Events


Feature Story
Zero Discrimination Platform relaunched in Central African Republic
29 October 2021
29 October 2021 29 October 2021The goal of zero discrimination still eludes the Central African Republic. HIV-related stigma is pervasive in the lives of people living with HIV in the country. According to the 2018 People Living with HIV Stigma Index, discrimination affects almost all of the people living with HIV surveyed (more than 87%). And more than 45% of people living with HIV have experienced some form of stigma because of their HIV status. Stigma affects women (49%) more than men (37%).
“But the fight against HIV remains a public health priority for the government, which was the first country to join the Global Partnership for Action to Eliminate all Forms of HIV-Related Stigma and Discrimination, in December 2019,” said Marguerite Ramadan, the Minister of Gender Promotion, Women’s Protection, Family and Children, Central African Republic.
Since its engagement in the Global Partnership for Action to Eliminate all Forms of HIV-Related Stigma and Discrimination, the Central African Republic has implemented several key activities.
A memorandum of understanding was signed between the Ministry of National Defence and Reconstruction, the Ministry of Health and Population, the AIDS Control Council (CNLS) and UNAIDS to implement programmes aimed at eliminating gender-based violence and accelerating HIV prevention, treatment and care within the defence and security forces. A national charter of patients’ rights has been launched and is being disseminated progressively in health centres. A series of key human rights activities have been included in the Global Fund to Fight AIDS, Tuberculosis and Malaria’s grant for 2021–2023.
A Zero Discrimination Platform, composed of some 30 partners representing ministries, CNLS, United Nations agencies, technical and financial partners, civil society, human rights organizations and other organizations was launched in 2020 and is supporting these efforts, including through identifying synergies.
During the COVID-19 pandemic, initiatives have slowed down, so in order to relaunch the momentum of the Zero Discrimination Platform and agree on collective priorities for the end of 2021 and 2022, a validation workshop and launch of a joint workplan took place in Bangui, Central African Republic, on 28 October under the chairmanship of the Minister of Gender Promotion, Women’s Protection, Family and Children.
Priorities include the adoption of a revised law on HIV, the revision of training programmes for health professionals to include ethics and human rights, the signing of a memorandum of understanding between organizations of lawyers and networks of people living with HIV and key populations to provide free legal services and training on knowing your rights, the development of radio and television spots on discrimination issues and high-level advocacy for better integration of HIV issues in humanitarian interventions.
“The denial of health services to people living with HIV remains unfortunately common in the country, and the prevalence and effects of discrimination are often particularly severe for members of key populations, who face multiple and overlapping forms of discrimination,” said Marie Engel, Director, a.i., of the UNAIDS Country Office for the Central African Republic.
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Feature Story
Five questions about the HIV response in the Gambia
31 October 2021
31 October 2021 31 October 2021In the lead up to the West and Central Africa Summit on HIV/AIDS taking place in Dakar from 31 October to 2 November 2021, UNAIDS asked its country directors across the region five questions about the AIDS response in their country. Here are the replies of Ms. Sirra NDOW, UNAIDS country director in the Gambia
“Existing resources, skills and medical equipment designed for the HIV response proved essential to address COVID-19 when it emerged in the Gambia. Going forward, the country will need to refocus its efforts on providing tailored support to the most at-risk key populations which have often discontinued their treatment during the pandemic. Committing to the protection and fulfillment of their rights is the first crucial step.”
Similar to other western African countries, the Gambia has a low but highly concentrated HIV epidemic, affecting heavily key populations such as men who have sex with men and female sex workers. While impressive progress towards reducing new adult and paediatric infections have been observed in recent years, COVID-19 has caused a lot of complications. Repurposing HIV medical equipment and health personnel to address the fast-rising epidemic was necessary to limit COVID-19 related deaths. It also came with a cost—reducing the capacity to deliver HIV prevention and treatment services.
Lessons must be learned from the dual HIV/COVID-19 epidemics. Effort must be invested in better prevention services, especially tailored to key populations. Health personnel must be better trained and better supported to manage their workload and prevent bottlenecks. The approach of task shifting/sharing must continue and be further complemented by the strengthening of community health workers and decentralization of services. Finally, no progress will be truly radical unless stigma, discrimination and violence against people living with HIV and other marginalized groups are eradicated.
1. What are the main areas of progress in your country’s response to the HIV epidemic in the last five years?
The HIV epidemic in The Gambia mirrors those prevailing in other West African countries: the epidemic is overall low—less than 2% of the general population—but highly concentrated among key populations. The most recent Integrated Biological Behavioural Surveillance Study (IBBS.2018) estimates that prevalence is over 35% among men who have sex with men (MSM) and over 10% among female sex workers (IBBS 2018).
In 2018, the Gambia started implementing WHO’s recommendation to provide all people living with HIV with lifelong antiretroviral therapy (ART) regardless of clinical status or CD4 cell count. Between 2015 and 2020, impressive progress happened as new infections were cut by half and new infections among children were reduced by 75% (National AIDS Strategic Plan,2020-2025). All pregnant women attending antenatal clinics are routinely offered HIV tests, and all pregnant women living with HIV are eligible for ART (Option B+). Until the COVID-19 epidemic started, ART uptake had increased significantly. The country also adopted task shifting for HIV/AIDS and malaria—typically enabling nurses to dispense ART and capacitating community health workers to deliver a range of HIV services.
2. What are the main challenges that still need to be addressed?
Despite increased outreach activities, the testing coverage remains very low with less than 40% of the estimated PLHIV knowing their status. Inadequate investment in HIV prevention programmes and lack of access to prevention services, especially among key population groups, continue to impede progress in the national HIV response. HIV prevalence has increased more than three-fold among MSM from less than 10% in 2011 to over 35% in 2018 (IBBS, 2018) and no program have been designed to accelerate the uptake of pre-exposure prophylaxis as a prevention strategy among MSM.
HIV-related human rights and gender situation in the Gambia has not improved in the past five years. Key populations suffer multiple burden of frequent human rights violations, systematic disenfranchisement, stigma, and discrimination. The existence of punitive laws perpetuates barriers to accessing HIV services for key populations and further contributes to their social and economic marginalization. There remains lots to be done on promoting human rights literacy, putting in place mechanisms to monitor and report human rights violations, and advocate for policy reform and sensitization of lawmakers on human rights and gender-related issues.
Inadequately trained human resources for health coupled with frequent transfers of experienced and trained staff continue to threaten the national response. Decentralizing services, engaging community health services sites should be prioritized to further expand prevention, treatment, and care services. Finally, tracking patients at ART centres is a challenge due to inadequate cross-border programmes. There is need to strengthen cross-border initiatives to enhance follow-ups, defaulter tracing and referral of patients on treatment.
3. How has COVID-19 affected the HIV response in your country?
In the Gambia, there was no public health facility adequately equipped to treat COVID-19 cases and patients were treated at the Medical Research Council. There was no public health laboratory for COVID-19 testing, so health professionals repurposed PCR machines, which were originally intended for HIV testing, to test for COVID-19. HIV laboratory staff were also requested to provide COVID-19 services in addition to routine HIV and TB services While such urgent actions were required by the emerging pandemic, it led to a severe disruption in HIV diagnosis and the delivery of HIV and TB treatment services.
Social unrest caused by the COVID-19 pandemic also impeded access to regular healthcare, including for people living with HIV (PLHIV) and resulted in disruptions of ART availability. Rapidly, a multi-month dispensation of ARVs was initiated to try to maintain continued availability of treatment for all stable PLHIVs. During this period, a sharp decline in the number of PLHIV on ART was observed as well as a decline in HIV testing services in the general population.
4. Who are the unsung leaders of the AIDS response in your country?
We commend the admirable work delivered by community health workers in the Gambia, and the outstanding solidarity displayed by the community of people living with HIV.
5. If you could ask your Head of State to change one thing to strengthen the HIV response, what would it be?
To be a champion for the AIDS responses and to commit to mobilize adequate resources for the response.
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Feature Story
Five questions about the HIV response in Nigeria
31 October 2021
31 October 2021 31 October 2021In the lead up to the West and Central Africa Summit on HIV/AIDS taking place in Dakar from 31 October to 2 November 2021, UNAIDS asked its country directors across the region five questions about the AIDS response in their country. Here are the replies of Dr. Erasmus Morah, UNAIDS country director in Nigeria
“Recent years have been marked by positive trends when it comes to knowing the HIV epidemics. Thanks to better data, more efficient decisions were taken to address the needs of people living with HIV and place more than 80% of them on life-saving treatment. Going forward, we need to invest more efforts in domestic financing and protecting the rights of key populations.”
The National response in Nigeria is growing more ambitious and efficient—better information and high-level political commitment have led to increased antiretroviral therapy coverage. Communities, networks of people living with HIV and key populations are given more space to be actors in the response. The private sector is stepping up to play its part in funding the response.
Despite such effort, Nigeria is failing children living with HIV and vertical transmission is on the rise. Violent arrests are still routinely carried out against key populations. And user fees continue to impede access to HIV care and hinder adherence to treatment. Resilience in times of the COVID-19 epidemics gives hope that more effort will be invested to address these systemic barriers to truly turn the tide on HIV and end AIDS.
1. What are the main areas of progress in your country’s response to the HIV epidemic in the last five years?
First, the availability of data has expanded to enable the country to truly know its epidemic and its response. Several surveys took place since 2017 which provided precious support to national decision-makers to prioritize, track program performance and mobilize resources to end the epidemic.
In 2017, the Nigerian President committed to treating 50,000 Nigerians annually and has since honored his commitment. HIV treatment coverage has leapt from 55% in 2016 to over 85% in 2020. Currently, we estimated that 90% of people living with HIV (PLHIV) know their status, 86% of them receive antiretroviral therapy (ART), and among those, 72% have a suppressed viral load—meaning they have no risk of transmitting it.
To put communities at the centre of the response, the network of persons living with HIV and key populations are engaged in community-led monitoring to assess the quality of services they are receiving and to use data to influence policy and lead to programmatic changes.
To reduce Nigeria’s over reliance on international resources, the Nigeria Business Coalition Against AIDS has worked with the National Agency for the Control of AIDS (NACA) and UNAIDS to set up a trust fund of 150 million US dollars for HIV to be launched on World AIDS Day 2021. A sustainability plan is also being developed for HIV, tuberculosis and malaria.
2. What are the main challenges that still need to be addressed?
Unfortunately, children are still being left behind, and their treatment coverage remains much lower compared with adults. Only 45% of children living with HIV know their status, 45% of them receive antiretroviral therapy (ART), and among those, 31% have a suppressed viral load. It is sad to note that prevention of mother-to-child-transmission has been less effective over the past five years.
We continue to deplore the frequent arrest of key populations. Criminalization of the behaviour of key populations, violence and widespread stigma and discrimination continues to feed their avoidance of health care centers.
Finally, some health facilities are still demanding user fees from patient—despite evidence from western and central Africa showing that user charges undermine uptake of antiretroviral therapy, hinders the retention of people in care and reduce the quality of care. Studies specifically carried out in Nigeria have also shown that user fees undermine adherence to HIV treatment (Global AIDS report, 2020).
3. How has COVID-19 affected the HIV response in your country?
Despite the initial negative impact of lockdowns, the contingency measures put in place has ensured that Nigeria was able to successfully put about 300,000 people on treatment by the end of 2020. Through the one UN Basket Fund, about 10,000 households of PLHIV in needs were provided with cash transfers, personal protective equipment, and hygiene products to help prevent and mitigate the impact of COVID-19.
To ensure service continuity, the National AIDS and STI Control Program (NASCP) issued a policy directive from the Minister of Health for multi-month dispensing of ART, meaning that all clinically stable patients were provided with 3 months of treatment at once. NASCP set up a situation room to track HIV commodity stocks. Furthermore, NASCP regularly updated the UNAIDS HIV service disruption portal with programmatic data to monitor HIV service delivery during the COVID-19 pandemic. PLHIV networks provided home delivery ART services for their peers who could not access health services.
4. Who are the unsung leaders of the AIDS response in your country?
First, we need to recognize the outstanding work delivered by communities of key populations and networks of Persons Living with HIV in Nigeria. They truly are unsung heroes of the AIDS response. We also need to laud the support and commitment of international partners such as PEPFAR and the Global Fund.
5. If you could ask your Head of State to change one thing to strengthen the HIV response, what would it be?
I would call on Nigeria to take forward its commitments by investing its fair share in the AIDS response and by increasing domestic financing.
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Feature Story
Adapting to keep people living with HIV taking their treatment in the Central African Republic
31 October 2021
31 October 2021 31 October 2021To counter the low level of people living with HIV in Central African Republic (CAR) on treatment, the country has been testing new treatment approaches.
One is distributing up to 6 months of medicine, known as multi-month dispensing. The other is community ARV dispensation. CAR’s 2021-2025 National HIV Strategic Plan, identified these differentiated approaches at the community and hospital level and has been trying it out.
In the capital, Bangui, four pilots opened and 15 sites will progressively offer MMD (multi-month dispensing), health check-ups and community outreach thanks to funding from the Global Fund. This follows on the success of community-based treatment groups (CAGs) introduced by the Ministry of Public Health and Population and the National AIDS Control Council (CNLS) in 2015, with the support of the NGO Médecins Sans Frontières.
Certain community members deliver antiretroviral treatment to people living with HIV, especially in rural or conflict-stricken areas. Results showed that treatment intake was much more regular and people living with HIV had a rate of 75% viral suppression.
In addition, with UNAIDS support under a Luxembourg grant, the country has set up a steering committee to oversee the scale up of differentiated services, developed and validated national guidelines on the provision of differentiated services and two guides on multi month dispensing and the possibility of getting refills in a non-hospital setting.
At the end of October, clinicians, lab technicians, health care providers, community health care workers from the four pilot health centers participated in a workshop to go over the new approaches and guidelines. The CNLS and the country’s Division of Communicable Disease Control (DLMT) were confident adapting to the HIV epidemic in this way was a right step to keep patients on treatment. Currently, less than half of the people living with HIV take life-saving medicine (88,000-100,000 people live with HIV in CAR.)
Dr Marie-Charlotte Banthas from the DLMT said that "differentiated treatment models have demonstrated consistent improvement in patient engagement and retention of care, while freeing up time for the care of people with advanced disease.” She then added, ”It's a model of care for people living with HIV and staff working in the HIV field, a model of life."
These approaches came at the right time considering the lockdowns due to COVID-19, remarked UNAIDS CAR Country Director a.i. Marie Engel.
"With the long projected trajectory of the Covid pandemic, there is an even greater need to adapt the system to reduce service disruptions and not have recent gains in the HIV response stymied,” she said.
Region/country
Related


Opinion
How to end the AIDS epidemic in western and central Africa
31 October 2021
31 October 2021 31 October 2021By Winnie Byanyima, UNAIDS Executive Director
The AIDS epidemic in western and central Africa is an ongoing emergency. The early gains made against HIV in this region have not been translated into the sustained progress that has been made in other parts of sub-Saharan Africa.
Last year, there were 150 000 AIDS-related deaths in the region, and 200 000 people became newly infected with HIV. Every week more than 1000 adolescent girls and young women aged 15–24 years become infected with HIV in the region; 1.2 million people in western and central Africa are still waiting to initiate life-saving HIV treatment. Only 35% of children living with HIV in western and central Africa are on treatment.
Now the COVID-19 crisis has obstructed services and exacerbated the inequalities that drive the AIDS epidemic. If we don’t act now, not only will many more lives be lost, but containing the AIDS pandemic will be more difficult and expensive in the coming years.
Ending AIDS is achievable: there is a tested set of approaches that are proven to work, including in challenging settings.
From Cabo Verde’s leadership on the elimination of vertical transmission of HIV, to Cameroon’s decision last year to eliminate user fees for all HIV services at public health facilities and accredited community sites, examples that light the way are already there. By aligning policy with the evidence of what has succeeded, we can end AIDS as we promised.
Countries and communities are already leveraging the experience and expertise of the AIDS response to reduce the impact of COVID-19 across this region. From Côte d’Ivoire, to Guinea, to Senegal, public health authorities, international organizations, civil society actors and communities of people living with and affected by HIV have worked together to ensure that people living with HIV continue to receive their medication, to deliver care and prevention services in safe and innovative ways, to deliver food to people who have lost their incomes in lockdown, to convey messages about the importance of hygiene and social distancing in order to stay well and to dispel myths that feed stigma and discrimination and weaken public health messaging.
This spirit of cooperation and partnership is vital for stronger pandemic responses.
This week, hosted by the President of Senegal, Macky Sall, UNAIDS and the Civil Society Institute for HIV and Health in West and Central Africa are organizing a summit in Dakar on how to close the gaps in the region’s HIV response and strengthen pandemic preparedness.
Here are three of the bold actions we need to take.
First, embrace and enable communities to be at the centre of planning and delivery.
Communities know the situation on the ground—they must be given the resources and the space to lead. Countries need to ensure an enabling environment for communities to be involved in providing services as an integral part of the public health response, be involved as co-planners, be able to highlight experiences and concerns and be able to play their essential role ensuring accountability.
Countries need to lift those legal, policy and programmatic barriers that hold this back, and to scale up financial support to unleash the incomparable contribution of communities.
Second, increase investment.
Countries need to increase the scale of provision in prevention, testing and treatment and eliminate all financial barriers to ensure universal access to services.
The Abuja commitment to invest 15% of government budgets in public health needs to be met. Joint commitments made by health and finance ministers at the Africa Leadership Meeting to increase domestic revenues dedicated to health must be fulfilled.
International donors too have to step up with support at the time of the worst crisis in decades. Enabling the required fiscal space will require debt cancellation to support governments in scaling up investments in health and in tackling the social drivers of HIV and pandemic risk.
International action to prevent harmful tax competition and illicit financial flows is likewise key. It is difficult to advance towards fair and progressive taxation, and grow revenues, when large corporations and high-net-worth individuals are systemically enabled internationally to evade the taxes the ordinary citizen must pay, and which are essential for health, education, social protection and economic investment.
Third, address the inequalities that drive the epidemic.
COVID-19 has once again shown the world how epidemics thrive on inequalities, both between countries and within them. The new UNAIDS strategy adopted earlier this year puts the fight to end inequalities at the centre of the mission to end AIDS.
Inequalities drive HIV. Vulnerable groups of people represent 44% of new HIV infections in western and central Africa. Their partners represent a further 27%.
The ECOWAS Strategy for HIV, TB, Hepatitis B & C and Sexual and Reproductive Health and Rights among Key Populations puts it so well:
“the protection of human rights for all members of each key population is crucial to success. Laws that discriminate or create barriers should be reformed, to ensure that key populations are free from stigma, discrimination and violence and their vulnerability to HIV is reduced.”
Gender inequality likewise drives HIV: of the new HIV infections among young people in western and central Africa, almost three quarters are among adolescent girls and young women. The issue is power.
Research shows that ensuring that girls complete secondary education reduces their risk of acquiring HIV by up to half, and that combining this with a package of services and rights for girls’ empowerment reduces their risk further still.
The Education Plus initiative, co-convened by UNICEF, UNESCO, UNFPA, UN Women and UNAIDS, with governments, civil society and international partners, is helping to accelerate the actions and investments needed to ensure that every African girl is in school, safe and strong.
What we need to do to end AIDS is also what we need to do to enable Africa to rise.
Governments, international organizations, scientists, researchers, community-led organizations and civil society actors cannot be successful alone, but together they can create an unbeatable partnership and an unstoppable force to end AIDS as a public health threat by 2030.
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025




Update
Regional HIV summit aims to reinforce HIV response in Western and Central Africa
01 November 2021
01 November 2021 01 November 2021Delegations from 26 countries including 16 government ministers and representatives from civil society from the West and Central African region have formally opened the regional HIV summit, co-organized by UNAIDS and the Civil Society Institute of HIV and Health in West and Central Africa.
Following the welcome speeches, participants ranging from the heads of National AIDS councils to donors, the Global Fund and UNAIDS as well as their co-sponsors, began addressing the lagging HIV response in the region and how to overcome such setbacks.
The Western and Central Africa region represents only 8% of the world’s population but is home to more than 12% of all people living with HIV globally. In addition, 1 in 3 new HIV infections among children occur in this region with only 35% of children on treatment (vs 77% of adults.)
For Daouda Diouf, Executive Director of the Civil Society Institute of HIV and Health in West and Central Africa based in Dakar, a reset button must be activated to get HIV back on the agenda and further empower civil society.
“Our main expectation from the summit is to have civil society officially recognized as a key contributor in the countries within the official health systems and unofficial ones that the community health workers and civil society so aptly support,” he said.
Mr Diouf wants civil society to be on a more equal footing in the region and stressed that when community health workers, peer educators and civil society are involved, countries tend to have better health outcomes.
UNAIDS Fast Track Director a.i. Fodé Simaga agrees. Citing the fact that more than 65% of the new HIV infections in the region are among key populations and their partners, he believes civil society plays a crucial role with a specific added value.
“Considering the statistics, we rely on civil society and their networks to find people at risk of HIV, and reach out to them,” he said. He added that what is needed now is to reinforce their capacities.
“We can no longer consider civil society low-cost, ad-hoc health providers, they are an integral part of the healthcare systems that now need to be fully funded and supported,” Mr Simaga said.
Aside from advocating for civil society, a main session will focus on governments increasing domestic funding in the HIV response and another will be on the Education Plus initiative that stresses the importance of keeping girls and young women in secondary school. Additional break-out sessions will focus on HIV policies such as where and how to best distribute anti-retroviral pills, multi-month dispensing of medicine, prevention and combating stigma and discrimination.
The President of Senegal, Macky Sall, will close the three-day summit with a call to action from governments and civil society to close the gaps in the region’s HIV response.




Feature Story
Getting unconditional cash to marginalized households during COVID-19
29 October 2021
29 October 2021 29 October 2021COVID-19 has underscored the crucial need for pandemic responses to include social protection measures that reach and benefit marginalized populations.
As the pandemic swept across western and central Africa in early 2020, the region was already grappling with socioeconomic distress and humanitarian crises. Social restrictions imposed to contain the pandemic exacerbated those challenges. Impoverished and vulnerable populations, including people living with HIV and key populations, were hit hard.
Surveys conducted between June and August 2020 in 17 countries in the region on the situation and needs of people living with HIV—with support from UNAIDS, in partnership with the Network of African People Living with HIV West Africa—revealed that up to 80% of people living with HIV were experiencing livelihood losses, and more than 50% of them needed financial and/or food assistance.
These findings convinced UNAIDS and the World Food Programme (WFP) to launch a pilot project on unrestricted cash transfers in July 2020 to help people living with HIV and key populations cope with the socioeconomic impact of HIV and COVID-19 in four priority countries: Burkina Faso, Cameroon, Côte d’Ivoire and Niger. The initiative was designed to capitalize on WFP’s existing arrangements with service providers and on UNAIDS’ community engagement and relationships with civil society networks in the four priority countries.
Cash transfers are increasingly recognized as an effective form of social protection, with positive social and economic effects. They provide income support and help households avoid selling off assets or removing children from school, and they have multiplier effects on local economies. They constituted approximately 40% of global social safety net expenditures in 2018, but less than 20% in western and central Africa.
As the pandemic spread across western and central Africa, only a few countries (Côte d’Ivoire and Senegal among them) allocated additional support for vulnerable households in the form of cash transfers or social grants.
The immediate objective of the pilot was to reach about 5000 households with one-off, unconditional cash transfers, which ranged from US$ 88 per beneficiary (in Côte d’Ivoire) to US$ 136 (in Cameroon).
“I am so grateful for this support. I used it to pay the fees for my sewing course and to buy a sewing machine to start my own business. I also helped my mother who lost her job due to the pandemic,” said a young woman living with HIV in Cameroon.
Civil society organizations and financial service providers were engaged during the planning of the pilot. Eligibility for the transfers was decided based on a variety of vulnerability criteria, and beneficiaries were identified with the support of community-led organizations. Additional steps involved sensitizing beneficiaries, distributing the cash transfers, troubleshooting and monitoring the process. Specific attention was made to ensure confidentiality and to mitigate any potential stigma for beneficiaries.
Across the four countries, almost 4000 beneficiaries were reached, and it is estimated that a further 19 000 household members also benefited from the cash transfers, most of which went towards food, health care, education and housing expenses, or for income-generating activities. Country experiences varied in terms of the depth of their collaboration with community partners and the extent to which government actors were involved.
The experience of the pilot demonstrated that delivering rapid cash transfers to marginalized people living with HIV and key populations in very difficult circumstances is possible, and that it provides valuable emergency support.
Critical lessons learned include the need for inclusive and flexible approaches, working in ways that are clear and transparent to community partners and systematically involving community partners throughout the process. Defining clear and unbiased eligibility criteria, applying them consistently and sensitizing beneficiaries and communities are also vital.
Capacity-building and other support (including funding) for community partners is another critical element. Community-level organizations, trusted counsellors and peer educators were essential for establishing trust, identifying and reaching the intended beneficiaries, minimizing stigma and assessing the impact of the cash transfers. Engaging with government structures from the beginning helps to create the potential for long-lasting improvements.
One-off cash transfers of this kind can help households withstand short-term shocks, but they do not do away with the need to fully integrate vulnerable and marginalized populations into crisis responses and comprehensive social protection systems. It is imperative that countries across Africa expand inclusive, multipurpose social protection that is accessible and sustainable. Enhancing the people-centredness of cash transfers and slotting them in with other forms of social provisioning and support that are not necessarily cash-based—such as free or subsidized primary health care, education, water and energy—is part of this process.
Following this pilot experience on the use of cash transfers to support the most vulnerable people living with HIV and key populations, UNAIDS and the Civil Society Institute for Health have further strengthened their collaboration on advancing HIV-sensitive and inclusive social protection in western and central Africa. Recently they organized, with the support of LUXDEV funding and in collaboration with several UNAIDS Cosponsors, a capacity-building workshop to mobilize and build the capacity of civil society and communities and to promote dialogue and collaboration among civil society organizations, partners and governments to advance inclusive, HIV-sensitive social protection in the region.
Building on the recommendations of the workshop, a number of follow-up activities were agreed to enhance the role and positioning of communities in advancing HIV-sensitive social protection within their countries and the region.
“The cash transfer initiative in Niger came at the right time. The cash transfers were used by the beneficiaries to stockpile food and pay rent, but most importantly to allow the children to continue their schooling. This initiative demonstrated the value and importance of working together with the communities and our Cosponsors to achieve a common goal,” said El Hadj Fah, the UNAIDS Country Director for Niger.
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025

Update
Financial shortfalls hold back the HIV response in western and central Africa
25 October 2021
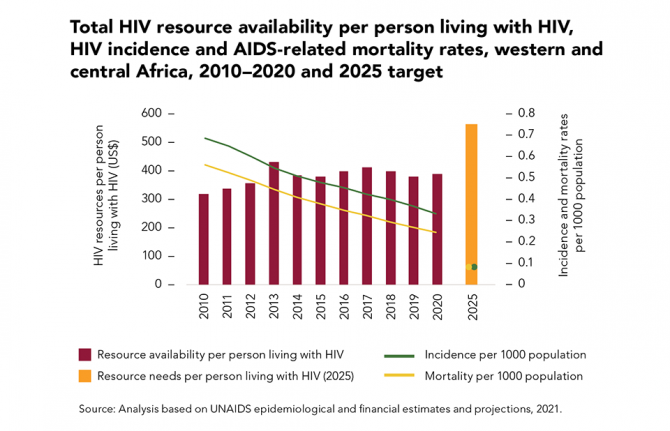
25 October 2021 25 October 2021Underinvestment in the HIV responses of low- and middle-income countries was a major reason why the global targets for 2020 were missed. Financial resource availability during the past five years was consistently below the resources needed, and in 2020 it was 29% less than the US$ 26 billion target for that year (in constant 2016 US dollars).
In western and central Africa, large resource shortfalls and continued reliance on out-of-pocket expenditures (such as user fees for health services) are associated with more modest declines in the incidence of HIV infection and the rate of AIDS-related mortality compared to eastern and southern Africa, where a combination of domestic and international investments has fuelled the rapid expansion of HIV prevention, testing and treatment in areas with a high burden of HIV, resulting in strong and steady reductions in the rate of HIV infections and AIDS-related mortality.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Feature Story
Launch of advocacy explainers on western Africa model drug law
28 September 2021
28 September 2021 28 September 2021Since the West Africa Commission on Drugs launched a groundbreaking model drug law in 2018, civil society across the region and beyond has been engaging stakeholders on the need to use the model law as a blueprint for national reform.
The model drug law promotes, among other things, the availability of harm reduction services as well as the decriminalization of possession of drugs for personal use, which have long been called for by UNAIDS.
As the model drug law is, by design, a long and technical document, UNAIDS supported the West Africa Drug Policy Network and the International Drug Policy Consortium to develop and disseminate two important new tools for civil society: a shorter and more accessible resource that summarizes the key points of the model drug law and a short guide for local nongovernmental organizations to explore how to use the model drug law in their work. In other words, the first advocacy explainer is about the key “ingredients” of the model drug law and the second contains a list of methods and strategies on how to use these ingredients to better integrate the law in their advocacy and to advance drug policy reform, based on experiences from the region.
The documents were launched on 27 September during a virtual webinar live on Facebook and can be found in English, French and Portuguese at https://www.wadpn.org/resources.
“These new tools will directly support and empower civil society advocacy for more health- and rights-based drug policies in western Africa and, in turn, strengthen the response to HIV among people who use drugs,” said Patrick Brenny, the Director of the UNAIDS Regional Support Team for West and Central Africa.
Adeolu Ogunrombi, a West Africa Commission on Drugs Commissioner, underlined that the needs and demands for drug dependence treatment and harm reduction are high, but service provision is low in the region, and specified that the law provides guidance on this. He also noted that criminalizing the possession of equipment and materials, such as needles, syringes and other paraphernalia, has been demonstrated to undermine harm reduction service provision and uptake and to have a damaging impact on public health.
A case study was presented by Chinwike Okereke, a civil society organization representative and focal point for the West Africa Commission on Drugs in Nigeria, on the use of the model drug law. In 2020, a coalition of civil society organizations made presentations on the model drug law to key policymakers, including the Federal Ministry of Justice, the Drug Law Reform Commission and the National Drug Law Enforcement Agency. “The model drug law presented an opportunity to have face-to-face discussions and drive a buzz on the reform that led to a drug law reform round table where all key federal, criminal justice and state actors and civil society made a case for the adoption of the law as a template for reform,” he said. Further engagement with the Drug Law Reform Commission then led to the setting-up of a working group that is actively working on reshaping drug laws in the country. He also encouraged civil society to use the new explainers and urged technical and funding partners to invest more funding for this effort across western Africa, as law reform takes some time to achieve.
Our work
Region/country


Feature Story
UNAIDS strongly supports calls for the rejection of draft law targeting LGBTI people in Ghana
12 August 2021
12 August 2021 12 August 2021UNAIDS fully backs calls made today by an eminent group of United Nations experts that Ghana should reject a proposed “family values bill” that targets the country’s lesbian, gay, bisexual, transgender and intersex community.
After analyzing the draft legislation, the independent experts appointed by the United Nations Human Rights Council concluded that adopting the legislation in its current or any partial form would be tantamount to a violation of a number of human rights standards, including the absolute prohibition of torture.
The experts said that the proposed law seeks to establish a system of State-sponsored discrimination and violence against the LGBTI community.
UNAIDS has already called for the law to be rejected as a gross violation of human rights. It has also warned that the legislation would be a grave setback for the HIV response in driving vulnerable people further away from essential HIV treatment, care and prevention services.
Ghana: Anti-LGBTI draft bill a “recipe for violence” – UN experts
GENEVA, 12 August 2021 — UN human rights experts* urged Ghana’s Government to reject a proposed ‘family values’ bill, saying it seeks to establish a system of State-sponsored discrimination and violence against the LGBTI community. The first reading of the bill took place on 2 August 2021, and its consideration is expected to resume in October 2021.
“The draft legislation argues that any person who deviates from an arbitrary standard of sexual orientation or gender identity is immediately to be considered dangerous, sick or anti-social,” said the experts. “Such laws are a textbook example of discrimination.
“The proposed law promotes deeply harmful practices that amount to ill-treatment and are conducive to torture, such as so-called ‘conversion therapy’ and other heinous violations like unecessary medical procedures on intersex children, and so-called corrective rape for women,” they added.
The independent experts, appointed by the Human Rights Council, presented an analysis of the draft bill to the Ghanaian Government, concluding that adopting the legislation in its current or any partial form would be tantamount to a violation of a number of human rights standards, including the absolute prohibition of torture.
For example, attempts to prevent human rights defenders from organising themselves to defend LGBTI people, and the absolute prohibition of public debate on sexual orientation and gender identity, raises grave concerns about rights to freedom of opinion and expression, and of association. Moreover, the bill in question would essentially legitimize the above instances of violence against LBTI women and reinforce existing gender stereotypes and discrimination against women, which are both cause and consequence of violence against women and girls.
“The consideration of this legislation is deeply perplexing in a country that has been regarded as a champion of democracy in Africa, with an impressive record of achieving certain Millennium Development Goals by 2015,” they said. They cited specific concerns about the MDG goals on health, education, employment, housing and gender justice.
“The draft legislation appears to be the result of a deep loathing toward the LGBTI community. It will not only criminalise LGBTI people, but anyone who supports their human rights, shows sympathy to them or is even remotely associated with them.
“Given that LGBTI people are present in every family and every community it is not very difficult to imagine how, if it were to be adopted, this legislation could create a recipe for conflict and violence.”
ENDS
*The experts: Victor Madrigal-Borloz, Independent Expert on protection against violence and discrimination based on sexual orientation and gender identity; Reem Alsalem, Special Rapporteur on violence against women, its causes and consequences; Koumbou Boly Barry, Special Rapporteur on the right to education; Irene Khan; Special Rapporteur on the promotion and protection of the right to freedom of expression; Mary Lawlor, Special Rapporteur on the situation of human rights defenders; Nils Melzer, Special Rapporteur on Torture and other Cruel, Inhuman or Degrading Treatment or Punishment; Tlaleng Mofokeng, Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health; Elina Steinerte (Chair-Rapporteur), Miriam Estrada-Castillo (Vice-chairperson), Leigh Toomey, Mumba Malila, Priya Gopalan, Working Group on arbitrary detention Clément Nyaletsossi Voule, Special Rapporteur on Rights to Freedom of Peaceful Assembly and Association
The Special Rapporteurs, Independent Experts and Working Groups are part of what is known as the Special Procedures of the Human Rights Council. Special Procedures, the largest body of independent experts in the UN Human Rights system, is the general name of the Council's independent fact-finding and monitoring mechanisms that address either specific country situations or thematic issues in all parts of the world. Special Procedures' experts work on a voluntary basis; they are not UN staff and do not receive a salary for their work. They are independent from any government or organization and serve in their individual capacity.
UN Human Rights, country page: Ghana
For more information and media requests please contact Catherine de Preux De Baets (+41 22 917 93 27/ cdepreuxdebaets@ohchr.org) or write to ie-sogi@ohchr.org
For media enquiries regarding other UN independent experts, please contact Renato de Souza (+41 22 928 9855 / rrosariodesouza@ohchr.org).
Follow news related to the UN's independent human rights experts on Twitter @UN_SPExperts.
Our work
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025