Data

Update
People who use drugs: still being left behind
18 March 2019
18 March 2019 18 March 2019While the incidence of HIV infection globally for all ages declined by 22% between 2011 and 2017, HIV infections among people who inject drugs appear to be rising. HIV incidence—the number of new HIV infections among a susceptible population during a certain time—among people who inject drugs rose from an estimated 1.2% in 2011 to 1.4% in 2017.
There is compelling and comprehensive evidence that harm reduction—including opioid substitution therapy and needle–syringe programmes—prevents HIV infections among people who inject drugs. However, criminalization of drug use and possession for personal use and the widespread stigma, discrimination and violence faced by people who use drugs hampers access to health and harm reduction services.
In its new report, Health, rights and drugs: harm reduction, decriminalization and zero discrimination for people who use drugs, UNAIDS has outlined a set of recommendations for countries to adopt for a public health and human rights response to drug use.
Related information
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025


Press Release
New survey results indicate that Nigeria has an HIV prevalence of 1.4%
14 March 2019 14 March 2019Expanded data collection and analysis provides better understanding of HIV epidemic in Nigeria
ABUJA/GENEVA, 14 March 2019—Results released today by the Government of Nigeria indicate a national HIV prevalence in Nigeria of 1.4% among adults aged 15–49 years. Previous estimates had indicated a national HIV prevalence of 2.8%. UNAIDS and the National Agency for the Control of AIDS estimate that there are 1.9 million people living with HIV in Nigeria.
Speaking in Abuja, Nigeria, the President of Nigeria, Muhammadu Buhari, welcomed the news that there are fewer people living with HIV in the country than previously estimated and launched the Revised National HIV and AIDS Strategic Framework 2019–2021, which will guide the country’s future response to the epidemic. Nigeria has made good progress in scaling up HIV treatment and prevention services in recent years.
"For the first time, the end of AIDS as a public health threat by 2030 is truly in sight for our country,” said H.E. Muhammadu Buhari, President of Nigeria. “I urge all of us not to relent but to increase the momentum. Let us work collectively and push for the last mile.”
The data from the Nigeria National HIV/AIDS Indicator and Impact Survey (NAIIS) are based a revised and enhanced methodology. The survey provides a clearer understanding of Nigeria’s HIV epidemic and shines a light on progress and the remaining gaps and challenges.
The Executive Director of UNAIDS, Michel Sidibé, welcomed the new estimates and said the improved understanding of the country’s HIV epidemic would allow Nigeria to better reach people living with HIV and people at higher risk of acquiring HIV.
“I commend the Government of Nigeria and its partners for conducting this ambitious survey, which provides us with a much better understanding of the country’s HIV epidemic,” said Mr Sidibé. “While it is fantastic news that there are fewer people living with HIV in Nigeria than previously thought, we must not let down our guard. Let us use the results of this survey to better focus our delivery of HIV prevention, treatment and care services to the people in the greatest need and ensure that Nigeria gets on track to end the AIDS epidemic by 2030.”
While Nigeria’s national HIV prevalence is 1.4% among adults aged 15–49 years, women aged 15–49 years are more than twice as likely to be living with HIV than men (1.9% versus 0.9%.) The difference in HIV prevalence between women and men is greatest among younger adults, with young women aged 20–24 years more than three times as likely to be living with HIV as young men in the same age group. Among children aged 0–14 years, HIV prevalence according to the new data is 0.2%. Significant efforts have been made in recent years to stop new HIV infections among children.
At the national level, viral suppression among people living with HIV aged 15–49 years stands at 42.3% (45.3% among women and 34.5% among men). When people living with HIV are virally suppressed they remain healthy and transmission of the virus is prevented.
The improved understanding of the country’s HIV epidemic will allow for more efficient investments in the response to HIV and more effective planning for the provision of HIV prevention, care and treatment services, including a focus on key populations, such as female sex workers. It will permit the adoption of a population–location approach to deliver services to the people and areas where they are most needed.
The new data differentiate HIV prevalence by state, indicating an epidemic that is having a greater impact in certain areas of the country. The South-South zone of the country has the highest HIV prevalence, at 3.1% among adults aged 15–49 years. HIV prevalence is also high in the North Central zone (2.0%) and in the South East zone (1.9%). HIV prevalence is lower in the South West zone (1.1%), the North East zone (1.1%) and the North West zone (0.6%).
“The Nigeria National HIV/AIDS Indicator and Impact Survey (NAISS) findings provide Nigeria with an accurate national HIV prevalence measure of 1.4%. NAIIS also showed we are able to effectively provide antiretroviral treatment,” said Isaac F. Adewole, Nigeria’s Minister of Health. “Everyone infected with HIV needs to get treatment so they can achieve viral suppression, especially pregnant women. We must ensure pregnant women have access to antenatal services and are tested during every pregnancy. We know we can support HIV-positive mothers, hence ensuring the next generation is free from HIV.”
Nigeria has shown steady progress on increasing access to treatment for people living with HIV, with the adoption of a test and treat policy in 2016. This measure has further accelerated referrals to treatment facilities for people who test positive for the virus. From 2010 to 2017, the country almost tripled the number of people living with HIV having access to antiretroviral therapy, up from 360 000 people in 2010 to more than 1 million people in 2018. However, the new estimates released today indicate that more than half of people living with HIV still do not have suppressed viral loads.
The new data are more accurate as they are based on an expanded surveillance system and a revised and enhanced methodology. In recent years, there has been a significant expansion in the country’s response to HIV. The number of sites providing treatment has more than tripled, the number of sites providing services to prevent mother-to-child transmission of HIV has increased eightfold and the number of HIV counselling and testing sites has increased fourfold. A total of 11.3 million adults were counselled and tested for HIV in 2016, four times as many as in 2012.
“It is important that all people living with HIV get treatment and achieve viral suppression. To halt the epidemic, we need to act now,” said Sani Aliyu, Director-General of the National Agency for the Control of AIDS. “As a government working with our partners, we have what it takes to support people who are HIV-positive, to provide treatment, to protect their families and to help people live long and healthy lives.”
The NAIIS was led by the Government of Nigeria through the Federal Ministry of Health and the National Agency for the Control of AIDS. UNAIDS, the United States President’s Emergency Plan for AIDS Relief and the Global Fund to Fight AIDS, Tuberculosis and Malaria provided support for the work on the survey, which was overseen by the United States Centers for Disease Control and Prevention and implemented by the University of Maryland, Baltimore, with a scope that included all 36 states and the Federal Capital Territory of Nigeria. The survey reached around 220 000 people in about 100 000 households. Fieldwork was conducted between July and December 2018.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Federal Ministry of Health (FMOH)
Federal Ministry of Health is one of the Ministries in the Federal Republic of Nigeria. It is concerned with the formulation and implementation of policies related to health. The Ministry has several departments focusing on different aspects of health care. The Department of Public Health’s National HIV and STI Control Program (NASCP) participated in the conduct of NAIIS and guided its implementation. More information can be found at http://www.health.gov.ng/
National Agency for the Control of AIDS (NACA)
The National Agency for the Control of AIDS was established to coordinate the various activities of HIV/AIDS in the country. The Agency among several functions coordinate and sustain advocacy by all sectors and at all levels for HIV/AIDS/STDs Expanded Responses in Nigeria. The Agency in collaboration with the FMoH guided the implementation of NAIIS. More information can be found at https://naca.gov.ng/ for more information about NACA.
Contact
UNAIDSMichael Hollingdale
tel. +41 22 791 5534 / +41 79 500 21 19
hollingdalem@unaids.org
UNAIDS Media
tel. +41 22 791 42 37
communications@unaids.org
Press centre
Download the printable version (PDF)
Region/country

Update
HIV prevention: not hitting the mark
11 March 2019
11 March 2019 11 March 2019The number of new HIV infections globally continues to fall. Modelled estimates show that new infections (all ages) declined from a peak of 3.4 million [2.6 million–4.4 million] in 1996 to 1.8 million [1.4 million–2.4 million] in 2017—the year for which the most recent data are available. However, progress is far slower than that required to reach the 2020 target of fewer than 500 000 new HIV infections (see graph below).
Related information


Update
The disproportionate impact of HIV on women in western and central Africa
25 February 2019
25 February 2019 25 February 2019Women are disproportionality affected by HIV, particularly in sub-Saharan Africa. However, in some countries the imbalance is severe.
According to data collected in the Demographic and Health Surveys 2009–2017—a programme that collects and disseminates data on health and populations in developing countries—in the past decade HIV prevalence has been up to three times higher among 20–29-year-old women than men in some of the countries with the highest HIV burden in western and central Africa: Cameroon, Côte d’Ivoire and Ghana (see graph below).
Data for 20–29-year-olds show the importance of HIV transmission through sex. Since men tend to start having sex at an older age than women, data for people who are 20–29 years old better cover both sexually active women and sexually active men. It is clear that women in the region are not being reached with the range of HIV prevention options they need to stop them becoming infected with HIV through sex.
With the ongoing drive in western and central Africa to match the progress made against HIV in eastern and southern Africa, there is a vital need for awareness of the disproportionate impact that the HIV epidemic has had, and continues to have, on women in the region.
Related information




Feature Story
With UNAIDS’ support, everyone counts
28 January 2019
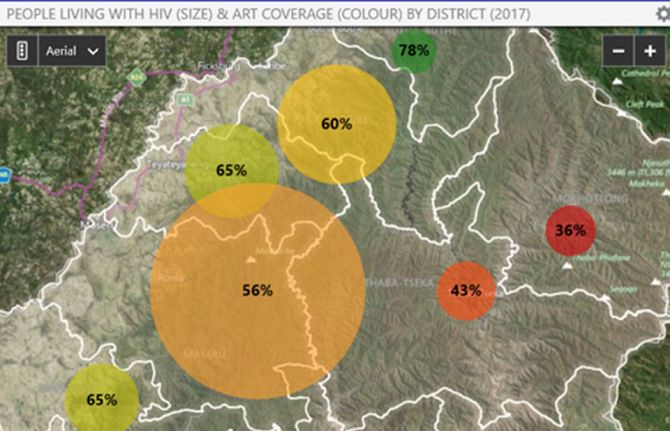
28 January 2019 28 January 2019For five weeks in 2018, teams of up to 10 people in each of 120 clinics and hospitals across Lesotho sifted through more than 180 000 records of people diagnosed with HIV and receiving care. The goal: to count the number of people living with HIV who were on treatment in June 2018.
During the long and dusty days, the teams attached green stickers—indicating active on treatment—or other coloured stickers—specifying that a person had defaulted, transferred or died—to nearly 80% of all patient files in the country. Facility by facility, counts of the number of people found to be active on treatment were compared to counts previously reported to the Lesotho Ministry of Health and other partners, including the United States President’s Emergency Plan for AIDS Relief. All of this to confirm that the country’s reporting adds up.
“Together with our team, we reviewed the treatment status of more than 5000 people at the Senkatana Clinic in Maseru, Lesotho, one of the oldest and busiest treatment centres in the country. After two days of reviewing the paper-based files, we found about 30% more people on treatment than the clinic had reported to the Ministry of Health in June 2018,” said Motselisi Lehloma, Ministry of Health Officer. Overall, the exercise found an underreporting to the Ministry of Health of 3% for all the 120 facilities visited.
Since early 2017, UNAIDS and other international partners have supported more than 15 countries, primarily in sub-Saharan Africa, to verify that the number of people reported currently to be on treatment is accurate. This work also supports facilities to improve the accuracy of the data reported through their health information systems by reviewing patient registries and processes for collecting, aggregating and reporting treatment numbers.
“The exercise that Lesotho undertook to audit and validate treatment numbers underscores its commitment to accurately monitor programme impact,” said Kim Marsh, Senior Adviser, Epidemiology and Monitoring, UNAIDS. Thanks to these efforts, and the efforts of many other countries in the region, UNAIDS and stakeholders can be confident in treatment numbers that allow us to monitor progress towards 90–90–90. Through debriefings with clinical staff and written reports, minor deficiencies were addressed on the spot and larger systematic issues were brought to the attention of the ministry and implementing partners in order for them to adopt necessary corrective actions.
Lesotho has one of the highest burdens of HIV in the world. In 2017, 320 000 people were living with HIV in the country, an HIV prevalence of 23.8%.
Region/country


Feature Story
New data dashboard launched in the Asia and the Pacific region
02 November 2018
02 November 2018 02 November 2018A new data dashboard to enhance the HIV strategic information products that were already available on the AIDS Data Hub for the Asia and the Pacific region was launched on 30 October.
Developed by UNAIDS, the platform allows users to visualize data and indicators related to HIV epidemiology and the AIDS response in the region through customizable maps, graphs, tables and fact sheets by indicator, country and key population. It also facilitates integrated analysis and gives access to granular data. The data dashboard is a one-stop shop that offers HIV-related strategic information, data analysis products and reference documents.
“With concrete targets to be met on the way to end the AIDS epidemic by 2030, it is vital to have the right data tracking whether the Asia and the Pacific region is on course to meet the commitments made in the 2016 United Nations Political Declaration on Ending AIDS. Data show us how far we have come and how far we have to go,” said Eamonn Murphy, Director of the UNAIDS Regional Support Team for Asia and the Pacific.
Accurate and credible data on the HIV epidemic are the cornerstone of the AIDS response. Over the years, a detailed understanding of the HIV epidemic has been built up through the collection, analysis and dissemination of data, helping programmes to reach the right people in the right place and at the right time. Having high-quality data on the AIDS response coupled with cutting-edge analysis has been critical for countries to track their progress towards ending the AIDS epidemic.
UNAIDS and the Data Hub team work with all the countries in the region to collect and analyse data on their AIDS responses and to help build their capacity to generate and use strategic information. In the region, no major report, speech or policy initiative on HIV is launched or made without referring to data collected and released by UNAIDS.
The Data Hub team works closely with civil society, particularly on strengthening the capacity of young community members on data literacy and the interpretation and use of data. “Research and data, coupled with the lived experience of our community, provide the evidence we need for an effective response to HIV. The AIDS Data Hub is an essential tool for helping community-based HIV workers across the Asia–Pacific region access relevant research and data to amplify their advocacy for better services, more funding and the scaling up of programming,” said Midnight Poonkasetwattana, the Executive Director of APCOM.
Asia Pacific AIDS Data Hub
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025




Feature Story
Smithsonian exhibition features UNAIDS data in a look at various viruses
21 August 2018
21 August 2018 21 August 2018An infectious disease can spread around the world in days. Human factors that have quickened the pace of virus transmission include the growing global population, urbanization and the industrialization of food production. The Smithsonian’s National Museum of Natural History in the United States of America features nine diseases that have spilled over from animals to humans in its newly opened exhibition, Outbreak: Epidemics in a Connected World.
One hundred years after the influenza pandemic, the three-year-long exhibition sheds a light on the causes of disease outbreaks such as Nipah virus and severe acute respiratory syndrome (SARS) and the various responses to epidemics.
“The 2014 Ebola outbreak in western Africa was the catalyst, but we wanted to have HIV—the pandemic of our time—as a big focus of the exhibition,” said Sabrina Sholts, the lead curator. For HIV, the museum created a three-dimensional timeline showing the landmarks of the AIDS response in the United States, from the activism to the science to the policy changes and treatment. Objects such as red ribbon pins, ACT UP T-shirts with a pink triangle with the saying Silence=Death, condoms, antiretroviral medicine bottles and photos guide visitors from the start of the HIV epidemic until now. A large touch table allows for people to explore new infections around the world today based on the latest UNAIDS data.
“We didn’t want to leave the impression that AIDS is over and limited to one place, so the interactive component resonates with people as to where we stand right now,” said Ms Sholts.
The UNAIDS Strategic Information Department worked with Ms Sholts’ team and provided specific epidemiological data. Timely and accurate data on diseases are the clues to trends in an epidemic. Displaying and using those data are critical pieces of our work,” senior UNAIDS epidemiologist Mary Mahy said.
Ms Sholts admits that making the data visually engaging was a challenge, but by simplifying the language and adding context, the digital interactive centerpiece works well.
The curator’s aim was to have visitors understand the varying difficulties of getting people to know their HIV status and ultimately the long-term benefits that that entails.
“Diseases are scary stuff, so for every dire challenge or obstacle, we created an “on the upside” component to highlight a success story or uplifting angle,” she said. For the HIV pandemic, the upsides focus on various organizations serving people in need, like the Ponce de Leon Center in Georgia, United States.
She explained that the main goal of Outbreak is to raise public awareness about pandemic risks with the perspective that human, animal and environmental health are all connected as one.
The exhibition also showcases a mock-up of an Ebola treatment ward and a game, played on touch screens, that has visitors simulate a variety of roles—epidemiologist, wildlife biologist or community worker—to complete tasks as a team to end an outbreak.
Part of Outbreak focuses on the detective work involved in tracking down and containing diseases. Future viruses are inevitable, which is why understanding human influence on their emergence and development is key.
Touching wild animals, a lack of vaccination, unprotected sex and travelling when sick all contribute to a virus’ proliferation, linking distant and diverse populations to each other beyond their communities, countries and continents. The response to these diseases, therefore, must also involve everyone.
“We are all connected, we all matter and we have to think holistically, collaboratively and collectively,” Ms Sholts said.
For those not travelling to Washington, DC, the Smithsonian has a free pared-down version of the exhibition—including the UNAIDS interactive display—available for translation and customization worldwide.

Feature Story
Situation rooms bring actionable data to decision-makers
27 August 2018
27 August 2018 27 August 2018Health situation rooms—software platforms designed to support decision-making on countries’ health responses—are opening up across Africa, bridging data and decision-making in order to improve the health and lives of tens of millions of the world’s most vulnerable people.
Data integration, data warehousing and data visualization are the core of the situation room concept, providing transparent and improved information on a range of diseases. While situation rooms are virtual working space, some countries also use physical rooms in which the analytics can be discussed and acted upon.
The idea of a health situation room is that data—whether on the availability of HIV medicines, the effects of a strike by health-care workers or diagnoses of cervical cancer—are centralized, yet accessible to everyone. Whereas in the past health data on different diseases would be spread around several databases in assorted government ministries, disease-specific organizations, etc., situation rooms collect the data in one place, on one system, in a form that is easily shared. The information held by the situation room can be utilized on tablets or computers throughout the country.
“We must continue to innovate in our response to HIV,” said Michel Sidibé, the UNAIDS Executive Director. “Having reliable and up-to-date information is vital if the world is to meet its commitment to end AIDS and reach the Sustainable Development Goals.”
By pooling the health data in the virtual situation room, better and more focused health services can be made available to the people who need them. For example, having data on specific parts of a city helps to drive a location–population approach to HIV prevention services, ensuring that the right people are reached in the right place with the right services.
Through combining data on, for example, HIV, tuberculosis and cervical cancer, interlinkages between the diseases can be seen and responded to. Data can be viewed in real time, so, for example, levels of HIV medicines can be monitored in order to anticipate and respond to medicine stock-outs. Studying the effects of HIV test and treat campaigns in Uganda, the effectiveness of cervical cancer screening in Côte d’Ivoire and malaria testing and new diagnoses in Zambia are other examples how health situation rooms are benefiting health responses.
Five countries—Côte d’Ivoire, Kenya, Lesotho, Zambia and Uganda—have launched situation rooms. Data on indicators, including on HIV, tuberculosis, malaria, noncommunicable diseases and reproductive, maternal, newborn and child health are gathered, with different countries collecting different information depending on the local situation. Namibia, Mozambique and Zimbabwe are preparing to launch situation rooms, and several other countries are in the planning stage.
As part of its work, UNAIDS has been helping countries to set up their situation rooms, with UNAIDS working with countries to select the specific indicators and connecting data in the country to their situation room. Countries with existing data collection systems, that collect data separated by age and sex and at the local level, that have good Internet connectivity and that have qualified local staff are best placed to establish their own situation rooms.
The situation room programme has resulted in UNAIDS’ support to countries being enhanced, with UNAIDS able to support health information systems in a way unique in the United Nations system. UNAIDS is therefore supporting country and programmatic monitoring in a more meaningful way in those countries that have invested in situation rooms.
“For us, its strength is in bringing multiple data sets together, and sharing powerful analytics in a visual and understandable way,” said Andrew Kashoka, Deputy Director of Information Technology, Zambia Ministry of Health.
For the future, UNAIDS plans to ensure that countries have technical support so that they can continue to operate their situation rooms without support from UNAIDS. UNAIDS will also work with partners, including the Africa Centres for Disease Control and Prevention, the private sector and others, to reduce the dependency of countries on UNAIDS’ support in setting up and running the platforms.
Such investments in technology and collaboration between UNAIDS, governments and partners are driving innovative approaches to responding to AIDS and to ultimately ending the AIDS epidemic as a public health threat by 2030.
Resources


Press Statement
UNAIDS welcomes additional evidence from Cameroon, Côte d’Ivoire, and South Africa on progress towards the 2020 targets
22 July 2018 22 July 2018Results from population-based HIV impact surveys provide insight into where investments are needed
AMSTERDAM/GENEVA, 22 July 2018—Cameroon, Côte d’Ivoire, and South Africa have released new survey data on progress towards the 2020 targets. The Cameroon and Côte d’Ivoire population-based HIV impact assessment (PHIA) surveys and the South African survey all studied knowledge of HIV status, new HIV infections, condom use, voluntary medical male circumcision, antiretroviral therapy coverage, viral suppression and other indicators.
In South Africa, which has the largest HIV epidemic in the world with more than 7 million people living with HIV and the largest treatment programme in the world with 4.4 million people on antiretroviral therapy, the new data combined with similar data from an earlier survey indicate that there has been a 40% reduction in the rate of new adult HIV infections between 2010 and 2017.
“These surveys are incredibly important and play a vital role in helping countries to review and refine their HIV programming to make sure that the right services are reaching people affected by HIV,” said Michel Sidibé Executive Director of UNAIDS.
The survey data confirm UNAIDS estimates which indicate that South Africa has also improved treatment coverage and is very close to reaching the 90-90-90* treatment targets. It found that 85% of people living with HIV knew their HIV status, 71% of people who knew their status were accessing antiretroviral treatment and 86% of people who were accessing treatment had supressed viral loads.
Viral load suppression among all people living with HIV in Cameroon and Côte d’Ivoire however was less than 50% reflecting low treatment coverage. The two countries are far from reaching the 90-90-90 targets at 47%, 91% and 80% and 37%, 88% and 76% respectively.
The largest difference between the southern African country and the two western and central African countries is observed in knowledge of HIV status, indicating that HIV testing services need to be significantly scaled up in west and central Africa.
The PHIA surveys provide key information for identifying characteristics of the populations that are not receiving services. In Cameroon, viral load suppression varied by province from 28% to 63%. In South Africa less than 50% of children and young men (ages 15-34 years) living with HIV had suppressed viral load (compared to 67% among the women aged 15-49). These data will provide critical information to allow programme managers to direct their responses to the populations and locations most in need of services.
The PHIA surveys, were led by Columbia University in collaboration with country governments and supported by the United States President’s Emergency Plan for AIDS Relief. The South African survey was conducted by the Human Sciences Research Council
* 90% of people living with HIV know their HIV status, 90% of people who know their status are receiving antiretroviral treatment, and 90% of people on treatment have suppressed viral loads.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Press centre
Download the printable version (PDF)




Feature Story
How HIV treatment numbers are shown to be accurate
26 July 2018
26 July 2018 26 July 2018Estimating how many people living with HIV are on treatment is vital to keeping track of the success or otherwise of the global AIDS response. HIV treatment not only keeps people alive, but, through reducing the viral load of a person, greatly reduces the chance that a person living with HIV will transmit the virus to someone else.
UNAIDS published its latest estimates of the number of people living with HIV accessing antiretroviral therapy in its new report, Miles to go. An estimated 21.7 million [19.1–22.6 million] people of the 36.9 million [31.1–43.9 million] people living with HIV at the end of 2017 were on HIV treatment.
A total of 143 countries submitted the data that UNAIDS used to compile the estimate, representing 91% of all people estimated to be on treatment worldwide. Those 143 countries supply actual counts of people on treatment, not estimates, although estimates are used for those few countries that do not supply counts. Countries report their numbers of people on treatment—both adults and children, disaggregated by sex—through the Global AIDS Monitoring tool every six months. Similar data are included in the Spectrum epidemiological estimation software.
UNAIDS provides technical assistance and training to public health officials and clinical officers—the people who compile the numbers in the countries—to ensure that their reports on treatment coverage are accurate. In addition, every year, in partnership with the United Nations Children’s Fund, the World Health Organization and other partners that support the delivery of HIV treatment services, UNAIDS reviews and validates the treatment numbers reported through both the Global AIDS Monitoring tool and Spectrum.
When UNAIDS’ estimates of treatment coverage in countries are compared with estimates of treatment coverage made in Population-Based HIV Impact Assessments (PHIA) and other surveys, similar levels of treatment coverage are seen (see the attached graph).
In 2017, UNAIDS carried out a triangulation of data as a way to confirm or deny the results of its annual data collection. That analysis sought to answer a simple question: are enough antiretroviral medicines produced and bought to treat the number of people reported to be on antiretroviral therapy?
At the end of 2016, 19.4 million people globally were on antiretroviral therapy, with an estimated 14.1 million people accessing treatment in generic-accessible low- and middle-income countries.
A study of the exports and domestic procurement of antiretroviral medicines in 2016 from India showed 11.4 million person-years of treatment. When the generic antiretroviral medicines produced in other countries were included, an estimate of 14.2 million–16.2 million person-years on treatment was made—sufficient to treat the 14.1 million people in generic-accessible low- and middle-income countries.
In 2018, UNAIDS partnered with the World Health Organization, the Global Fund to Fight AIDS, Tuberculosis and Malaria and selected technical partners and ministries of health in 28 countries, most of which are in sub-Saharan Africa, to conduct data quality reviews of reported treatment numbers and, where over- or undercounting is found, to correct current and historical reports of treatment numbers. Previous data quality reviews since 2016 have been used to adjust estimates, for example by taking into account people who transfer from one clinic to another, but are reported by both clinics, or people who have died, left care or emigrated but are not identified and removed from treatment registries.
More details on the methods for calculating the number of people on treatment can be found in the annex on the methods in Miles to go, while details of how the triangulation was undertaken can be found in a publication published on an earlier triangulation exercise.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025






