Data


Update
New HIV infections differ by sex and by region
08 June 2020
08 June 2020 08 June 2020In sub-Saharan Africa, where 61% of all new HIV infections occur, women are disproportionally affected by HIV, accounting for 54% of all new HIV infections in 2018. Young women aged 15–24 years were the hardest hit, accounting for 25% of new HIV infections in the region but representing only 10% of the total population.
Outside of sub-Saharan Africa, however, the situation is different, with men aged 25–49 years accounting for almost half of all new HIV infections, although they represent only 18% of the total population.
Our work
Related

Feature Story
Modelling the extreme—COVID-19 and AIDS-related deaths
25 May 2020
25 May 2020 25 May 2020Kimberly Marsh, a senior adviser on modelling and epidemiology, has worked for UNAIDS for six years. She supports countries in estimating the impact of the HIV epidemic globally and regionally.
Can you tell me more about the latest modelling report that you are a co-author of, which examines the potential for HIV service disruption in times of COVID-19 in sub-Saharan Africa?
This work looks at potential disruptions in sub-Saharan Africa owing to the COVID-19 pandemic on HIV services that might have an impact on HIV incidence—the number of new HIV infections—and on the number of AIDS-related deaths in excess to those we might have observed if we hadn’t had the COVID-19 pandemic.
We are particularly interested in those question because we know that more than two thirds of all people living with HIV worldwide are living in sub-Saharan Africa. That’s 25.7 million people living with HIV, 1.1 million new HIV infections and around 470 000 deaths from AIDS-related causes in 2018. Among all people living with HIV in the region, 64% of people are on life-saving antiretroviral therapy, which also prevents further new HIV infections.
It is really important that we’re able to ensure they will have access to services. In the models, we looked at service disruptions—a complete disruption of any HIV-related services over a three-month and a six-month period of time. And we looked at the impact after one year and five years. Now remember, these are just scenarios, and extreme ones. We don’t expect this to happen, but it helps us to answer two questions: what HIV-related services are most important to prevent additional deaths and new HIV infections and what might happen if we don’t mitigate or address those disruptions.
From this huge amount of work, what are the two key takeaways?
The modelling work predicted that with a six-month disruption in HIV treatment there could be an excess of 500 000 deaths in sub-Saharan Africa. So, when you look at UNAIDS estimates of AIDS-related deaths over time, that would take us back to about 2008, when we had nearly a million deaths.
There is no doubt about it, HIV treatment is critical. Ensuring that HIV treatment is available to people who need it during the three- to six-month periods is the most important thing that countries can do to prevent excess deaths and HIV incidence. All countries should work to ensure that supply chains are providing them with enough medicines to distribute and that people have sufficient medicines so that they can take them over the coming months.
The second thing to say is that these are projections and that there is still time to ensure that people get the HIV treatment services they need.
Let’s prevent what this model potentially predicts and let’s get HIV medicines to the people who are living with HIV.
What about HIV prevention? Does condom availability have an impact?
The models showed that when you look at prevention services, condom availability impacted the results. I think it is important to say that this is a treatment lesson primarily, but things like access to condoms is really important. We saw around a 20–30% relative increase in HIV incidence over one year if condoms were not available for six months. This is definitely something that we should be focusing on.
Can you tell us a little bit more about the impact on mother-to-child transmission of HIV in these scenarios?
In the scenarios, we looked at the potential for HIV testing services to be disrupted as well as for women to not get medicine to prevent transmission of HIV to their children. And what the various models found was that by removing those medicines—which have had an extremely important impact in terms of reducing new child HIV infections over the past five to 10 years—you could see rises in new child HIV infections in selected countries anywhere up to 162%. It really is critical to maintain prevention of mother-to-child transmission of HIV services.
You have said this was an extreme scenario, not a prophecy, but yet you still believe in modelling?
Models are very important for exploring questions that countries routinely pose to UNAIDS and the World Health Organization in terms of thinking of strategic approaches to responding to HIV in their countries. Models aren’t perfect, but they have a lot to tell us and I think in this instance it really highlights some of the strategies that will be important over the coming months as COVID-19 impacts or potentially impacts sub-Saharan Africa.
Related

Update
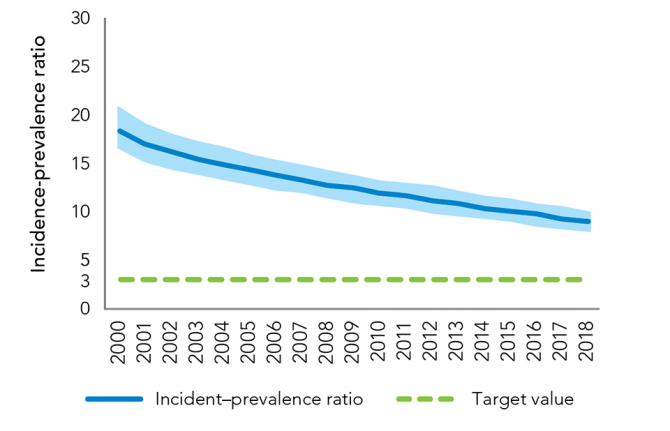
Wide differences in incidence–prevalence ratio by region
20 April 2020
20 April 2020 20 April 2020While important progress has been made against the global incidence–prevalence ratio—which, while declining from 11.2% in 2000 to 6.6% in 2010 and to 4.6% in 2018, still leaves the world not on track to end AIDS as a public health threat by 2030—the progress is uneven across regions.
Western and central Europe and North America, where treatment coverage is generally high and a comprehensive set of HIV prevention options is available to a large percentage of people at risk of HIV, had an incidence–prevalence ratio of 3.1% in 2018. Performance in other regions ranged from 3.9% in eastern and southern Africa, 4.6% in the Caribbean, 5.4% in both Latin America and Asia and the Pacific, 5.5% in western and central Africa, 8.0% in the Middle East and North Africa and 9.0% in eastern Europe and central Asia.
Resources

Update
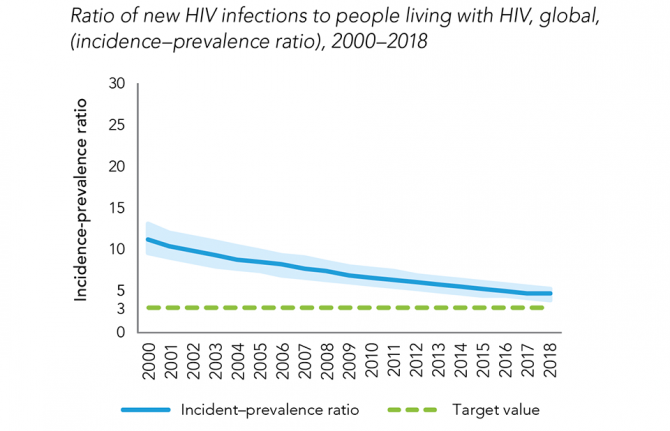
Ratio of new HIV infections to number of people living with HIV improving
14 April 2020
14 April 2020 14 April 2020Recent trends in new HIV infections and AIDS-related mortality can only show part of the story of the AIDS response. Epidemic transition metrics have been developed by UNAIDS and its partners as measures that countries can use to better track their progress towards ending AIDS as a public health threat.
One such metric, the incidence–prevalence ratio, uses the number of new HIV infections and the number of people living with HIV within a population. An epidemic transition benchmark of 3.0%—three HIV infections per 100 people living with HIV per year—corresponds to an average life expectancy after infection of 30 years. At this average life expectancy, the total population of people living with HIV will gradually fall if the country is below the 3% benchmark. The 3.0% benchmark thus combines two desirable conditions: long, healthy lives among people living with HIV and reductions in new infections.
The global incidence–prevalence ratio has declined from 11.2% in 2000 to 6.6% in 2010 to 4.6% in 2018, showing that important progress has been made against the HIV epidemic. Despite this, the world is not yet on track to end AIDS as a public health threat by 2030.
Resources
Related




Feature Story
HIV data check in Papua New Guinea’s National Capital District
06 March 2020
06 March 2020 06 March 2020For six weeks, two teams covered 12 HIV clinics on a data checking mission in Papua New Guinea. UNAIDS joined the country’s strategic information technical working group in the National Capital District, which includes Port Moresby, to inspect the clinics’ records to see if they match the records of the National Department of Health.
“The data quality assessment is part of the country’s HIV monitoring and evaluation plan to ensure the quality of data and reporting of the AIDS response,” explained Zimmbodilion Mosende, UNAIDS Papua New Guinea Strategic Information Adviser.
Led by USAID, the two teams of 12 branched out into smaller teams to look at the number of people registered as enrolled on antiretroviral therapy, the number of people newly starting treatment, the percentage of people returning for refills and the number of people who did not return to the clinics. In addition, the groups checked information on, for example, the age and sex of each person.
The volunteers from civil society groups, international nongovernmental organizations, development partners and key government offices went through the records of nearly 5000 people.
Papua New Guinea has the highest HIV incidence and prevalence in the Pacific region. The country of 8.4 million people represents 95% of the reported HIV cases in the region. There are approximately 45 000 people living with HIV in the country, of whom 65% are on antiretroviral therapy.
The groups tried to find out if there are discrepancies in the data and the reasons behind them. Albert Arija, Monitoring and Evaluation Specialist of USAID, described the reasons for discrepancies, which range from there being an inadequate number of staff, hence not enough time to fill out all entries, to incorrect data entry or at times misinterpretation of information. For fear of stigma and discrimination, some clients don’t want to give personal information.
One key missing data point was also birthdates. “Many people in Papua New Guinea cannot recall their exact date of birth,” said Mr Arija.
The technical working group is advocating for the use of electronic forms and real-time reporting. “Since the current antiretroviral therapy forms are still paper-based, there are several potential data quality risks, including human errors, from the data entry and processing,” Mr Mosende said.
Overall, most of the clinics had good quality data and processing, according to the teams’ assessment. They hope to simplify the overall process to scale up the data check for the whole country.
Related information
Region/country
Related
Documents
The response to HIV in Eastern Europe and Central Asia - Global AIDS update 2019
16 July 2019
The number people newly infected with HIV in eastern Europe and central Asia increased by 29% between 2010 and 2018. Key populations are disproportionately affected, and they lack access to the HIV services they need. Despite expanded HIV testing services, antiretroviral therapy coverage in the region is lower than in most other regions. Large proportions of people diagnosed with HIV are not being linked to HIV treatment and care.
Documents
Power to the people
04 December 2019
A new report by UNAIDS, Power to the people, released ahead of World AIDS Day, shows that where people and communities living with and affected by HIV are engaged in decision-making and HIV service delivery, new infections decline and more people living with HIV gain access to treatment. When people have the power to choose, to know, to thrive, to demand and to work together, lives are saved, injustices are prevented and dignity is restored.
Related
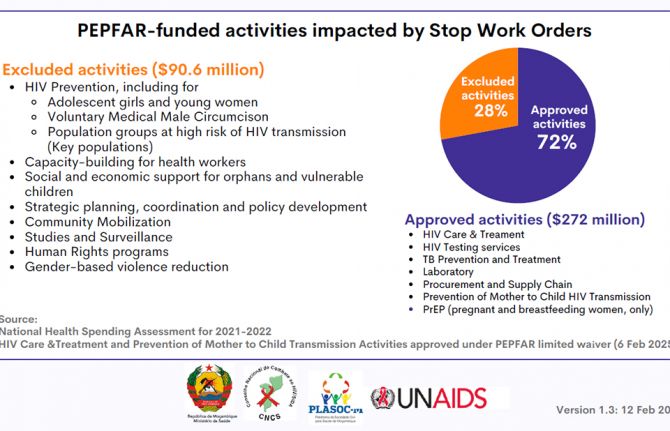
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Zambian football star Racheal Kundananji named UNAIDS Goodwill Ambassador for Education Plus in Zambia
Zambian football star Racheal Kundananji named UNAIDS Goodwill Ambassador for Education Plus in Zambia

23 January 2025
Documents
The response to HIV in Western and Central Africa — Global AIDS update 2019
16 July 2019
Some national HIV responses show improvement, but insufficient political will, frail health systems and weak support for community organizations hold back progress. Systemic barriers, including HIV-related criminalization and user fees, continue to deter large numbers of people from accessing HIV testing and treatment services. Many countries and communities in the region are fragile, affected by conflict, insecurity and humanitarian crises that create additional barriers to HIV responses.
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025
 Government mitigation measures in Cameroon
Government mitigation measures in Cameroon

09 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
UNAIDS data 2024
02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
 Empowering youth to lead Togo’s HIV response
Empowering youth to lead Togo’s HIV response

31 October 2024
Related
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
UNAIDS data 2024
02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
Domestic revenues, debt relief and development aid: Transformative pathways for ending AIDS by 2030, Report on Western and Central Africa
18 September 2024
Domestic revenues, debt relief and development aid: Transformative pathways for ending AIDS by 2030, Report on Eastern and Southern Africa
18 September 2024
UNAIDS information/guidance note on the mpox response
30 August 2024
Related
UNAIDS data 2024
02 December 2024
Slide deck - 2024 global AIDS update
22 July 2024
Core epidemiology slides
22 July 2024