the main problems we, people living with HIV, are confronting since the beginning of the epidemic,” said HIV activist Gracia Violeta Ross Quiroga, who is coordinating the implementation of the stigma index study in the Plurinational State of Bolivia. “I have hope in this research because it is coming from the community, and such responses have proved to be the most effective in the history of HIV.”
ALEP is an innovative effort that combines the leadership, vision, capacities and strengths of regional networks in the Plurinational State of Bolivia, Colombia, Costa Rica, Ecuador, El Salvador, Guatemala, Honduras, Nicaragua, Panama, Paraguay and Peru. It works in partnership with Country Coordinating Mechanisms where there is a Global Fund programme in place, UNAIDS and the Pan American Health Organization.
“This is a solid example of how peers are contributing to their own communities while tackling key intersecting issues, such as human rights, stigma and discrimination, and other structural barriers. It’s essentially by communities, for communities,” said Guillermo Marquez, the Senior Community Support Adviser for the UNAIDS Regional Support Team for Latin America and the Caribbean.
Watch launch event (in Spanish)
Follow ALEP’s updates on the multi-country Stigma Index 2.0 initiative
Watch launch event (in Spanish)
Region/country




Feature Story
Don’t be silent on gender-based violence
04 October 2021
04 October 2021 04 October 2021Larisa Aleksandrova is a legal expert at the Center for Human Rights and has been protecting the rights of women living with HIV in Tajikistan since 2011.
For the past few months, she has been helping a lawyer to open a criminal case against a man who attacked his wife, Amina Khaidyrova (not her real name), and repeatedly threatened to rape her daughter from her first marriage. The prosecutor's office has so far refused to open the case, considering it a private family matter. According to the prosecutor’s office, if there are only minor injuries, the victim must seek to open a criminal case against the attacker by filing an application to the court by herself. The man is now in hiding and the prosecutor's office continues to refuse to open the case, now claiming that he cannot be found.
Ms Khaidyrova, who is living with HIV, will stop at nothing to get justice. She says that she has nothing to lose and fears for her life and the life of her daughter.
Ms Aleksandrova says that women who have been victims of violence often either do not report the assault to the police or withdraw the allegation, fearing the consequences. She says that women don’t report violence for a variety of reasons—some want to keep their family together, no matter what, others do not want publicity, but the majority are afraid of finding themselves without economic support, since women in Tajikistan are often economically dependent on their husbands.
“In general, women are ready to endure. And women living with HIV are even more willing to endure,” said Ms Aleksandrova.
She emphasized that there were rare cases when women living with HIV have sought help, but fear of disclosure of HIV status, stigma and discrimination, lack of support from family and friends, the vulnerability of people living with HIV because of the criminalization of HIV transmission, legal illiteracy and insecurity prevent women from asserting their rights in court.
Speaking at a training jointly organized by UNAIDS, the United Nations Development Programme and the United Nations Office on Drugs and Crime for 35 representatives of nongovernmental organizations working on human rights and gender-based violence prevention, Ms Aleksandrova presented the legal norms governing the legal status of people living with HIV. She also discussed the criminal legislation of the country on HIV, international and national standards for the protection of women’s rights and sexual and gender-based violence and mechanisms for the protection of women living with HIV who are victims of violence.
The participants analysed cases related to sexual and gender-based violence against women, reviewed and worked out strategies for prosecuting such cases and gave practical advice on strategies for dealing with gender-based violence. According to the participants, such training for nongovernmental organizations in Tajikistan is crucial if they are to reach more women, particularly women living with HIV.
“Community-based monitoring of violations of the rights of people living with HIV and their ability to access confidential HIV services is an important component of community empowerment to speak up and raise questions about the root causes that drive the spread of various forms of violence. These problems can only be resolved if communities are literate in the field of civil and international human rights and are ready to stand up for their rights and seek the proper implementation of the law against domestic violence,” said Nisso Kasymova, the UNAIDS Country Manager for Tajikistan.
Ms Aleksandrova believes that legal literacy is critical, but it is insufficient to solve the problem. She said that if a woman is economically dependent, she will not use her legal knowledge. “I always say that women need to be given confidence in the future, the confidence that they will not be thrown out into the street, that they will be able to protect themselves, they will be supported and they will be able to live on and realize themselves in life.” But you need to start small, she added, “Do not be silent, talk about the problem, demand and defend your right to life, health and economic independence.”
Region/country
Related
 Status of HIV programmes in Tajikistan
Status of HIV programmes in Tajikistan

05 March 2025
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025


Feature Story
The humanitarian activist supporting Venezuelan migrants living with HIV in Brazil
23 August 2021
23 August 2021 23 August 2021Nilsa Hernandez, 62, used to work as an informal greengrocer in Venezuela to help increase her family income and provide for her children, grandchildren and great-grandchildren. As a person living with HIV for 16 years, Nilsa had managed to reduce her viral load to undetectable until everything changed suddenly when the political-economic crisis took hold in Venezuela. Health services were severely affected and people living with HIV gradually lost access to regular care, treatment and medication.
"I went about two years without access to treatment. My body started to feel the consequences and I realized that I needed to do something urgently. It was a live or die situation, and I decided to live!", remembers Nilsa.
Nilsa crossed the border and emigrated to Brazil, where HIV treatment is available to everyone through the public health system. It took her a year to prepare for the journey. In 2018, she arrived in Roraima, the Brazilian state bordering Venezuela, with her partner, who also lived with HIV, and her 12-year-old grandson.
They ended up in the streets after suffering all kinds of discrimination and violence. Thanks to the support of people she met, she finally managed to rent a small house in the outskirts of Rio Branco, the capital of Roraima, and resume her HIV treatment. As soon as she recovered immunity, she had no doubt: it was time to become an activist and create Valientes por la Vida (Brave for Life), a voluntary initiative to support other Venezuelans living with HIV who, like her, arrived in Brazil with scarce resources and little information.
"We are brave because it takes a lot of courage to leave your country, often with only the things we had to hand, in search of treatment and in search of life."
Today, as a humanitarian activist, Nilsa has mobilized a network of other Valientes who joined her to spread the word about the arrival of new Venezuelan migrants in search of HIV treatment.
The COVID-19 pandemic has severely affected this process, especially when the borders between Brazil and Venezuela were closed in March 2020. “The closure made it very difficult for my compatriots to access HIV treatment that could save their lives. With the reopening of the border, we are now putting these services back on track."
According to the 2020 Annual Report on Epidemiology issued by the state of Roraima’s medical authority, in the years 2018 and 2019, a combined total of 1,137 cases of HIV/AIDS were reported in the state. Among the foreign population, migrants from Venezuela represent the most significant number of the combined HIV/AIDS cases for the same period: 383 people.
Just like Nilsa, many of the Venezuelan people living with HIV migrate to Brazil in search of access to HIV treatment that they are no longer able to have in many parts of the country. In this context, UNAIDS established a partnership with UNESCO in December 2020 in a joint, collaborative and intersectoral strategy to grant Venezuelan migrants access to health education, prevention, and health promotion, and to support the responses of Roraima to HIV and COVID-19.
Claudia Velasquez, UNAIDS Representative and Country Director in Brazil, explains that the proposal is to reduce prejudice, stigma and discrimination related to migrants and refugees, and more vulnerable populations, such as sex workers and LGBTQIA+ population, youth and indigenous peoples.
"We want to promote the empowerment of vulnerable populations through the dissemination of information about HIV and the rights of people living with HIV”, says Ms. Velasquez. “Nilsa Hernandez is an example of a humanitarian activist. And people like her, who are Brave for Life, show the enormous impact that civil society's mobilization has on supporting and welcoming people living with HIV and on the efforts to face stigma and discrimination, which enhance the inequalities that prevent us from ending the AIDS pandemic by 2030."
For the future, Nilsa's dream is for Valientes por la Vida to become an international organization, with volunteers dedicated to supporting people living with HIV to have access to treatment and a healthy life. "I also want people to stop seeing us as HIV positive. This creates a horrible stigma that weighs on us all. We are not HIV positive. We are brave and impatient because we are in a hurry to live like everyone else."