HIV Prevention





Feature Story
Four Albanian cities commit to ending the AIDS epidemic by 2030
19 June 2024
19 June 2024 19 June 2024Four Albanian cities—Kolonja, Durrës, Pogradec, and Shkodra—have signed the Paris Declaration on AIDS committing to ending AIDS as a public health threatby 2030. By signing the declaration, the Mayors committed to achieving the 95-95-95 targets by 2025 and called on other municipalities in Albania, including the capital Tirana, to join this effort.
The Albanian cities are the latest additions to the list of more than 550 other cities around the world that are part of the Fast-Track Cities initiative which aims to fast-track action at local level to improve the quality of life of people living with and affected by HIV.
In order to fulfill their commitments, the cities have developed different plans of action based on their local circumstances. For instance, the Municipality of Durrës plans to increase investments in methadone maintenance therapy, aiming to expand the number of people benefiting from such services by 10% each year.
The Municipalities of Pogradec and Kolonja are focused on raising awareness among migrant populations to increase HIV testing rates in these regions. As border cities with a significant male population migrating for work, ensuring these communities are well-informed and have access to necessary health services is crucial.
Finally, the Municipality of Shkoder aims to foster a partnership with Podgorica in Montenegro to exchange experiences and best practices in developing the "Healthy Houses" model, which has been successful in the neighboring country. The "Healthy Houses" initiative is a free social service providing psychosocial support to citizens. It focuses on improving the quality of life, reducing risks, and offering support to socially vulnerable groups. The service addresses a range of issues, including HIV, domestic violence, addiction, services for LGBTQ+ peopleand others.
Olimbi Hoxhaj, Executive Director of the Albanian Association of People Living with HIV, hopes that signing the Declaration and the follow-up actions will not only help prevent new HIV infectionsbut will also significantly reduce AIDS-related mortality.
Albania has a low HIV-prevalence epidemic but faces an increasing number of new HIV cases. From 1993 to 2023, 1,716 cases were diagnosed, with 113 new cases in 2023 alone. Most HIV testing occurs in the late stages of infection (about 60% of new cases), meaning official figures do not fully represent the actual infection rate.
The Minister of Health and Social Protection of Albania, Ogerta Manastirliu, emphasized that rapid diagnosis and treatment are key. “The whole fight in this aspect is timely diagnosis so that the treatment can start as soon as possible, and the infection is under control.”
“While the European region continues to face political, economic, and healthcare challenges due to regional conflicts, migration, and other complexities, it is important to secure commitment from municipalities to advance progress towards the crucial HIV targets,” said Eamonn Murphy, UNAIDS Regional Director for Asia-Pacific and Eastern Europe and Central Asia.
Technical assistance to all municipalities in developing their local programs was provided through the cooperation between the International Association of AIDS Care Providers (IAPAC), the Fast-Track Cities Institute (FTCI), UNAIDS and the Global Fund’s regional #SoS 2.0 project, which aims to ensure the sustainability of HIV services in 15 countries in Eastern Europe. "Since 2019, with our support, 21 municipalities from Southeast Europe have joined the Fast-Track Cities initiative," said Tetiana Deshko, Director of the International Programs Department at the Alliance for Public Health.
Learn more
Region/country
Related
Documents
HIV Response Sustainability Roadmap — Part A — Companion Guide
30 April 2024
As we approach 2025, the longer-term sustainability of the HIV response is a pressing concern: work to achieve and sustain an impactful HIV response must intensify. This Companion Guide is intended to support that work. It complements the HIV Response Sustainability Primer, which describes a new approach to sustainability and provides recommendations for developing HIV Response Sustainability Roadmaps. Related: Download the HIV response sustainability primer.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025
 UNAIDS urges that all essential HIV services must continue while U.S. pauses its funding for foreign aid
UNAIDS urges that all essential HIV services must continue while U.S. pauses its funding for foreign aid

01 February 2025


Press Statement
UNAIDS stands with LGBTQ+ communities worldwide as PRIDE celebrations get underway
29 May 2024 29 May 2024GENEVA, 29 May 2024—As LGBTQ+ communities and allies take to the streets to mark PRIDE month, UNAIDS is speaking out in solidarity, rejecting the criminalization, discrimination and stigmatization of LGBTQ+ people and insisting on respect for all.
“The PRIDE celebrations are a demonstration of the power of inclusivity,” said UNAIDS Executive Director, Winnie Byanyima. “PRIDE has brought the world a long way in the struggle to protect the human rights of LGBTQ+ people. So much has been won. But the progress that has been made is under threat. The world needs the spirit of PRIDE more than ever today: to protect everyone’s health, we need to protect everyone’s rights.”
There is much to celebrate. UNAIDS data shows that 123 countries do not penalize same-sex relations. This represents the highest number of countries rejecting criminalization ever.
More and more countries have been scrapping the harmful punitive anti-LGBTQ+ laws which are often leftovers of colonial rule. Since 2019 alone, Botswana, Gabon, Angola, Bhutan, Antigua and Barbuda, Barbados, Singapore, Saint Kitts and Nevis, Cook Islands, Mauritius and Dominica have all repealed laws that had criminalized LGBTQ+ people.
However, the human rights of the LGBTQ+ community are threatened by a globally coordinated and well-funded extremist anti-rights network who are spending millions promoting hate and social division and are proposing ever more draconian laws to punish LGBTQ+ people. Attacks on LGBTQ+ people violate human rights and undermine public health.
This perilous time calls for courage and solidarity from everyone. PRIDE has always been as much about protest and commemoration as celebration. The first marchers in New York more than 50 years ago knew that PRIDE was the antidote to stigma and discrimination – a rejection of the shame that others sought to impose on them.
Movements spearheaded by LGBTQ+ activists have driven much of the progress that has been made in protecting everyone’s human rights and protecting everyone’s health.
Today we are at a hinge moment: the end of AIDS as a public health threat is realisable in this decade, but progress is imperiled by the pushback on human rights.
At a time when support for human rights defenders is vital and urgent, funding support for civil society organizations is shrinking, as donor countries cut their budgets.
The evidence is crystal clear: stigma kills, solidarity saves lives.
This is a moment for solidarity. This is a moment for PRIDE.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Documents
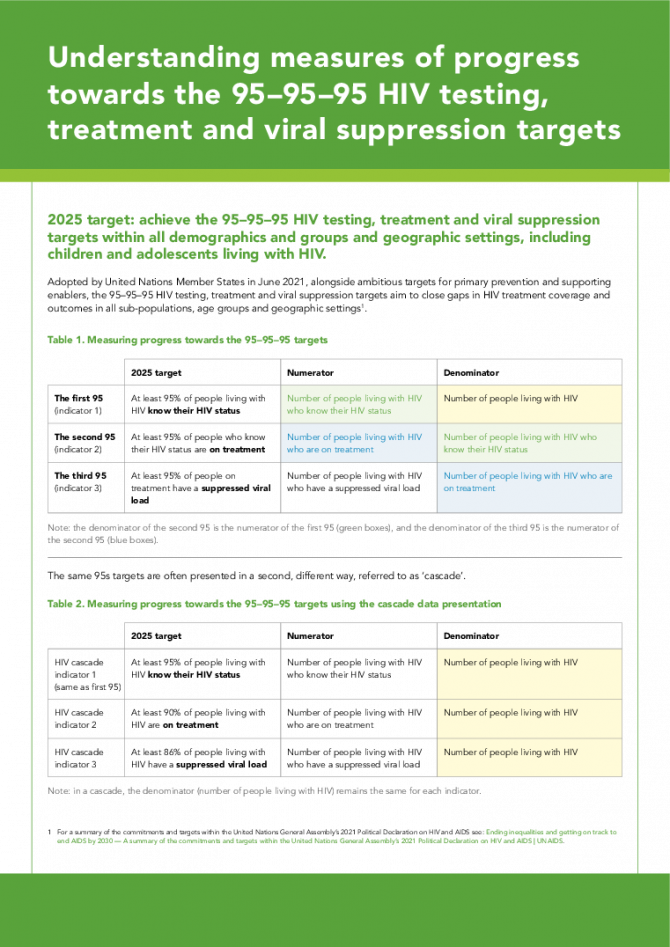
Understanding measures of progress towards the 95–95–95 HIV testing, treatment and viral suppression targets
11 March 2024
Adopted by United Nations Member States in June 2021, alongside ambitious targets for primary prevention and supporting enablers, the 95–95–95 HIV testing, treatment and viral suppression targets aim to close gaps in HIV treatment coverage and outcomes in all sub-populations, age groups and geographic settings.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025





Feature Story
How communities led in the HIV response, saving lives in Eswatini at the peak of a crippling AIDS epidemic
25 April 2024
25 April 2024 25 April 2024This story was first published by News24.com
Eswatini is one of the countries which has been most affected by HIV. At the peak of the epidemic in 2015, almost one out of three people were living with HIV. In 1995, when there was no antiretroviral treatment for people living with HIV, 73 000 people were living with HIV. 2400 people died of AIDS that year. Worried about the rising number of infections and deaths, communities of people living with HIV mobilized to press that antiretroviral treatment be made available for people living with HIV.
One of the key campaigners for access was Hannie Dlamini. Dlamini is now 50 years old and has been living with HIV for 32 years, after finding out about his HIV positive status at the age of 18. He was one of the first people in Eswatini to publicly declare his positive HIV status in 1995 at a time when the stigma and misinformation around HIV was rife.
Dlamini rallied together other people living with HIV as well as non-governmental organizations working to end AIDS in Eswatini, to ensure that everyone living with HIV and in need of treatment had access to it. They formed a community-led organization called Swaziland AIDS Support Organization (SASO) as a support group for people living with HIV. SASO also provided healthy living information for people living with HIV.
“When we asked the government [in 2002] for ARVs in Eswatini we did a pilot project with NECHA [National Emergency Response Council on HIV/AIDS], to see if people would use the drugs.” Dlamini says the response was overwhelming, with many people keen to start the lifesaving treatment. “We initially planned to enrol 200 people on treatment but the demand was 630.” said Dlamini.
Today, Eswatini is one of the countries which has achieved the ambitious 95-95-95 targets (95% of people living with HIV who know their HIV status, 95% of people who know that they are living with HIV are on life-saving antiretroviral treatment, and 95% of people who are on treatment are virally suppressed). This achievement has put the country a step closer to ending AIDS as a public health threat, thanks to the work of community-led organizations, authorities and global partners like UNAIDS, the United States President's Emergency Plan For AIDS Relief (PEPFAR) and the Global Fund to fight AIDS, TB and Malaria who are working with the government and local communities to end AIDS.
Eswatini’s HIV response strategy includes ongoing nationwide testing and treatment campaigns, use of self-testing kits to encourage more people to take up testing at the comfort of their homes, antiretroviral treatment, male circumcision and pre-exposure prophylaxis (medicine to prevent HIV) and other prevention measures. Community organizations such as Kwakha Indvodza are also key in encouraging men to take full responsibility for their wellbeing and reducing toxic masculinity and gender-based violence which are some of the drivers of HIV.
The driving role of communities in Eswatini to end AIDS is acknowledged by the health authorities. According to Dr. Michel Morisho, HIV management specialist at Mbabane Government Hospital, the government “could not have achieved the 95-95-95 without communities.”
Dr. Morisho says as part of the country’s strategy to end AIDS, HIV testing and treatment are part of disease management for every patient who presents at health facilities for any illness. “When people come to the hospital for whatever, or check up, we offer an HIV test to allow them to know their HIV status,” he said. Dr. Morisho added that treatment is important to bring down viral load and is helping people living with HIV to stay healthy. Eswatini is striving to achieve 100-100-100 [in the number of people who know their HIV status, are on treatment and are virally suppressed].” People who are virally suppressed cannot transmit HIV, thus helping in HIV prevention efforts.
Young women living with HIV have also stepped up to fight the spread of HIV in the country, volunteering their time as peer educators to educate young people about HIV and supporting people newly infected to stay on treatment to live healthily and long lives. Ntsiki Shabangu is a 28-year-old young woman living with HIV. She was diagnosed with HIV in 2015, at the age of 19. She opened up about her status in 2017 and is now working with the Eswatini Network of Young Positives, a local non-governmental organisation working to end AIDS among young people providing counselling and HIV awareness training . Ntsiki believes that: “When you share your story, you bring hope to young people.”
While Eswatini is on the path to end AIDS, the country is facing other health burdens associated with aging, including non-communicable diseases such as diabetes and cancer. People living with HIV are not often more affected by these illnesses. Some people living with HIV in Eswatini have developed these comorbidities, which presents the need for the strengthening of the healthcare system to provide easily accessible holistic disease management and treatment along with HIV services to improve the quality of life for people living with HIV. As Thembi Nkambule, a woman who has been on HIV treatment for more than 20 years said: “Most of us are sick. Most of us are presenting with kidney issues. We are presenting with hypertension; we are presenting with sugar diabetes. We have a lot of issues.”
To protect the gains that have been made against HIV in Eswatini, the government should invest more resources in building a resilient healthcare infrastructure to strengthen the system to better meet the health needs of people living with HIV and to prepare for future pandemics. Community-led organisations should also be placed at the centre of HIV response and supported, both financially and politically, to reach more people who need HIV services to end the epidemic by 2030 as a public health threat.
Region/country
Documents
A framework for understanding and addressing HIV-related inequalities
30 June 2022
This framework and its accompanying toolkit are designed to help the Joint Programme support countries and communities in their efforts to identify HIV-related inequalities and their drivers and to address them according to the Joint Programme’s comparative advantages and capacity—and, in doing so, support the full realization of human rights.
Related
 UNAIDS calls for rights, equality and empowerment for all women and girls on International Women’s Day
UNAIDS calls for rights, equality and empowerment for all women and girls on International Women’s Day

06 March 2025
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025




Press Release
UNAIDS urges Indian Ocean Island countries to strengthen HIV prevention to end AIDS
27 March 2024 27 March 2024ANTANANARIVO/GENEVA, 27 March 2024—Despite progress across most of sub-Saharan Africa, UNAIDS warns that gaps in HIV prevention are driving new HIV infections in the Indian Ocean Countries (IOC) and several other countries in Africa. The critical gaps in HIV prevention were the focus of a workshop organized by UNAIDS and UNFPA which was hosted in Madagascar between 18 and 20 March to address some of the barriers to accelerating progress.
Insufficient focus on HIV prevention in a number of African countries including Egypt, Madagascar, Angola, Sudan and South Sudan has resulted in these countries not achieving the proportionate declines in new infections seen in the rest of the region.
For example, the increase in the number of new infections in a country like Madagascar for example, is in stark contrast to the downward trend in Botswana which has seen a 66% decline in new HIV infections since 2010 and 36% decline in AIDS-related deaths during the same period. As a result, Botswana—along with Eswatini, Rwanda and Zimbabwe— are on the path to end AIDS having achieved the global 95-95-95 targets through strong HIV prevention and treatment interventions.
Madagascar, one of the poorest countries in the region, has been hit by cyclical natural disasters including drought and cyclones, making it difficult for the country to recover and mount an effective response to HIV. Madagascar recorded a 151% increase in the number of new HIV infections since 2010, and a 279% increase in AIDS-related deaths during the same period. In addition, just 18% of the estimated 70 000 people living with HIV in Madagascar had access to treatment in 2022, and 3200 people died of AIDS-related illnesses. Sudan and South Sudan are also falling behind on HIV prevention and treatment efforts. Inequalities are exacerbating people’s vulnerability to HIV.
“Local research indicates increases in new HIV infections among key populations, including people who use drugs, and among young women and girls. This could be attributable to many factors including drug routes, recurring cyclones and deep poverty in some areas that is making people more vulnerable to HIV infections,” said Professor Zely Randriamanantany, Madagascar’s Minister of Public Health. “We need our international partners to invest with us before it's too late. This prevention focus is very welcome indeed."
“It is clear from our visits to communities and from speaking to health specialists in Madagascar, that the HIV epidemic is changing. The persistent rise in new infections in Madagascar since 2010, for example, shows that it could spread rapidly if we do not stop it in its tracks immediately,” said Anne Githuku-Shongwe, UNAIDS Regional Director for Eastern and Southern Africa. “We know the path that ends AIDS. It’s not a miracle. It requires strong political and financial support.”
Gaps identified in some countries include a lack of data that would point to where HIV prevention efforts need to focus. Data gathering interventions are key to implementing evidence-informed and effective programmes. Some countries are also lacking commodities, including HIV testing kits and condoms.
“Inadequate investment in HIV responses is holding back ending AIDS as a public health threat,” said Jude Padayachy, UNAIDS Country Director for Comoros, Madagascar, Mauritius and Seychelles. “We need to accelerate the HIV response in the Indian Ocean Island states by ensuring all the basics—making sure people are informed about HIV and how to prevent it, and making sure people have access to HIV prevention services and commodities, such as condoms. We also need to make sure that people who are HIV-positive know their status and get the treatment they need.”
UNAIDS is committed to support countries to accelerate political leadership, investments and better data for prevention.
The meeting in Madagascar brought together HIV experts and programme leaders from a number of countries across Africa to learn from each other and to review and strengthen their national plans on HIV prevention to support countries in scaling up their HIV responses. The meeting included teams from Comoros, Egypt, Madagascar, Rwanda, Sudan and South Sudan.
Participants explored ways to improve data collection to help develop more of an understanding of the dynamics of their HIV epidemics to ensure an effective, evidence-informed, human rights-based response. They also drafted national assessments which will serve as a guide to facilitate dialogues with communities, governments, and partners. This will aid in refining strategies and setting priorities to implement ambitious HIV prevention plans. UNAIDS will continue to support countries in their internal assessments to strengthen their HIV responses.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS JohannesburgBathsheba OKWENJE
tel. + 27 (0) 72 895 5174
okwenjeb@unaids.org
UNAIDS Johannesburg
Robert SHIVAMBU
tel. +27 (0) 83 608 1498
shivambuh@unaids.org
Our work


Press Release
Reductions in new HIV infections in several Global HIV Prevention Coalition countries, but global progress needs to be accelerated
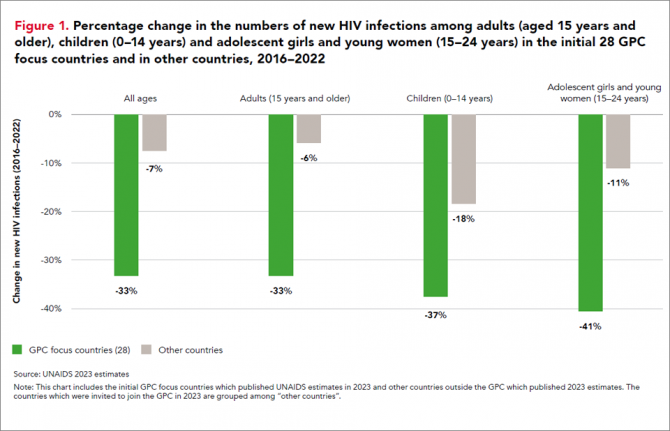
13 March 2024 13 March 202413 March 2024—A new report, HIV Prevention: From Crisis to Opportunity shows that HIV infections continue to decline in countries that are part of the Global HIV Prevention Coalition (GPC) faster than in the rest of the world.
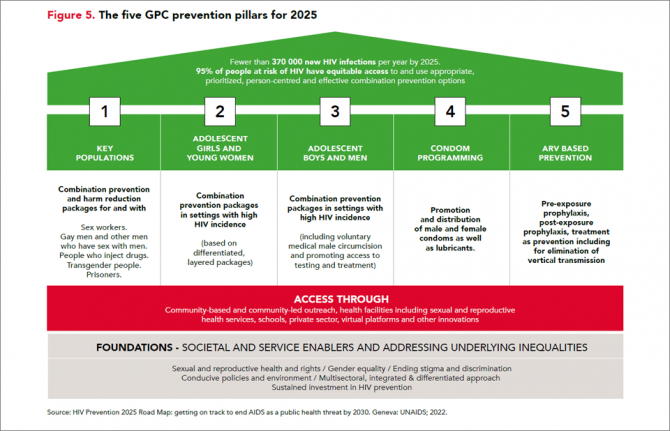
Eleven GPC focus countries have reduced their annual number of new HIV infections by at least 66% since 2010. By comparison, the average reduction in new HIV infections since 2010 globally is 38%. The GPC is a coalition of 38 countries working together to accelerate declines in new HIV infections to achieve the target of having 95% of the people who are at risk of HIV accessing effective combination prevention options.
The GPC countries that have prioritised primary prevention and treatment and that have focused on reaching people most at risk have secured the strongest consistent declines in new HIV infections.
Globally, progress in HIV prevention has been highly uneven and a majority of the world’s countries are not currently on track to achieve the 2025 targets. Indeed, several countries are experiencing prevention crises with low access to services and face record rising new HIV infections.
“The findings of this report offer crucial lessons for action,” said Angeli Achrekar, Deputy Executive Director Programme, UNAIDS. “The report shows that sustained political leadership, investment in effective HIV prevention programmes, and an enabling policy environment are crucial to end AIDS as a public health threat by 2030.”
Declines in new HIV infections have been boosted by the cumulative impact of combination HIV prevention options and increased access to antiretroviral treatment which has also increased viral suppression in people living with HIV. People who are on treatment and are virally supressed cannot transmit HIV.
“It’s remarkable to see what has been achieved in the AIDS response in the past 20 years. But the progress to date has not been equitable and is not yet sustainable, and we must never confuse progress with being sure of success,” said Mitchell Warren, GPC co-chair and Executive Director, AVAC. “Our progress is fragile, and what we’ve achieved today could slip away even more quickly than it was achieved if we let complacency take hold.”
Key populations and adolescent girls and young women are still at high risk of new infections
HIV incidence remains unacceptably high among populations where gaps in HIV prevention investments persist. This includes key populations in all regions globally and adolescent girls and young women in parts of sub-Saharan Africa.
Around 3100 young women and girls aged 15-24 became newly infected with HIV every week in sub-Saharan Africa in 2022 and HIV incidence declined less rapidly than it has among young men. Only 43% of the sub-national areas in which there is elevated HIV incidence among young women are being reached with dedicated prevention programmes for young women.
Although GPC countries have shown solid gains in reducing new HIV infections, challenges remain worldwide in reaching key populations most at risk of new HIV infections including men who have sex with men, sex workers and people who inject drugs. Every week, more than 11 000 new HIV infections occur among key populations and their sexual partners globally.
Only 44% of sex workers, 28% of gay men and other men who have sex with men, and 37% of people who inject drugs accessed two or more HIV prevention services in the previous three months according to median values reported by GPC countries ––against a target of 90%.
HIV prevention is being obstructed by shortfalls in prevention financing, and by punitive laws. Social stigma, violence, discrimination and social exclusion are barriers to key populations’ access to health-care services and information, exacerbating their risk of acquiring HIV. Law reform is a crucial enabler of prevention programmes. Protecting the human rights of everyone is vital for protecting the health of everyone.
Investments in both condom and voluntary medical male circumcision programmes, which are both effective in preventing HIV, have fallen in some of the countries with the largest HIV epidemics. In addition, breakthrough HIV prevention options such as pre-exposure prophylaxis (PrEP), medicine to prevent HIV, are still only available to a small fraction of the people who need them.
There are unprecedented opportunities for HIV prevention in 2024. There is a growing array of prevention options including existing tools and new long-acting prevention technologies, as well as country examples of how to implement prevention at scale and increase choices available to communities.
HIV Prevention programmes need to be at scale, efficient and equitable. The actions that are needed for success and sustainability are known, have been shown to work, and have been agreed: collaborate, follow science, tackle inequalities, protect everyone’s rights, let communities lead, and invest in what is needed. Sliding back on resourcing or inclusion would hurt everyone. Solidarity will benefit everyone. Communities, countries and international partners can prevent new infections – together.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work
Documents
HIV prevention: from crisis to opportunity — Key findings from the 2023 Global HIV Prevention Coalition scorecards
13 March 2024
The Global HIV Prevention Coalition focus countries are progressing unevenly towards the goal of reducing HIV infections to levels that would no longer constitute a public health threat. The biggest declines are occurring in eastern and southern Africa and, to a lesser degree, in western and central Africa. Expansion of access to effective ART, combined with an ongoing focus on primary prevention, are driving those achievements.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025




Feature Story
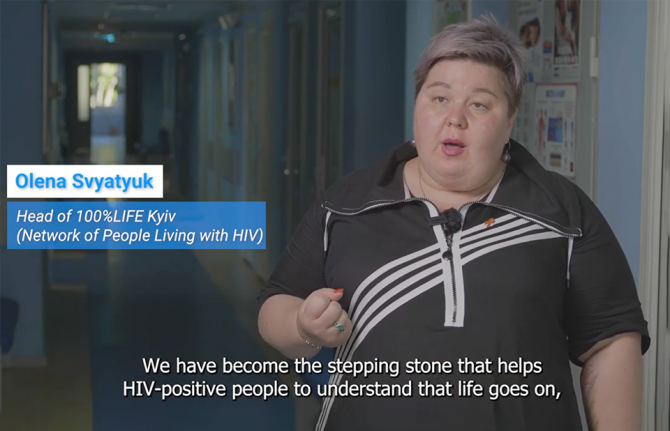
Two years on: UNAIDS supports Ukraine’s commitment to the HIV response
23 February 2024
23 February 2024 23 February 2024Two years of war in Ukraine have resulted in significant humanitarian consequences. Forty percent of the current population of Ukraine,14.6 million people, are in need of humanitarian assistance, 6.4 million refugees have fled the country, and more than 3 million people are internally displaced. People living with and affected by HIV continue to be vulnerable to the effects of the war, even as HIV services have been restored and are functional in most parts of the country.
Russian strikes have continued to wreak havoc on Ukrainian cities, causing death and destruction, impacting access to water, electricity, heating, and health services for millions of civilians.
In addition, there have been 1,570 attacks on health facilities and 630 health facilities damaged.
According to the latest data from The Ukrainian Public Health Center, prior to the war, Ukraine had made significant progress in reducing HIV incidence (-47%) and AIDS-related mortality (-81%) since 2010. Despite the initial disruption to the national AIDS response at the onset of the war, the national AIDS program has gradually resumed routine operations.
As of the end of 2023, the number of patients on antiretroviral therapy (ART) was only slightly below the pre-war figure, standing at 118,348 (130,724 as of February 2022). Additionally, approximately seven thousand patients are known to receive ART abroad. In the last two years, the number of patients on opioid agonist therapy (OAT) increased by 38%, reaching 27,511 people. Pre-exposure prophylaxis (PrEP) more than doubled, reaching 12,354 people.
However, in eastern and southern occupied territories data is incomplete or not available. This is true of Donetsk, Luhansk, Zaporizhzhia, Kherson regions, AR Crimea, and the city of Sevastopol. The same occurred in 2023. Despite these challenges, the surveillance system in the government-controlled areas remains operational, ensuring the completeness and quality of data on HIV prevention, testing and treatment services.
In addition, 9.6 million people in Ukraine are estimated to be at risk of or living with a mental health condition, and 3.9 million people are estimated to suffer from moderate to severe symptoms. And there has been an increase in gender-based violence.
Ukraine remains committed to the HIV response through a strong coalition of government, civil society, international organizations, and donors, first and foremost The United States President's Emergency Plan for AIDS Relief (PEPFAR) and The Global Fund to Fight AIDS, Tuberculosis, and Malaria. This collaboration has secured vital supplies of antiretroviral therapy (ARV), tuberculosis medicines, and opioid agonist therapy (OAT), ensuring uninterrupted HIV treatment and services.
UNAIDS Secretariat, Co-sponsors and UN agencies have joined forces to provide a unified response, ensuring that vulnerable populations, including those on the frontline and in the most severely affected areas, receive comprehensive support. This collaborative effort aims to bridge gaps and address the unique challenges faced by women, people living with HIV and key populations, including the delivery of crucial humanitarian aid and HIV services.
The past two years have been very challenging. Even though the country has managed to maintain HIV services, the unpredictability of what lies ahead has many fearing the worst. Support is needed to ensure sustainability of the AIDS response and to protect key populations affected by the enduring hardships of war.
For more information and more in-depth analysis, read the Situation Report (February 2024)