40 years of the AIDS response
Data

27 September 2021
27 September 2021 27 September 2021New HIV infections among children declined by more than half (54%) from 2010 to 2020, due mainly to the increased provision of antiretroviral therapy to pregnant and breastfeeding women living with HIV. However, that momentum has slowed considerably, leaving particularly large gaps in western and central Africa, which is home to more than half of pregnant women living with HIV who are not on treatment.
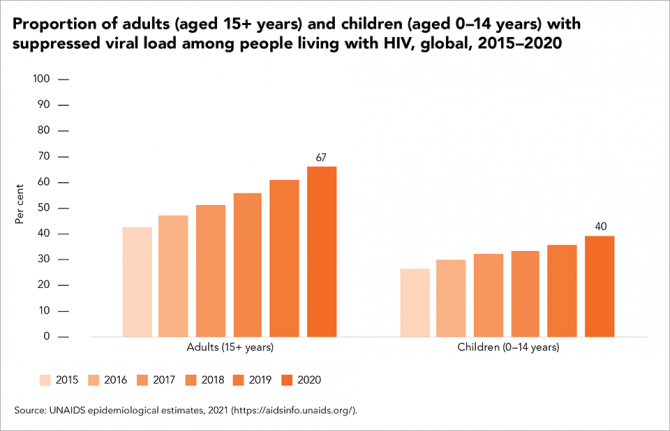
Gaps in the testing of infants and children exposed to HIV have left more than two fifths of children living with HIV undiagnosed. The number of children on treatment globally has declined since 2019, leaving almost 800 000 children (aged 0 to 14 years) living with HIV not on antiretroviral therapy in 2020. Just 40% of children living with HIV had suppressed viral loads, compared to 67% of adults. Nearly two thirds of children not on treatment are aged 5 to 14 years—children who cannot be found through HIV testing during postnatal care visits. A priority for the next five years is to expand rights-based index, family and household testing and to optimize paediatric treatment in order to diagnose these children, link them to treatment and retain them in life-long care.

27 February 2025
24 September 2021
This brief was developed following a consultation with members of the UNAIDS Scientific and Technical Advisory Committee (STAC) and other key stakeholders following the results from four community trials in Africa that showed decreased HIV incidence (by approximately 20–30%) and decreased HIV-related mortality (by approximately 20%) within three years of implementing a community-wide universal test and connect programme compared with current standard care.
Universal test and connect is an intensive community-wide strategy to accelerate HIV epidemic transition to rapidly reduce new HIV infections and deaths from AIDS-related illnesses across a specific community. This brief captures the highlights of the core findings of the STAC meeting and is focused on explaining universal test and connect in clear terms, with an emphasis on what it is and isn’t and on what to consider if a country is interested in implementing the approach at the subnational level. It also highlights the implications of the current and possible future COVID-19 contexts on opportunities for universal test and connect.
30 January 2025
21 January 2025

20 September 2021
20 September 2021 20 September 2021Progress against HIV has been uneven. The gains made through people-centred approaches within the highest performing HIV programmes have been tempered by insufficient action in other countries.
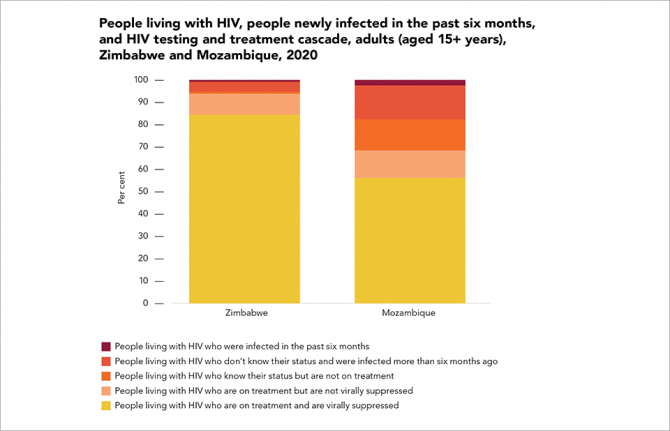
Zimbabwe has been an HIV testing and treatment leader. The southern African country’s AIDS Levy has mobilized a significant amount of domestic funding, communities are strongly engaged in service delivery and international financial and technical support has been strong and consistent. Eighty-two per cent of adults living with HIV in the country have suppressed viral loads. Neighbouring Mozambique, by contrast, has lagged behind the regional average, leaving nearly half (44%) of adults living with HIV in the country with unsuppressed viral loads. Conflict, climate change, high levels of poverty and poor health infrastructure are among the country’s many challenges.
08 July 2021
30 January 2025
21 January 2025
17 December 2024
17 December 2024
02 December 2024
26 November 2024

People living with HIV are at a higher risk of severe COVID-19 illness and death, yet the vast majority are denied access to COVID-19 vaccines. Key populations and their sexual partners account for 65% of new HIV infections but are largely left out of both HIV and COVID-19 responses—800 000 children living with HIV are not on the treatment they need to keep them alive
GENEVA, 14 July 2021—The UNAIDS Global AIDS Update 2021, launched today, highlights evidence that people living with HIV are more vulnerable to COVID-19, but that widening inequalities are preventing them from accessing COVID-19 vaccines and HIV services.
Studies from England and South Africa have found that the risk of dying from COVID-19 among people living with HIV was double that of the general population. In sub-Saharan Africa, which is home to two thirds (67%) of people living with HIV, less than 3% had received at least one dose of a COVID-19 vaccine by July 2021. At the same time, HIV prevention and treatment services are eluding key populations, as well as children and adolescents.
COVID-19 vaccines could save millions of lives in the developing world but are being kept out of reach as rich countries and corporations hold on tightly to the monopoly of production and delivery of supplies for profit. This is having a severe impact around the world as health systems in developing countries become overwhelmed, such as in Uganda, where football stadiums are being turned into makeshift hospitals.
“Rich countries in Europe are preparing to enjoy the summer as their populations have easy access to COVID-19 vaccines, while the global South is in crisis,” said Winnie Byanyima, Executive Director of UNAIDS. “We have failed to learn the lessons of HIV, when millions were denied life-saving medicines and died because of inequalities in access. This is totally unacceptable.”
The new UNAIDS report shows how COVID-19 lockdowns and other restrictions have badly disrupted HIV testing—in many countries this has led to steep drops in HIV diagnoses, referrals to care services and HIV treatment initiations. In KwaZulu-Natal, South Africa, for example, there was a 48% drop in HIV testing after the first national lockdown was imposed in April 2020. There were also fewer new HIV diagnoses and a marked drop in treatment initiation. This occurred as 28 000 HIV community health-care workers were shifted from HIV testing to COVID-19 symptom screening.
The report, Confronting inequalities, shows that in 2020 the 1.5 million new HIV infections were predominantly among key populations and their sexual partners. People who inject drugs, transgender women, sex workers and gay men and other men who have sex with men, and the sexual partners of these key populations, accounted for 65% of HIV infections globally in 2020. Key populations accounted for 93% of new HIV infections outside of sub-Saharan Africa, and 35% within sub-Saharan Africa. However, they remain marginalized and largely out of reach of HIV services in most countries.
The report shows that many of the 19 countries that achieved the 90–90–90 targets by 2020 have been leaders in differentiated service delivery, where facility-based services are complimented by community-led services. Most have also included key populations as central to their responses. In Estonia, for example, the expansion of comprehensive harm reduction services was followed by a 61% countrywide reduction in HIV infections and a 97% reduction in new HIV infections among people who inject drugs.
HIV testing and treatment has been scaled up massively over the past 20 years. Some 27.4 million of the 37.7 million people living with HIV were on treatment in 2020. However, gaps in service provision are much larger for children than for adults. In 2020, around 800 000 children aged 0–14 years who were living with HIV were not on HIV treatment. Treatment coverage was 74% for adults but just 54% for children in 2020. Many children were not tested for HIV at birth and remain unaware of their HIV status, making finding them and bringing them into care a major challenge.
Confronting inequalities also shows that women and girls in sub-Saharan Africa continue to be at a higher risk of HIV infection, with gender inequality and gender-based violence at the centre of that risk. Gender inequalities and gender-based violence rob women and girls of their fundamental human rights, including the right to education, health and economic opportunities. This increases their risk of HIV infection and blocks access to services. In sub-Saharan Africa, adolescent girls and young women account for 25% of all new HIV infections despite representing just 10% of the population.
Poverty and lack of schooling are also formidable barriers to health and HIV services. The report shows how family planning services for women and voluntary medical male circumcision for men and boys are much less likely to be accessed by people living in poverty. In 2020, the number of voluntary medical male circumcisions dropped by more than 30% in 15 priority countries in eastern and southern Africa.
Poverty is also a driver of migration, which has been shown to severely impact access to HIV services and puts lives in danger as migrants flee conflict and poverty in the hope of safety and economic security.
“Billionaires are sailing their yachts in the same Mediterranean waters that migrants are drowning in,” said Winnie Byanyima. “How can we stand by and let this be the “new normal”. We must confront these horrific inequalities and put the emphasis back on respect for basic, fundamental human rights.”
Inequalities are not naturally occurring. They are the result of policy and programmatic actions that divide rather than include. For example, key populations are marginalized and criminalized for their gender identities and expression, sexual orientation and livelihoods. New analysis included in the report shows a positive correlation between better HIV outcomes and the adoption of laws that advance non-discrimination. A study from sub-Saharan Africa found that HIV prevalence among sex workers was 39% in countries that criminalized sex work, compared to 12% in countries where sex work was partially legalized.
“We are 40 years into the fight against HIV. Both the successes and the failures have taught us that we cannot prepare for or defeat a pandemic unless we tear down inequalities, promote people-centred, rights-based approaches and work together with communities to reach everyone in need,” said Ms Byanyima.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.


25 June 2021
25 June 2021 25 June 2021Since key populations and their sexual partners account for 69% of new HIV infections in western and central Africa, reaching 95–95–95 among key populations will result in a significant impact on the overall HIV epidemic in the region. However, programmes focusing on key populations are insufficient. In western and central Africa, funding for programmes for key populations represented only 2.4% of the region’s overall HIV funding between 2016 and 2018, according to Frontline AIDS.
Having strategic information—quality data and analysis—is vital for an HIV response, for ensuring accountability and since it allows ambitious and measurable time-bound targets for monitoring progress to be set.
“The old adage “What gets measured gets done” may be a cliché, but it is still very true for the HIV response. Over the years, data collection, analysis and dissemination have led to a better understanding of the HIV epidemic and helped programmes to reach the right people in the right place at the right time,” said Marie Engel, Adviser at the UNAIDS Regional Support Team for Western and Central Africa.
In order to strengthen their skills in building and analysing data on the location and size estimates of key populations, approximately 30 people from four countries—Senegal, Côte d’Ivoire, Guinea and Guinea Bissau—and who were mainly from organizations for key population recently attended a training session in Saly, Senegal. During the training, which was part of a subregional project called RECCAP, funded by Expertise France, the Enda Santé nongovernmental organization, in collaboration with Johns Hopkins University, trained the participants on basic statistical analysis methods, population size estimation, health mapping tools and the analysis and presentation of collected data. UNAIDS and the World Health Organization sponsored the participation of several participants.
“The development of local capacities will allow for programmes that are best adapted to contextual changes by locating the dynamics of HIV vulnerability and analysing how sociospatial combinations influence epidemiological data. The diversity of the selected participants’ profiles and the plurality of the training team’s experiences guarantee a transfer of know-how and true sharing,” said Daouda Diouf, Enda Santé’s General Manager.
It is hoped that the training will empower key populations to exercise leadership—an essential mainstay of HIV responses to ensure that they are inclusive, equitable, effective, efficient and sustainable.

19 February 2025
23 June 2021
30 January 2025
21 January 2025
17 December 2024
02 December 2024
26 November 2024
18 September 2024
18 September 2024
30 August 2024
03 June 2021
After 40 years of AIDS, charting a course to end the pandemic. Read press release


UNAIDS urges world leaders to adopt a bold political declaration on HIV at the United Nations General Assembly High-Level Meeting on AIDS, being held in New York and online next week, and to commit to achieving a new set of targets for 2025 to end AIDS by 2030
NEW YORK/GENEVA, 3 June 2021—Four decades after the first cases of AIDS were reported, new data from UNAIDS show that dozens of countries achieved or exceed the 2020 targets set by the United Nations General Assembly in 2016—evidence that the targets were not just aspirational but achievable.
The report shows that countries with progressive laws and policies and strong and inclusive health systems have had the best outcomes against HIV. In those countries, people living with and affected by HIV are more likely to have access to effective HIV services, including HIV testing, pre-exposure prophylaxis (medicine to prevent HIV), harm reduction, multimonth supplies of HIV treatment and consistent, quality follow-up and care.
“High-performing countries have provided paths for others to follow,” said Winnie Byanyima, the Executive Director of UNAIDS. “Their adequate funding, genuine community engagement, rights-based and multisectoral approaches and the use of scientific evidence to guide focused strategies have reversed their epidemics and saved lives. These elements are invaluable for pandemic preparedness and responses against HIV, COVID-19 and many other diseases.”
Globally, the report shows that the number of people on treatment has more than tripled since 2010. In 2020, 27.4 million of the 37.6 million people living with HIV were on treatment, up from just 7.8 million in 2010. The roll-out of affordable, quality treatment is estimated to have averted 16.2 million deaths since 2001.
Deaths have fallen in large part due to the roll-out of antiretroviral therapy. AIDS-related deaths have fallen by 43% since 2010, to 690 000 in 2020. Progress in reducing new HIV infections has also been made, but has been markedly slower—a 30% reduction since 2010, with 1.5 million people newly infected with the virus in 2020 compared to 2.1 million in 2010.
The report underscores that countries with punitive laws and that do not take a rights-based approach to health punish, ignore, stigmatize and leave key populations—which make up 62% of new HIV infections worldwide—on the margins and out of reach of HIV services. For example, almost 70 countries worldwide criminalize same-sex sexual relationships. Gay men and other men who have sex with men, sex workers, transgender people, people in prison and people who inject drugs are left with little or no access to health or social services, allowing HIV to spread among the most vulnerable in society.
Young women in sub-Saharan Africa also continue to be left behind. Six out of seven new HIV infections among adolescents aged 15–19 years in the region are among girls. AIDS-related illnesses remain the leading cause of death among women aged 15–49 years in sub-Saharan Africa.
COVID-19 has shown the fragility of the health and development gains made over the past decades and has exposed glaring inequalities. To get the world on track to end AIDS by 2030, the global AIDS community and UNAIDS have used an inequalities lens to develop an ambitious and achievable strategy with new targets to reach by 2025. Ending inequalities requires HIV responses that can reach the populations currently being left behind.
If reached, the targets will bring HIV services to 95% of the people who need them, reduce annual HIV infections to fewer than 370 000 and AIDS-related deaths to fewer than 250 000 by 2025. This will require an investment of US$ 29 billion a year by 2025. Each additional US$ 1 of investment in implementing the global AIDS strategy will bring a return of more than US$ 7 in health benefits.
UNAIDS urges the United Nations General Assembly to commit to the targets in a new political declaration on HIV at the fifth United Nations General Assembly High-Level Meeting on AIDS, taking place from 8 to 10 June 2021.
“The world cannot afford to underinvest in pandemic preparedness and responses,” said Ms Byanyima. “I strongly urge the United Nations General Assembly to seize the moment and commit to taking the actions needed to end AIDS.”
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.