PLHIV

Feature Story
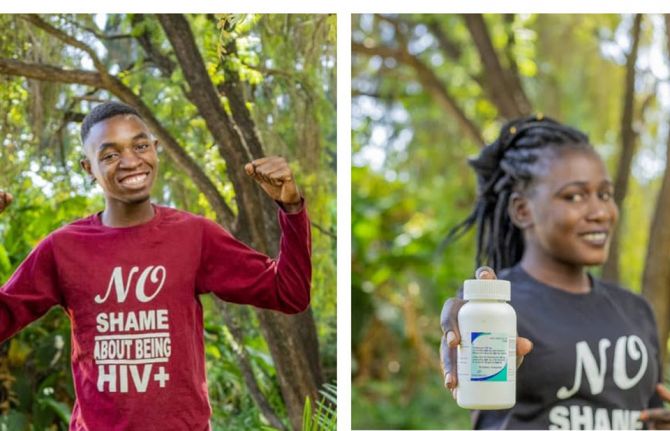
Y+ Global launches COVID-19 fund to support young people living with HIV
05 January 2021
05 January 2021 05 January 2021Communities of people living with HIV have been at the forefront of the community-led response to the COVID-19 pandemic. As part of that response, the Global Network of Young People Living with HIV (Y+ Global), with support from UNAIDS, has launched the Y+ Social Aid Fund for young people living with HIV.
The Y+ Social Aid Fund will be piloted in Nigeria and Malawi, where, with the support of national networks of young people living with HIV ,Y+ Global will offer financial support to young people living with HIV who have been impacted by COVID-19-related restrictions.
“Lockdowns, social instability and treatment interruptions during COVID-19 have further magnified the inequalities that exist in the societies of young people. With grants such as the Y+ Social Aid Fund, young people living with HIV will be able to access basic living essentials that will relieve a portion of the burden on their mental health,” said Igor Kuchin, the Y+ Global Board Chair.
COVID-19 and associated restrictions have had a severe negative impact on the lives of young people living with HIV. Adolescent girls and young women living with HIV are experiencing issues ranging from poor access to menstrual hygiene products to increased need for refuge from gender-based violence while in lockdown. In the 2020 World AIDS Day report, Prevailing against pandemics by putting people at the centre, 27 out of 28 countries surveyed reported that COVID-19 restrictions were impacting antiretroviral therapy initiation for people newly diagnosed with HIV.
“In the context of the COVID-19 pandemic, communities of young people living with HIV are once again leading responses and providing new examples of the solidarity, resilience and innovation that have driven and accelerated the HIV response since the beginning of the HIV pandemic,” said Suki Beavers, Director of the UNAIDS Department for Gender Equality, Human Rights and Community Engagement.
It is hoped that this initial roll-out to provide financial assistance to the most vulnerable young people living with HIV globally will be scaled up. UNAIDS is encouraging other partners and funders to support the scale-up of the Y+ Social Aid Fund in order to ensure that more young people living with HIV are able to access health care and other services during the COVID-19 crisis and beyond.
Our work
Related




Feature Story
Coming together to address the cost of inequality
15 December 2020
15 December 2020 15 December 2020“My business suffered because of corona. Before corona, I would sell at least 10 egg trays a week. At the height of the pandemic, I was lucky if I could sell two trays,” lamented George Richard Mbogo, who is living with HIV, a father of two, and owns a chicken, egg and chips business in Temeke, a district in the southern part of Dar es Salaam, United Republic of Tanzania.
The COVID-19 crisis has adversely impacted the livelihoods of people living with HIV in the United Republic of Tanzania, exacerbating the challenges they face. These include HIV service delivery and widening social and economic inequalities.
“Corona has been a very difficult time. I lived with a lot of worry and stress. Driving a bodaboda (motorbike taxi) requires going into crowds and working closely with people. It has been difficult not to fall into anxiety and depression, balancing getting my HIV treatment and work. I had moments thinking of stopping taking my meds, but I didn’t,” said Aziz Lai, a motorcycle driver who also lives in Dar es Salaam.
Although the colliding pandemics of HIV and COVID-19 are hitting the poorest and the most vulnerable the hardest, through national resource mobilization the COVID-19 crisis has created an opportunity for partners to mobilize in support of the communities they serve.
The collaborative efforts between the government, development partners, including the United States President’s Emergency Plan for AIDS Relief, USAID and UNAIDS, the National Council of People Living with HIV (NACOPHA) and community activists have been key in responding to COVID-19, providing information, services, social protection and hope to people living with HIV during these unprecedented and trying times.
One such initiative is Hebu Tuyajenge, run by NACOPHA and funded by USAID, which focuses on increasing the utilization of HIV testing, treatment and family planning services among adolescents and people living with HIV, strengthening the capacity of community organizations and structures and improving the enabling environment for the HIV response through empowering people living with HIV.
Caroline Damiani is a single mother of three who is living with HIV and keeps chicken and ducks for a living. “Hebu Tuyajenge gave us personal protective equipment, sanitizers, soap and buckets and education about COVID-19 and how to take care of ourselves in order to stay healthy during the pandemic,” she said.
Through community-based services that supplement facility-based care, people living with HIV have been linked to and kept on treatment during the crisis by critical peer-to-peer HIV services.
For Elizabeth Vicent Sangu, who has been living with HIV for 26 years, her “numbers” speak for themselves.
“From my community follow-ups, I have returned 80 people to the clinic for CD4 count testing, inspired 240 people to get tests, reported 15 gender-based violence cases and provided education to 33 groups, including youth and church groups,” she said, beaming with pride.
NACOPHA helped Ms Sangu to come to terms with her status and helped her on her own journey of self-empowerment.
“Since becoming a treatment advocate for Hebu Tuyajenge, I have received help with entrepreneurship and education about HIV. I have become a teacher for others. I have made others brave about living with HIV and getting tested,” she said.
The partnership between community advocates and health facilities has paid off.
“Both we and our patients were fearful initially, but due to information and education, things got better. We focused on providing hourly and daily information to patients about corona and made sure that people practised safe social distancing,” said Rose Mwamtobe, a doctor at the Tambukareli Care and Treatment Centre in Temeke.
“Not only in the United Republic of Tanzania, but globally, COVID-19 is showing once again the cost of inequality. Global health, including the AIDS response, is interlinked with human rights, gender equality, social protection and economic growth,” said Leopold Zekeng, UNAIDS Country Director for the United Republic of Tanzania.
“The key to ending AIDS and COVID-19 is for all partners to come together, on a country and global level, to ensure that we leave no one behind,” he said.
Our work
Region/country


Feature Story
Snapshots on how UNAIDS is supporting the HIV response during COVID-19
03 December 2020
03 December 2020 03 December 2020From the very beginning of the pandemic, UNAIDS has been helping people living with and affected by HIV to withstand the impacts of COVID-19.
In January and February, when COVID-19 forced a lockdown in Wuhan, China, the UNAIDS China Country Office started to receive messages on social media from people living with HIV, expressing their frustration and seeking help.
A survey of people living with HIV in China devised and jointly launched by UNAIDS found in February that the COVID-19 outbreak was having a major impact on the lives of people living with HIV in the country, with nearly a third of people living with HIV reporting that, because of the lockdowns and restrictions on movement in some places in China, they were at risk of running out of their HIV treatment in the coming days.
The lockdowns had also resulted in people living with HIV who had travelled away from their home towns not being able to get back to where they live and access HIV services, including treatment, from their usual health-care providers.
The UNAIDS China Country Office worked with the BaiHuaLin alliance and other community partners to urgently reach the people at risk of running out of their medicines to ensure that they got their medicine refills. By the end of March, special pick-ups and mail deliveries of HIV medicines arranged by UNAIDS had reached more than 6000 people in Wuhan. UNAIDS also donated personal protective equipment to civil society organizations serving people living with HIV, hospitals and others to help in the very early stages of the outbreak.
But the UNAIDS China Country Office didn’t just help people in China. Liu Jie, the Community Mobilization Officer in the UNAIDS Country Office in China, was surprised when she had a call from Poland in March. “A Chinese man introduced himself, saying he is stranded and will run out of HIV medicine in two days,” she said.
With travel restrictions closing down more and more countries, the man could neither return home nor access medicine. Not knowing what to do, he reached out to a Chinese community-based organization and through it contacted UNAIDS in Beijing. A series of phone calls later and the National AIDS Center in Poland followed up—24 hours later, Ms Liu received a photo of the same man who called her, holding up a box of HIV medicine.
The man stuck in Poland wasn’t the only example of UNAIDS helping individuals to get the treatment they needed. By May, UNAIDS had helped hundreds of stranded people to obtain HIV medicine in countries around the world.
A day before Deepak Sing (not his real name) planned to return to India, all international travel ground to a halt, and he was stuck in Luanda, Angola. “I visited more than 10 pharmacies and explored options of delivery of antiretroviral medicines from India to Angola, but without success,” he said. The UNAIDS Country Director for Angola guided Mr Sing towards the national AIDS institute in Angola, which organized a conference call with a medical doctor because one of the medicines that Mr Sing took is not yet in use in the country. The doctor proposed a substitute and in less than 24 hours he picked up his medication.
It was realized early on in the COVID-19 pandemic that one way of ensuring that people on HIV treatment can continue to access their medicines, and to avoid the risk of transmission of the new coronavirus, was to ensure that people living with HIV got multimonth supplies of their treatment.
An early adopter of multimonth dispensing was Thailand, which announced in late March that it would dipense antiretroviral therapy in three- to six-month doses to the beneficiaries of the Social Security Insurance Scheme. After the decision, UNAIDS worked closely with the Ministry of Public Health and partners to advocate for the adaptation of the same policy for all health insurance schemes.
UNAIDS has supported countries worldwide to ensure that people living with HIV access multiple-month supplies of HIV treatment. For example, in Senegal in May, weaknesses in the supply chain, including inadequate assessments of the needs at some clinics for supplies of antiretroviral therapy and irregular supplies centrally, meant that not all people who needed such supplies got them. UNAIDS supported the government in tracking orders of antiretroviral medicines and in strengthening the supply chain.
A modelling group convened by the World Health Organization and UNAIDS estimated in May that if efforts were not made to mitigate and overcome interruptions in health services and supplies during the COVID-19 pandemic, a six-month disruption of antiretroviral therapy could lead to more than 500 000 extra deaths from AIDS-related illnesses and that gains made in preventing mother-to-child transmission of HIV could be reversed, with new HIV infections among children up by as much as 162%.
The physical distancing and hygiene recommendations to counter the new coronavirus are particularly difficult for some communities to follow. In April, the UNAIDS Regional Support Team for Eastern and Southern Africa and Reckitt Benckiser joined forces to distribute more than 195 000 hygiene packs to people living with HIV in the eastern and southern African region. Each pack consisted of a three-month supply of Dettol soap and Jik surface cleaner and was distributed in 19 countries through UNAIDS country offices and networks of people living with HIV as part of efforts to reduce exposure to the impact of COVID-19 among people living with HIV.
Kyrgyzstan saw a state of emergency imposed on some regions in March, which resulted in a loss of earnings for many people. The UNAIDS Country Office in Kyrgyzstan, with the support of a Russian technical assistance programme, organized the delivery of food packages for the families of people living with HIV, along with colouring books, marker pens and watercolour sets for the children of people living with HIV, to help them get through the lockdown. “We hope that this small help will go some way to enabling people living with HIV to remain on treatment,” said the UNAIDS Country Manager for Kyrgyzstan at the time.
The UNAIDS Country Office for Angola leveraged its partnerships to reach thousands of people in Luanda with food baskets. UNAIDS and partners provided support to women who inject drugs in camps and settlements in Dar es Salaam, United Republic of Tanzania, while a partnership that included UNAIDS provided cash transfer to vulnerable households in Abidjan, Côte d’Ivoire, for nutrition and food security and basic health kits.
Members of key populations and people living with HIV have been particularly impacted by the response to COVID-19. UNAIDS has supported the rights of gay men and other men who have sex with men, transgender people, sex workers, people who inject drugs and prisoners throughout the pandemic.
The Global Network of Sex Work Projects and UNAIDS in April called on countries to take immediate, critical action to protect the health and rights of sex workers during the COVID-19 pandemic. UNAIDS embarked on a project with the Caribbean Sex Work Coalition to help national networks address sex workers’ knowledge, HIV prevention and social support needs during COVID-19. “Sex workers need to be included in national social protection schemes and many of them need emergency financial support,” said the Director of the UNAIDS Caribbean Sub-Regional Office.
UNAIDS Jamaica provided financial support to ensure that Transwave, a transgender rights organization, had personal protective equipment and to supplement care package supplies and ensured that transgender issues are included in the coordinated HIV civil society response to COVID-19 in the country. “COVID-19 has laid bare just how vulnerable people are when they do not have equitable access to opportunities, justice and health care,” said UNAIDS Jamaica’s Community Mobilization Adviser. “That’s why it’s so important and inspiring that Transwave has continued its core work through all this.”
Since the start of the COVID-19 pandemic, UNAIDS has repeated the call that governments must protect human rights and prevent and address gender-based violence. In June, UNAIDS published a report highlighting six critical actions to put gender equality at the centre of COVID-19 responses, showing how governments can confront the gendered and discriminatory impacts of COVID-19.
“Just as HIV has held up a mirror to inequalities and injustices, the COVID-19 pandemic has put a spotlight on the discrimination that women and girls battle against every day of their lives,” said Winnie Byanyima, the Executive Director of UNAIDS, on the launch of the report.
In August, UNAIDS urged governments to protect the most vulnerable, particularly key populations at higher risk of HIV, in a report intended to help governments to take positive steps to respond to human rights concerns in the evolving context of COVID-19.
In the next month, UNAIDS issued a report that shows how countries grappling with COVID-19 are using the experience and infrastructure from the AIDS response to ensure a more robust response to both pandemics.
In October, UNAIDS issued guidance on reducing stigma and discrimination during COVID-19 responses. Drawing on 40 years of experience from the AIDS response, the guidance was based on the latest evidence on what works to reduce HIV-related stigma and discrimination and applies it to COVID-19. As with the HIV epidemic, stigma and discrimination can significantly undermine responses to COVID-19. People who have internalized stigma or anticipate stigmatizing attitudes are more likely to avoid health-care services and are less likely to get tested or admit to symptoms, ultimately sending the pandemic underground.
Looking to the future, UNAIDS joined the call for a COVID-19 People’s Vaccine—a vaccine that is affordable and available to all.
Our work
Related


Feature Story
The COVID-19 pandemic and women living with HIV: Caroline Damiani
14 December 2020
14 December 2020 14 December 2020Unlike many other countries in the region and the world, no lockdown measures were put in place at the height of the COVID-19 pandemic in the United Republic of Tanzania. In June, all restrictions on movement and gatherings were lifted. Nevertheless, the restrictions impacted people’s health and livelihoods, especially those who work in the informal sector, most of whom are women.
Women such as Caroline Damiani, from Chamazi, an administrative ward in the Temeke district of Dar es Salaam.
While, according to the government, about 83% of the 1.7 million people living with HIV in the United Republic of Tanzania are on HIV treatment, this leaves around 300 000 people living with HIV vulnerable. It has been shown that people with underlying health conditions are more susceptible to severe COVID-19 disease.
Thus, COVID-19 is a particular concern for people living with HIV, for both people who are not on HIV treatment and those who are, in ensuring they have access to medicines and health facilities.
The COVID-19 pandemic throws into sharp relief existing inequalities, including gender inequality and economic inequality.
In Chamazi, many women make a living selling homemade food, such as buns, fish or ice cream, or selling groceries in small kiosks.
Ms Damiani, a single mother of three, says her business was greatly affected by the COVID-19 pandemic. “Many people no longer wanted to buy my buns or home-made ice cream. I also couldn’t go to the main market to sell because of the crowds and the risk it brought. I then decided to switch completely to selling groceries at a small kiosk and rearing ducks and chickens to sell,” says Ms Damiani.
Ms Damiani has been living with HIV since 1998. All her three children are HIV-negative. Her husband divorced her and married another woman due to her HIV status and pressure from his family. To date, she still does not know his status. She lives with her daughter and granddaughter as her sons each have their own families. Her daily routine now includes feeding her ducks and chickens, helping her granddaughter with her schoolwork, performing household chores and tending her kiosk.
Ms Damiani says the COVID-19 pandemic affected her mental health. “I don’t have many friends and I spend most of my time at home or at the church. My stress levels increased in the earlier days of the pandemic and I began to lose weight,” she says.
“Fortunately, I never stopped taking my HIV treatment due to the insistence of my doctors that I adhere to my treatment regimen,” she says. “I am now determined to show everyone that you can live a full and healthy life as long as you don’t stop taking your medication.”
“The education and support we received from the Hebu Tuyajenge project also greatly helped to alleviate my stress.”
Hebu Tuyajenge is an initiative of the National Council of People Living with HIV, with support from UNAIDS and funded through USAID.
It focuses on increasing the utilization of HIV testing, treatment and family planning services among adolescents and people living with HIV, strengthening the capacity of community organizations and structures and empowering people living with HIV. In the face of the COVID-19 pandemic its members educated people living HIV on how to protect themselves from COVID-19.
“In my community, one of the biggest problems was the lack of education and information surrounding COVID-19. Most of us didn’t even know how to properly wash our hands to reduce the risk of catching the virus,” says Ms Damiani.
The Hebu Tuyajenge project is an example of how the government, development partners, civil society and community activists have been key in responding to COVID-19 in the United Republic of Tanzania, providing information, services, social protection and hope to people living with HIV during these unprecedented and trying times.
“The efforts by the government and other donors should continue. Things have now improved in the country because everyone is now aware of the pandemic and people continue to take precautions,” says Ms Damiani.
Our work
Region/country

Feature Story
Study shows how COVID-19 is impacting access to HIV care in the Russian Federation
27 November 2020
27 November 2020 27 November 2020A new study shows the negative impact that the COVID-19 pandemic is having on access to HIV care in the Russian Federation and shows that people living with HIV in the country are more susceptible to COVID-19 but less likely to seek testing or treatment.
More than a third of people living with HIV who were surveyed reported some impact on HIV services, including about 4% who reported that they had missed taking antiretroviral therapy because they could not get the medicine and nearly 9% who reported that they had missed taking medicine for tuberculosis prevention. However, the majority of respondents (about 70% of people living with HIV) did not experience problems obtaining antiretroviral therapy and about 22% reported that antiretroviral medicines were delivered to their home. More than 900 respondents from 68 regions of the Russian Federation, including people living with HIV and those who are not, were reached by the study.
“This study answers some of the most important questions about the impact of COVID-19 on people living with HIV in our country,” said Natalya Ladnaya, Principal Investigator and Senior Researcher at the Central Research Institute of Epidemiology of the Federal Service for Surveillance on Consumer Rights Protection and Human Wellbeing (Rospotrebnadzor).
According to Ms Ladnaya, the study confirmed that it is crucial for people living with HIV to protect themselves against the new coronavirus. The authors of the study also note the need to provide uninterrupted HIV treatment during the COVID-19 pandemic.
“Encouraging results were obtained on how the pandemic affected access to HIV treatment—many specialized institutions have been able to adapt to the new reality,” said Alexey Mikhailov, Head of the Monitoring Department of the Treatment Preparedness Coalition, who took part in the study.
According to the study, the number of people living with HIV with COVID-19 markers was four times higher than that of HIV-negative respondents. At the same time, they were half as likely, compared with HIV-negative respondents, to be tested for coronavirus infection and were less likely to seek medical help, even if they had symptoms.
The majority of respondents with HIV and COVID-19 coinfection had a higher risk of contracting COVID-19 due to the significant number of local cases of COVID-19 and the low level of use of personal protective measures, as well as an underestimation of the real personal risk of COVID-19 disease.
Although more than two thirds of the study participants were women, among people living with HIV and having had COVID-19 the majority of respondents were men who had lived with HIV for more than 10 years.
The authors of the study point to the need for further investigation into the causes of the increased incidence of COVID-19 and the low demand for medical care to treat the symptoms of COVID-19 among people living with HIV.
“The COVID-19 pandemic continues to affect all areas of our lives. We need to closely monitor the colliding pandemics of COVID-19 and HIV and provide support so as not to lose the gains in the response to HIV that have been achieved,” said Alexander Goliusov, Director, a.i., UNAIDS Regional Support Team for Eastern Europe and Central Asia.
The study was conducted by the Central Research Institute of Epidemiology of Rospotrebnadzor together with the Treatment Preparedness Coalition with the support of UNAIDS and Rospotrebnadzor.
Our work
Region/country
Related



Feature Story
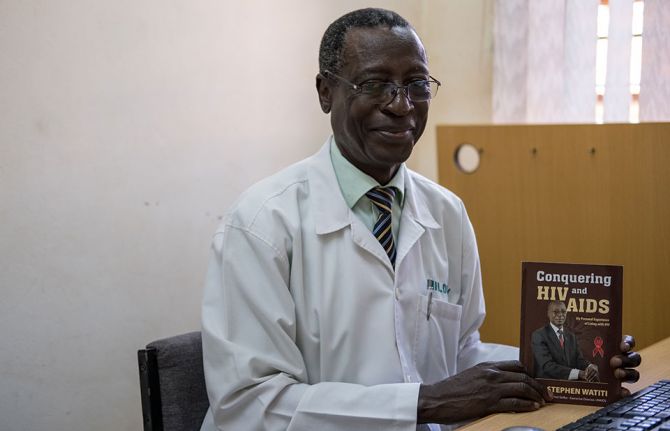
Stephen Watiti: a personal journey that imprints on others
27 November 2020
27 November 2020 27 November 2020Nearly 40 years into the HIV response, improved access to HIV treatment means the 26 million people living with HIV globally who are on HIV treatment can live long and healthy lives. But what does health care for an ageing population of people living with HIV look like?
Having lived with HIV for more than 30 years, this is a question 66-year-old Stephen Watiti from Uganda has been considering.
“My needs are going to be changing … and in the future most of the people living with HIV will be 50 years and above,” said the celebrated medical doctor, who is based at Mildmay Uganda Hospital, in Kampala.
In the eastern and southern Africa region, approximately 3.6 million of the 20.7 million people living with HIV are over the age of 50 years.
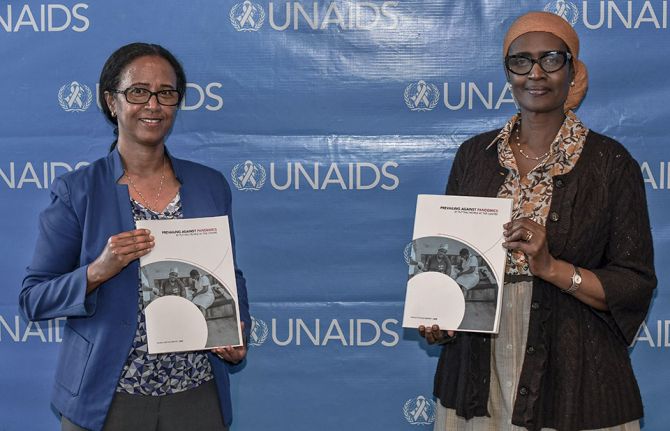
The new UNAIDS World AIDS Day report, Prevailing against pandemics by putting people at the centre, calls for a differentiated HIV response that is more intensive and more effective at ensuring that we reach those who until now have been left behind. This includes expanding treatment access equitably by providing people-centred, age-sensitive and integrated health services.
People living with HIV should be supported to lead long and healthy lives and people over 50 years of age should have equal access to social protection, employment and social integration.
Mr Watiti said little attention has been given to this phenomenon. “We have worked a lot in paediatric HIV. In geriatric HIV, there is no person who is trained in preparation for that,” he said.
Back in 1999, a period void of HIV treatment and substantial HIV knowledge and training among people in eastern and southern Africa, Mr Watiti experienced multiple AIDS-related illnesses. He had a “frightening” near-death experience where his CD4 count plummeted. His ailing body had to battle tuberculosis, cryptococcal meningitis and Kaposi’s sarcoma—all at the same time.
Mr Watiti started HIV treatment in 2000. However, due to the affordability and accessibility of the antiretroviral medicines in his regimen at that time, his adherence was poor, and he fell sick due to treatment failure.
In 2003, with a new antiretroviral regimen, and the unwavering support of a counsellor from the AIDS Support Organization in Uganda, Mr Watiti realized he was “no longer dying.”
During this period, he realized the need for him to educate and inspire his patients living with HIV. And so he returned to work.
Mr Watiti has come a long way. Despite living with uncertainty as part of an older generation living with HIV, Mr Watiti intends to live a full life, practising medicine well into his seventies.
“I’ll have to keep swallowing this medicine unless there’s a cure by then,” he said.
However, Mr Watiti wants to know what can be done to ensure that people living with HIV who are on treatment have a good quality life, including access to mental health services.
This is a question he raised during a conversation with UNAIDS Executive Director Winnie Byanyima at the launch of the UNAIDS World AIDS Day report.
Ms Byanyima agreed. “Considering that someone is going to live off a tablet for the rest of their lives and sometimes that person is living in poverty or hiding their secret because of stigma, this is a huge challenge of the mental and emotional well-being of a person,” she said. “People living with HIV need a wider comprehensive package of services, including mental health. The AIDS response cannot be narrowed just to the tablet.”
Mr Watiti was a beacon of hope for people who were living with HIV at a time when surviving AIDS was a grim prospect and is an example of resilience for people living with HIV today.
Mr Watiti says as he counsels his patients to overcome HIV stigma and about the importance of diligently taking their medication, it was as if he was talking to himself: “To tell you the truth, if there’s one person I've helped the most, it is me.”
Our work
Region/country

Press Release
UNAIDS calls on countries to step up global action and proposes bold new HIV targets for 2025
26 November 2020 26 November 2020As COVID-19 pushes the AIDS response even further off track and the 2020 targets are missed, UNAIDS is urging countries to learn from the lessons of underinvesting in health and to step up global action to end AIDS and other pandemics
GENEVA, 26 November 2020—In a new report, Prevailing against pandemics by putting people at the centre, UNAIDS is calling on countries to make far greater investments in global pandemic responses and adopt a new set of bold, ambitious but achievable HIV targets. If those targets are met, the world will be back on track to ending AIDS as a public health threat by 2030.
The global AIDS response was off track before the COVID-19 pandemic hit, but the rapid spread of the coronavirus has created additional setbacks. Modelling of the pandemic’s long-term impact on the HIV response shows that there could be an estimated 123 000 to 293 000 additional new HIV infections and 69 000 to 148 000 additional AIDS-related deaths between 2020 and 2022.
“The collective failure to invest sufficiently in comprehensive, rights-based, people-centred HIV responses has come at a terrible price,” said Winnie Byanyima, Executive Director of UNAIDS. “Implementing just the most politically palatable programmes will not turn the tide against COVID-19 or end AIDS. To get the global response back on track will require putting people first and tackling the inequalities on which epidemics thrive.”
New targets for getting back on track
Although some countries in sub-Saharan Africa, such as Botswana and Eswatini, have done remarkably well and have achieved or even exceeded the targets set for 2020, many more countries are falling way behind. The high-performing countries have created a path for others to follow. UNAIDS has worked with its partners to distil those lessons into a set of proposed targets for 2025 that take a people-centred approach.
The targets focus on a high coverage of HIV and reproductive and sexual health services together with the removal of punitive laws and policies and on reducing stigma and discrimination. They put people at the centre, especially the people most at risk and the marginalized—young women and girls, adolescents, sex workers, transgender people, people who inject drugs and gay men and other men who have sex with men.
New HIV service delivery targets aim at achieving a 95% coverage for each sub-population of people living with and at increased risk of HIV. By taking a person-centred approach and focusing on the hotspots, countries will be better placed to control their epidemics.
The 2025 targets also require ensuring a conducive environment for an effective HIV response and include ambitious antidiscrimination targets so that less than 10% of countries have punitive laws and policies, less than 10% of people living with and affected by HIV experience stigma and discrimination and less than 10% experience gender inequality and violence.
Prevailing against pandemics
Insufficient investment and action on HIV and other pandemics left the world exposed to COVID-19. Had health systems and social safety nets been even stronger, the world would have been better positioned to slow the spread of COVID-19 and withstand its impact. COVID-19 has shown that investments in health save lives but also provide a foundation for strong economies. Health and HIV programmes must be fully funded, both in times of plenty and in times of economic crisis.
“No country can defeat these pandemics on its own,” said Ms Byanyima. “A challenge of this magnitude can only be defeated by forging global solidarity, accepting a shared responsibility and mobilizing a response that leaves no one behind. We can do this by sharing the load and working together.”
There are bright spots: the leadership, infrastructure and lessons of the HIV response are being leveraged to fight COVID-19. The HIV response has helped to ensure the continuity of services in the face of extraordinary challenges. The response by communities against COVID-19 has shown what can be achieved by working together.
In addition, the world must learn from the mistakes of the HIV response, when millions in developing countries died waiting for treatment. Even today, more than 12 million people still do not have access to HIV treatment and 1.7 million people became infected with HIV in 2019 because they did not have access to essential HIV services.
Everyone has a right to health, which is why UNAIDS has been a leading advocate for a People’s Vaccine against COVID-19. Promising COVID-19 vaccines are emerging, but we must ensure that they are not the privilege of the rich. Therefore, UNAIDS and partners are calling on pharmaceutical companies to openly share their technology and know-how and to wave their intellectual property rights so that the world can produce successful vaccines at the huge scale and speed required to protect everyone.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 79 514 68 96
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org
Press centre
Download the printable version (PDF)


Feature Story
Interactive TV series about HIV launched in Kyrgyzstan
13 November 2020
13 November 2020 13 November 2020A new television series for young people in the Kyrgyz language, School Elections, was launched online last week. During six 15–20-minute episodes, a girl, Ayana, who is living with HIV, tells her story of bullying, friendship and the fight for human dignity. The producers of the series hope that Ayana’s example will give hope to young people who face similar challenges.
“We have a simple idea to promote: you may differ from others in your health, appearance or level of wealth. But regardless of this, we all deserve respect, friendship, love and happiness. This series is about kindness and acceptance of others as they are,” said Azim Azimov, Head of Production at the Media Kitchen production studio and the main screenwriter of the series.
Starting on 6 November, new episodes will be aired weekly on YouTube and will also be broadcast on television, Instagram and the teens.kg youth project website. Additionally, each series has one to three interactive episodes—the leading actors invite the viewers to look at the problems raised in the series through the viewers’ eyes, experience each situation for themselves and make their own decisions.
According to the United Nations Educational, Scientific and Cultural Organization (UNESCO), more than 30% of students around the world experience various forms of bullying at the hands of their classmates. Students who are perceived as “different” are often subjected to bullying for reasons of appearance, health status, including HIV status, sexual orientation and gender identity, social status or the economic situation of the family.
“This series tells people about the complex issue in simple and understandable language, to show how strong-willed and honest young people can overcome ignorance, indifference, cruelty and injustice, inspire others and change life for the better,” said Tigran Yepoyan, UNESCO Regional Adviser on HIV, Education and Health.
“This series is a powerful new instrument for reducing stigma in our society, it not only shows the difficulties of living with HIV, discrimination and bullying but also motivates our adolescents not to be afraid to fight for dignity and justice and move forward towards their dreams,” said Meerim Sarybaeva, UNAIDS Country Director for Kyrgyzstan.
The official soundtrack of the series, which was supported by the UNESCO Institute for Information Technologies in Education and UNAIDS, was performed by the singer Ayim Ayilchieva.
Our work
YouTube 1 st series
Soundtrack
Interactive episodes
Region/country
Related


Feature Story
A tale of two Jamaican clinics during COVID-19
03 November 2020
03 November 2020 03 November 2020A woman living with HIV is at the Centre for HIV Research and Education Services (CHARES) in Kingston, Jamaica. She normally gets a three-month allotment of her antiretroviral medicines. But not this time. The doctor warns her that, since April, state pharmacies have only been dispensing a one-month supply.
About a 20-minute drive away at the Comprehensive Health Clinic, a client waits for his name to be called. He doesn’t use one of the wooden benches allocated for sexual health patients. Instead, he finds a nearby seat and listens intently.
HIV service providers in Jamaica have been challenged this year with responding both to new challenges caused by COVID-19 and long-standing service delivery stumbling blocks. The UNAIDS Country Director, Manoela Manova, wanted to get a better understanding of the issues on the ground, so she visited both treatment sites to speak with everyone, from adherence counsellors to doctors.
The University Hospital of the West Indies’ CHARES has been a best practice model for HIV treatment in Jamaica. For the island as a whole, 79% of those on treatment were virally suppressed last year. At CHARES, however, an impressive nine in every 10 clients are virally suppressed and therefore keep healthy and are unable to transmit the virus.
But even for this accomplished programme, COVID-19 has presented significant challenges.
Laboratory support has been diverted toward COVID-19 and there has been a backlog in receiving viral load testing results.
CHARES had been used to writing three-month prescriptions for stable clients, but since COVID-19, state-run pharmacies have been dispensing only a one-month supply. This is part of the government’s strategy to avoid stock-outs given the supply chain challenges at this time, but it means that those on treatment need to go out to get their medicines more often. CHARES has begun home deliveries, particularly for older people, who are more reluctant to venture out given the novel coronavirus risk.
COVID-19 containment measures have increased the need for mental health support. Income loss, school closures and curfews have placed an added strain on thousands of Jamaican households, including many people living with HIV. But when clients are referred to psychiatric support in the main hospital they rarely go for fear of experiencing discrimination. Further, since the hospital in which CHARES is located is a designated COVID-19 treatment site, some clients have opted to stay away.
“We need closer monitoring and evaluation to address the challenges around patient management at this time,” said CHARES Programme Director Racquel Brown. “Optimally we would like to hire someone with responsibility for analysing patient data to make more strategic decisions around care and treatment.”
The Comprehensive Health Centre serves a number of people living with HIV alongside those infected with other sexually transmitted infections. Here, too, multimonth dispensing has not been possible during COVID-19. Patients’ need for nutrition support has been high during this period. Some have had their antiretroviral medicines but no food with which to take them.
But other challenges came before COVID-19. Two out of five clients are lost to follow-up. Patients have given service providers wrong addresses. And the clinic’s viral suppression rate stands at 70%, below the national average. Some come off their treatment against their doctor’s advice.
Ms Manova said many of the challenges at both clinics are linked to self-stigma and discrimination, which is the main issue facing Jamaica’s HIV response. For the country as a whole, just 43% of all people living with HIV were on treatment in 2019 despite the island’s relatively high testing coverage.
“Before and during COVID-19, our results are undermined by shame, fear and prejudice,” she noted. “For an effective public health response, we have to be deliberate and consistent about building trust with communities and combatting all forms of stigma and discrimination that block people from accessing care.”
“It was inspiring and sobering to spend time with these health-care providers,” Ms Manova said. “Jamaica has correctly treated community health-care employees as essential workers. Staff including community facilitators, social workers, adherence counsellors and case managers are just as needed as doctors and nurses. Their work is critical at this time to address the individual needs and emotions that could affect treatment outcomes.”
Our work
Region/country
Related


Feature Story
Community-led campaign encourages people living with HIV to start treatment
21 October 2020
21 October 2020 21 October 2020A new community-led public information campaign, It is in Your Power to, aimed at encouraging people living with HIV to start antiretroviral therapy has been launched in the four largest areas of the Russian Federation.
The campaign’s website has 12 “capsules” with inspiring stories told by people living with HIV. By “opening” the capsule, visitors can find out about people’s lives, find facts on antiretroviral therapy, ask questions and get help from peer counsellors on HIV-related issues.
All the stories deliver a message that being diagnosed with HIV does not define a person and that if people living with HIV start treatment they can live a long and productive life.
The campaign covers four major Russian areas—the Novosibirsk, Sverdlovsk and Chelyabinsk regions and the city of Saint Petersburg—where, according to the Federal AIDS Center of the Russian Federation, 200 000 people are living with HIV, about 20% of all registered HIV cases in the country.
“In the Sverdlovsk region, some people do not start treatment because they do not believe that HIV exists, some can’t accept their diagnosis, some are afraid of the side-effects of antiretroviral therapy and some have doubts about the effectiveness of the drugs. But the biggest obstacle is the fear of discrimination, fear of losing their job, fear of isolation. We believe we can address this by telling true stories of people living with HIV on treatment,” said Vera Kovalenko, Head of the New Life civil society organization.
The campaign was initiated and developed by several community-led civil society organizations, including Humanitarian Action (Saint Petersburg), the Humanitarian Project (Novosibirsk), Light of Hope (Chelyabinsk) and New Life (Sverdlovsk), with the support of a regional SOS_project funded by the Global Fund to Fight AIDS, Tuberculosis and Malaria and in close cooperation with other partners in the Russian Federation.
Denis Kamaldinov, Head of the Humanitarian Project, invited people to get help. “If you know you are HIV-positive but are not receiving treatment, please contact us for help. We will help with the registration at the AIDS centre. And the treatment is provided free of charge at the expense of the state,” he said.
“Our mission is to fight for every life, to give hope to everyone,” said Alexei Tananin, Head of Light of Hope.







