HIV Prevention
Documents
Male engagement in HIV testing, treatment and prevention in eastern and southern Africa — A framework for action
07 April 2022
This framework provides insights into some of these questions. It categorises existing research, knowledge and best practices and outlines the necessary building blocks for planning, implementing, and monitoring improvement in the HIV response among men and boys within a broader gender equality framework. The framework is an evidence-based action road map to guide the development of national strategies; when contextualized to local and national contexts and epidemiological situations, the framework provides a foundation for country-led movements to achieve the globally agreed HIV goals in the Global AIDS Strategy 2021–2026 and work towards achieving gender equality.
Related
 The impact of the US funding freeze and cuts on Namibia’s civil society: A struggle for survival
The impact of the US funding freeze and cuts on Namibia’s civil society: A struggle for survival

10 March 2025
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025
 Status of HIV Programmes in Botswana
Status of HIV Programmes in Botswana

20 February 2025





Feature Story
Training health-care workers in Indonesia to improve HIV services for young key populations
30 March 2022
30 March 2022 30 March 2022“Young people here don’t regularly access HIV services. I really want to invite my friends to get tested, but they are all so afraid. They don’t have enough information or support from their families and are scared about finding out their status,” said Andika Bayu Aji, a young person from West Papua, Indonesia.
The HIV epidemic among young people in Asia and the Pacific has largely been overlooked, even though about a quarter of new HIV infections in the region are among people aged 15–24 years. The vast majority of young people affected by HIV in the region are members of vulnerable populations—people living with HIV, gay men and other men who have sex with men, transgender people, sex workers and people who inject drugs.
Like many countries in the region, Indonesia’s HIV infections among young people, which make up almost half of new infections, are attributed to stigma and discrimination, poor educational awareness of HIV, lack of youth-friendly services and social taboos.
“Young people far too often experience stigma and discrimination in health-care settings. Health-care workers are first-line responders. If the services are bad, young people won’t use them and they will tell other young people not to use them. We are limited by which clinics we can access because many, if not most, are not youth-friendly,” said Sepi Maulana Ardiansyah, who is known as Davi and is the National Coordinator for Inti Muda, the national network of young key populations in Indonesia.
A recent study conducted by Inti Muda and the University of Padjajaran found that the willingness of young people to access services in provinces like West Papua was very low, mainly due to the lack of youth-friendly services and the poor understanding of key population issues by health-care workers. Young people often face difficulty accessing services because of the remoteness of clinics and hospitals and encounter barriers such as the age of consent for testing.
Stigma and discrimination, and especially discrimination from health-care providers, discourages many young key populations from accessing HIV services. Concerns about privacy and confidentiality are some of the main challenges. Additional obstacles include that the opening hours of public clinics are often ill-suited to people’s daily routines, and the assumptions and attitudes of health-care workers can be judgemental, especially on issues around sexual orientation, gender identity and mental health.
Between 14 and 18 March, Inti Muda, with technical support from Youth LEAD and UNAIDS, organized a sensitization training of health-care workers in two cities, Sentani and Jayapura, in the West Papua region. More than 50 health-care workers participated. A few days before the training, Inti Muda organized a festival for more than 80 young people, joining in an effort to engage young people in the HIV response and generate demand for access to HIV services.
“Prior to this training, I didn’t know about the different needs of key populations, which hinders our ability to reach them. We learned about important techniques for reaching young people, such as providing youth-friendly counselling, digital interventions and encouraging them to get tested,” said Kristanti, from the District Health Office of Jayapura.
“I learned that the needs of young people are diverse. The training will allow us to improve our services to become youth-friendly, which is now our main priority,” added Hilda Rumboy, a midwife in charge of the HIV Services Department at the Waibhu Primary Health Centre.
The training and festival were supported by the Australian Department of Foreign Affairs and Trade (DFAT). The recent investment of AU$ 9.65 million set aside by the Australian Government from the sixth replenishment of the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund), including DFAT funding of AU$ 2 million previously committed to UNAIDS, is aimed at reducing the annual number of new HIV infections among key populations in Cambodia, Indonesia, Papua New Guinea and the Philippines.
“Ensuring young people and vulnerable groups have access to accurate, digestible information about how to prevent HIV, and that testing facilities are cheap and accessible, is crucial to ending the AIDS epidemic. We are proud to work with local communities and UNAIDS to increase availability of information on HIV, improve the reach and quality of medical services and encourage young people and vulnerable groups to get tested,” said Simon Ernst, Acting Minister Counsellor for Governance and Human Development at the Australian Embassy in Indonesia.
The training is based on the manual developed by Youth LEAD in 2021, which was financially supported by the Global Fund’s Sustainability of HIV Services for Key Populations in Asia Programme and the UNAIDS Regional Support Team for Asia and the Pacific. Under the DFAT grant for the next two years, Youth LEAD will expand the training to two more countries, Cambodia and the Philippines, supporting networks led by young people in the respective countries to roll out the training.
“Young people still encounter many challenges that prevent them from accessing the life-saving health care they need. The UNAIDS Country Office for Indonesia is working closely with the UNAIDS regional support team and DFAT to ensure that networks led by young people have the capacity and leadership capabilities to take control of the HIV response and to have direct involvement in creating safe spaces where young people can access HIV services free from stigma and discrimination,” said Krittayawan Boonto, the UNAIDS Country Director for Indonesia.
Our work
Region/country
Related




Feature Story
Eastern Cape becomes the first South Africa province to campaign on U = U
21 March 2022
21 March 2022 21 March 2022Hundreds of people living with HIV are spreading the word in South Africa that effective treatment can prevent onward transmission of the virus. The Eastern Cape has become the first of nine provinces in South Africa to launch a public information campaign to raise awareness of U = U (undetectable = untransmittable) and to encourage people living with HIV to commence, maintain or resume treatment and achieve and maintain an undetectable viral load.
The innovative campaign celebrates the fact that people living with HIV who receive effective antiretroviral therapy and achieve and maintain an undetectable viral load cannot pass HIV to others via sexual activity.
The overall goal of the Eastern Cape U = U campaign is to reduce HIV transmission by promoting treatment adherence and decreasing loss to follow-up, increasing viral suppression and improving data management. The campaign is also promoting HIV prevention, including the use of condoms, and wider sexual and reproductive health.
Importantly, the campaign was designed to help the province to catch up and reach the HIV targets for 2020, under which 73% of all people living with HIV should have achieved viral suppression by 2020. Eastern Cape had reached 58% by 2020. The new global target for viral suppression is 86% by 2025.
The campaign was officially launched with pledges of support from Eastern Cape Premier Oscar Mabuyane, community members and other prominent stakeholders, including the Eastern Cape Provincial AIDS Council, the Department of Health, the South African National AIDS Council and UNAIDS.
Campaign leaders hope to inspire similar activities across the country and beyond. “We want this to be a bottom-up approach,” said nurse clinician and U = U pioneer Mandisa Dukashe, who first approached the Eastern Cape AIDS Council about the campaign. “We hope the success in Eastern Cape will inspire other provinces, at the national level and outside South Africa,” she said.
Four hundred people living with HIV have been trained as U = U peer educators across South Africa, including 70 in Eastern Cape, who formed the core of the new campaign. Campaigners are collaborating in a series of groups to ensure that awareness is raised, communities are mobilized and service providers are trained and ready.
The implications of U = U are that people living with HIV need access to treatment as soon as they are diagnosed and to maintain effective treatment to become virally suppressed. This means that people visiting health clinics and receiving a positive HIV test result need quality counselling, said Ms Dukashe, who is herself living with HIV. “There is not much time spent now with clients when initiating their treatment and they can get lost in the health system.”
The concept of U = U arose from trials in South Africa and elsewhere that found that early antiretroviral treatment of HIV infection can prevent onward transmission. However, people can only know whether they are virally suppressed by taking a viral load test. Viral load levels should be monitored regularly to be sure that the HIV medicines are working, and this requires the active involvement of health-care professionals.
The campaign organizers want health-care providers to communicate this information to all people living with HIV. They particularly hope to inform couples’ counselling, especially those in serodiscordant relationships, where one partner is living with HIV and the other is HIV-negative. U = U cannot only prevent transmission of HIV to the negative partner, but can also prevent onward transmission to their child if the couple conceives.
Importantly, knowledge of U = U can help to reduce stigma about HIV infection and motivate people to start treatment in order to become virally suppressed and continue follow-up care. Globally, 66% of people living HIV were virally suppressed in 2020, with South Africa estimated to have achieved 61%, with 58% in Eastern Cape. This compares to the global targets of 73% of all people living with HIV achieving viral suppression by 2020, and 86% by 2025.
Over the next six months, Eastern Cape province will spread the U = U message across diverse audiences, through social media, radio and print media. Peer educators are working as HIV ambassadors and sharing their stories to inspire others. The campaign will also use billboards, rallies and community dialogues to reach as many people as possible.
“There is clear evidence that U = U messaging works and helps to bring people back to treatment and reduces stigma and discrimination,” said UNAIDS Country Director for South Africa, Eva Kiwango. “Treatment interruption is a persistent issue in South Africa and this campaign helps remind everybody that having an undetectable viral load when you are taking HIV treatment also stops transmission of HIV to others. This is critical for populations at higher risk of infection, such as adolescent girls and young women and key populations, including sex workers and gay men and other men who have sex with men.”
Our work
Region/country


Press Statement
Identification of fast-spreading HIV variant provides evidence of urgency to halt the pandemic and reach all with testing and treatment
07 February 2022 07 February 2022Around 10 million people living with HIV are still not on antiretroviral therapy
GENEVA, 7 February 2022—Newly published research from the Netherlands has revealed the existence of a more transmissible and damaging variant of HIV. People living with the newly revealed HIV subtype experience double the rate of immune system decline (CD4 count), have higher HIV viral loads (amount of virus in the blood) and are vulnerable to developing AIDS two to three times faster after diagnosis than if they were living with other strains of the virus. The study, led by researchers from the University of Oxford’s Big Data Institute, was the first to discover this highly virulent variant of the subtype-B of HIV. The study also revealed that the variant has been circulating in the Netherlands for years and remains receptive to HIV treatment.
The HIV pandemic continues to take a life every minute and scientists have long worried about the evolution of new, more transmissible, variants of HIV. This newly identified variant does not represent a major public health threat but underscores the urgency of speeding up efforts to halt the HIV pandemic.
“Ten million people living with HIV worldwide are not yet on treatment, fuelling the continued spread of the virus and potential for further variants,” said Eamonn Murphy, UNAIDS Deputy Executive Director, Programme, a.i. “We urgently need to deploy cutting-edge medical innovations in ways that reach the communities most in need. Whether it’s HIV treatment or COVID-19 vaccines, inequalities in access are perpetuating pandemics in ways that harm us all.”
HIV remains the deadliest pandemic of our time—an estimated 79 million people have become infected with the virus, for which there is still no vaccine and no cure. Some 36 million people have died from AIDS-related illnesses since the start of the pandemic and 1.5 million people were newly infected with HIV in 2020. Of the 38 million people living with HIV today, 28 million are on life-saving antiretroviral therapy, keeping them alive and well and preventing transmission of the virus.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 79 514 68 96
bartonknotts@unaids.org
UNAIDS Media
communications@unaids.org


Feature Story
The importance of engagement of community organizations to ensure the sustainability of HIV services in eastern Europe and central Asia
02 February 2022
02 February 2022 02 February 2022Participants from 21 countries in central and eastern Europe and central Asia and the Balkans met in December 2021 in Istanbul, Turkey, for the International Health Sustainability Forum: HIV and COVID-19 in Eastern Europe and Central Asia.
The participants discussed the most efficient means to ensure the sustainability of AIDS programmes and the role of community organizations in providing uninterrupted HIV services during the COVID-19 pandemic in the region.
The results of a three-year project implemented by the Alliance for Public Health in a consortium with 100% Life (formerly the All-Ukrainian Network of People Living with HIV), the Central Asian Association of People Living with HIV and the Eurasian Key Populations Coalition, with the participation of a wide range of partners, were also presented and reviewed. The project was funded by the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) and was supported by UNAIDS.
Addressing the forum, Peter Sands, the Executive Director of the Global Fund, highlighted the key elements of successful AIDS programmes in the region, among them “systems, not project-based interventions,” the meaningful engagement of communities and their ownership of the HIV response and removing human rights barriers.
“Increasing public funding of HIV services through social contracting mechanisms, which was a rare case a few years ago, has now become an important component of a systemic response to the HIV epidemic in many countries of the region,” said Andriy Klepikov, the Executive Director of the Alliance for Public Health. He noted that over the past three years public funding of HIV services through social contracting mechanisms in the region amounted to more than US$ 30 million. “This is one of the most important achievements of the joint efforts of community organizations and governments in the region.”
However, as the participants noted, to sustain this success an appropriate legal framework, the support of governments and the strengthening of initiatives made by communities are needed.
Several cities across the region have produced impressive results due to the leadership of local governments that have not only taken responsibility for developing and funding municipal AIDS programmes, including services for key populations, but also through the involvement of community organizations in their implementation.
Thus, systematic work by the city government in close cooperation with community organizations saw Odesa, Ukraine, achieve the 90–90–90 targets. “Odesa has managed to change the strategy for HIV testing and treatment. Our experience has already received recognition from the international community. And we are ready to share our best practices and successes,” said Gennadiy Trukhanov, the Mayor of the city.
The experience of the Republic of Moldova was presented by Fadei Nagachevsk, the Vice-Mayor of Chisinau, and Ruslan Poverga, from Initiative Positiva, who demonstrated the importance of close interactions between city governments and community organizations to ensure the accessibility of services for key populations. Mr Poverga also noted that the integration of peer consultants and social workers in public institutions helps to ensure the sustainability of services.
The best practices of municipal responses to the HIV and COVID-19 epidemics of Kyiv, Ukraine, Osh, Kyrgyzstan, Podgorica, Montenegro, Kragujevac, Serbia, Bern, Switzerland, Prague, Czechia, and Istanbul, Turkey, were also presented.
According to Sergiy Dmitriev, an international expert on public health, civil society organizations have also played a leading role in reducing the prices of antiretroviral medicines by monitoring the procurement cycle and budget and attracting generic suppliers. The price of an annual course of first-line antiretroviral therapy has decreased to US$ 131—the average cost of first-line antiretroviral therapy in nine countries in the region was US$ 192 in 2017. Most of the savings on purchases, about US$ 119 million, remained within AIDS programmes.
Another critical area where community organizations have been playing an increasingly important role in the region is community-led monitoring of human rights violations. The results of work on the REAct system (a human rights violation monitoring system) were presented: during 2020 and 2021, more than 6000 cases of human rights violations and cases of stigma and discrimination were registered in seven countries.
Among the most frequent offences in the region are violence by law enforcement officials, denial of access to medical services, disclosure of medical data and stigma in health-care settings, as well as physical violence against women by their partners and relatives. Based on an analysis of all cases, civil society organizations, together with lawyers and governmental partners, developed recommendations for countries that will form the basis for further advocacy.
“Community-led organizations have become leaders in providing people-centred, human rights-based HIV services in the majority of countries in eastern Europe and central Asia,” said Alexander Goliusov, Director, a.i., UNAIDS Regional Support Team for Eastern Europe and Central Asia. “Their meaningful engagement in decision-making processes and financial sustainability provided by government funding are the key for an effective response to HIV and COVID-19 and for future pandemics.”
The forum video is available: in Russian and English
https://www.youtube.com/watch?v=gCVqVUKAJmo
https://www.facebook.com/AlliancePublicHealth/videos/4581620981957116
Region/country
Related


Update
One hundred and fifty thousand preventable new HIV infections among children in 2020
31 January 2022
31 January 2022 31 January 2022Most of the 150 000 new HIV infections among children in 2020 could have been prevented. A strong start would be to better engage women and girls at significant risk of acquiring HIV infection in integrated antenatal care and HIV services, including HIV prevention and testing, delivered at the local level, and to ensure that those who are HIV-positive receive treatment before pregnancy. Nearly 65 000 child infections occurred in 2020 because women already living with HIV were not diagnosed during pregnancy and did not start treatment.
More than 35 000 additional child infections occurred because women acquired HIV during pregnancy or breastfeeding, which led to a spike in their viral load and a high risk of vertical transmission. Women at substantial risk of HIV infection require tailored combination HIV prevention, including pre-exposure prophylaxis, more comprehensive counselling, repeat HIV testing and the provision of self-testing kits for partners.
More than 38 000 additional child infections occurred when mothers who started antiretroviral therapy did not continue treatment during pregnancy and breastfeeding, and nearly 14 000 occurred among women who were on treatment but not virally suppressed. Improving the quality of treatment and care—including the use of optimized treatment regimens and peer-assisted retention efforts (such as mentor mothers)—can help close these gaps.
Our work
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025




Feature Story
Love and condoms: broadcast on the importance of condoms in eastern Europe and central Asia
05 January 2022
05 January 2022 05 January 2022On the eve of World AIDS Day, the Russian language social media network OK.RU hosted a live broadcast, Telling the Truth, as part of an education project that has been run by UNAIDS and the United Nations Educational, Scientific and Cultural Organization since 2015. The show was organized in collaboration with a popular magazine, Domashniy Ochag, and was devoted to the use of condoms and the link to the HIV epidemic in eastern Europe and central Asia.
During the broadcast, which was watched by more than 1 million people, experts and celebrities discussed the most common myths, misconceptions, difficulties and fears connected to condom use.
Before the broadcast, an online survey of 1050 people aged 18 to 60 years was conducted on what Russian Internet users think about protection against sexually transmitted infections and what they consider to be safer sex. The study found that 87% of respondents had had sex without a condom, with older respondents reporting higher rates of sex without a condom.
“HIV has already reached the general population in this region. Almost 70% of all new HIV infections have been linked to heterosexual sex in recent years. At-risk people include single women aged more than 35 years and men and women who no longer worry about contraception and therefore do not use a condom,” said Natalya Ladnaya, Senior Researcher at the Central Research Institute of Epidemiology, Rospotrebnadzor.
Among the reasons for unprotected sex, the respondents most often named “awkwardness of discussing it with a partner”, which was reported by 41% of the respondents. In addition, “trust in a partner” (35%), “discomfort during intercourse” (20%), “fear of spoiling romance” (31%) and “fear of being misunderstood by a partner” (19%) were listed among the reasons for not using a condom.
Appearing on the broadcast was Masha Godlevskaya, who has been living with HIV for 22 years. She works as a peer consultant for the EVA Association, which provides HIV services. She explained that many women who go to the EVA Association for a consultation are embarrassed to carry condoms because of the stereotype that having a condom available means that they are available and ready for sex.
“Both women and men are victims of this story,” said Ms Godlevskaya. “If a man insists on having sex without a condom, the woman should be ready to say: “I don’t want to. I don’t want to offend you, but no sex without a condom.””
“We help women believe in themselves, work with a psychologist, fight back against their abusers, build new relationships where they can discuss everything frankly. I want our women to be able to defend their bodies, their rights, and be able to take their lives into their own hands,” she added.
Vera Brezhneva, UNAIDS Goodwill Ambassador for Eastern Europe and Central Asia, noted that many women vulnerable to HIV were born in the time of the Soviet Union, when there was no promotion of safer sex. “I didn’t know about HIV at all. Most of us at that time were afraid of pregnancy only. We believed in love as if love protects you from everything. We were not told that a condom is not protection against men or women but protection against infections.”
Ms Godlevskaya shared her story of becoming infected with HIV. “I was 16 years old. He was my first love, and, as it seemed to me then, the last one. It was a serious relationship, there was trust and we knew nothing about the need to use a condom.”
Marina Travkova, a family psychologist and sex therapist, noted that adolescents are vulnerable to HIV and other sexually transmitted infections. “They need help. There is nowhere to get reliable information. I am in favour of compulsory sex education in high school and for condoms to be available in school toilets. I always remind my sons before they go out: wallet, phone, brain, condom,” she said.
For a significant part of the population, especially young people, the cost of condoms is too high, noted Ms Ladnaya. “We are discussing these issues with partners, and we hope that there will be government programmes to support the production of condoms. There are nongovernmental organizations that provide condoms for free, but I believe that they should be available at every step,” she said.
Discussing the perception that sex with a condom is worse than sex without one, the reason that people often do not use condoms, the panellists noted that comfort might be related to the quality and size of a condom, as well as insufficient knowledge of how to use a condom and lubricant correctly.
Grisha Tumanov, a journalist and blogger and author of the Man, Where Are You Going? podcast, commented on a viewer’s question: “Is a condom needed if it’s love, which presupposes mutual trust.” He noted that, “We don't have a culture of speaking on sensitive topics, what you expect from relationships, including sexual relationships. And love does not absolve one of responsibility. This does not happen in adulthood. You are responsible for each other.”
Our work
Region/country
Related
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025

Update
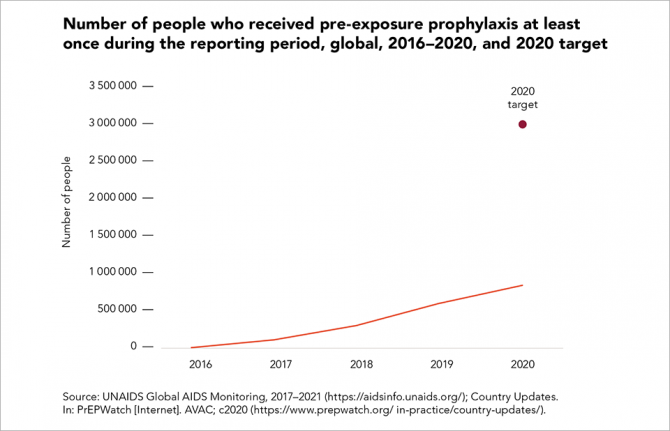
Pre-exposure prophylaxis use expands, but not fast enough
17 January 2022
17 January 2022 17 January 2022It has been more than a decade since the first evidence of the efficacy of daily oral pre-exposure prophylaxis (PrEP) was published. PrEP is now a valuable additional option for people who are at higher risk of acquiring HIV, and its global uptake has continued to increase, despite the COVID-19 pandemic: country data show that approximately 845 000 people in at least 54 countries received PrEP in 2020—a 43% increase since 2019, and a 182% increase since 2018.
Much of the PrEP scale-up is still highly concentrated in a fairly small number of countries, notably the United States of America, and in eastern and southern Africa, where Kenya and South Africa accounted for 158 630 (19%) of people who received PrEP at least once during 2020 in the region.
There continue to be substantial gaps in the availability of PrEP, however: the total number of people using this prevention option in 2020 was just 28% of the target of 3 million in low- and middle-income countries, which represents only 8% of the new global 2025 target.
Our work
Documents
2021 UNAIDS Global AIDS Update — Confronting inequalities — Lessons for pandemic responses from 40 years of AIDS
14 July 2021
UNAIDS report shows that people living with HIV face a double jeopardy, HIV and COVID-19, while key populations and children continue to be left behind in access to HIV services. Read the press release | Data slides | This document is also available in Arabic
Related
 UNAIDS calls for rights, equality and empowerment for all women and girls on International Women’s Day
UNAIDS calls for rights, equality and empowerment for all women and girls on International Women’s Day

06 March 2025
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025


Press Statement
UNAIDS welcomes the approval of long-acting injectable cabotegravir as a pre-exposure prophylaxis for HIV prevention
22 December 2021 22 December 2021The United States Food and Drug Administration announced its first approval of a long-acting HIV prevention medication earlier this week. The long-acting injectable cabotegravir (CAB - LA) is approved as a pre-exposure prophylaxis (PrEP) for adults and adolescents who are at risk of acquiring HIV sexually in the United States of America.
This is the first time an injectable antiretroviral drug becomes available as a pre-exposure prophylaxis for prevention of HIV. The long-acting formula is a step forward and a valuable addition to the HIV prevention toolbox and will make acceptance and adherence easy.
A long-acting PrEP product such as CAB-LA, taken initially as two injections one month apart and then after every two months afterward, could offer a better choice for adults and adolescents at substantial HIV risk who either do not want to take or struggle with taking a daily tablet. Companies holding new technologies should share their knowledge and recipes with generic producers to ensure availability and affordability in low and middle-income countries.
UNAIDS is calling for this new drug to quickly be made available and affordable to people who need it most not just in the United States of America but everywhere in the world. The mistakes of three decades ago when lifesaving drugs were only available to those who could afford it must not be repeated. Market strategies such as generic competition and public health-oriented management of intellectual property rights, either through voluntary agreements or the use of TRIPS flexibilities must be used to make this new drug widely available.
To make this drug available equitably across the world, a series of actions are essential. Firstly, the drug has to be approved by regional and national regulatory authorities in a speedy manner. It is encouraging to see that the developer of CAB-LA, has already submitted to the South African Health Products Regulatory Authority (SAHPRA) for approval and an outcome is expected in early 2022. However access must go much further. Secondly the selling price must come down through a combination of measures such as licencing and involvement of generic producers. Thirdly, national HIV prevention programmes must prepare roll out plans and prepare their health systems and communitiues to deploy this new HIV prevention option as soon as they are available.
Current pre-exposure prohylaxis--Tenofovir plus Emtricitabine—tablets have to be taken daily as oral PrEP. They are highly effective in preventing HIV acquisition among persons at substantial risk when taken as prescribed. However many find it challenging to take a daily tablet. Another option—dapiviringe vaginal ring—is becoming available as additional prevention option for women at substantial risk of HIV infection.
The CAB-LA option could be a game-changer for the HIV response, making PrEP simpler or less burdensome for all genders. This may also circumvent the stigma associated with daily oral therapy and improve correct dosing and adherence which is critical for PrEP effectiveness.
This week’s United States Food and Drug Administration approval follows results from two trials. The first trial, HPTN 083, was conducted in 4 566 gay men and men who have sex with men and transgender women at research centers in Argentina, Brazil, Peru, the United States, South Africa, Thailand, and Vietnam. CAB – LA reduced the risk of sexually acquired HIV by 66% compared to daily oral. In the second trial HPTN 084, among 3,223 at-risk women aged 18-45 across 20 trial sites in seven countries in Sub Saharan Africa (Botswana, Eswatini, Kenya, Malawi, South Africa, Uganda, and Zimbabwe), CAB – LA reduced the risk of acquiring HIV by 89% compared to daily oral PrEP.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.