Timeline of HIV and TB
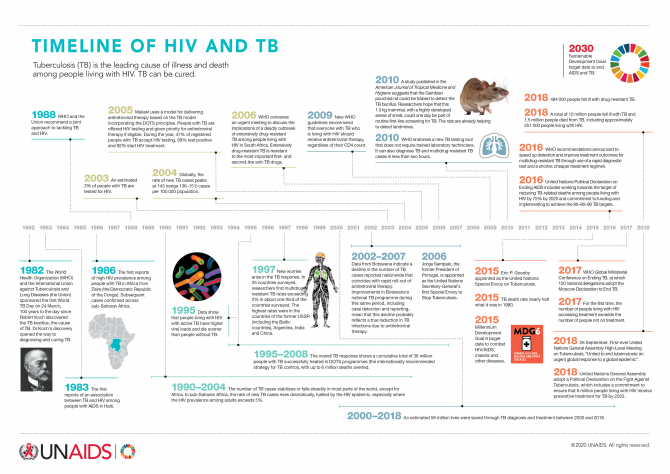
Tuberculosis is the leading cause of illness and death among people living with HIV. TB can be cured.
Tuberculosis TB


16 March 2021
16 March 2021 16 March 2021UCOP+, the Congolese Union of Organizations of People Living with HIV, through funding and technical support from UNAIDS, set up the Observatory project, designed to collect and analyse data to guide action to improve the quality of HIV services.
“The Observatory, which looks at access to and the quality of HIV and HIV/tuberculosis services, is a community-based initiative. Its main objective is to help the government and civil society define and implement national policies in accordance with international norms and standards,” said Natalie Marini, Human Rights and Gender Adviser at the UNAIDS Country Office for the Democratic Republic of the Congo.
The Observatory was set up following repeated stock-outs of HIV and tuberculosis medicine, requests for payment for services that are supposed to be free, the persistence of stigma and discrimination and human rights violations and the long distances that people have to travel to access health care. Three areas are monitored monthly—the availability of services, the quality of care, including the availability of medicine, and accessibility of care.
The initiative shows the importance of collaboration between civil society, health services and donors in the HIV response and has led to an improvement in HIV/tuberculosis services in health facilities. “The Observatory is an indispensable tool that gives us the first clues about supply,” said Aimé Mboyo, director for the National AIDS Control Programme. “It helps us enormously.” The data from the Observatory complements the data of the National Health Information System (SNIS).
Since its launch in 2013, the Observatory has contributed to reducing the cost of access to health care in some health facilities and has anticipated stock-outs and helped to reduce their frequency. The Observatory has also reduced self-stigma by valuing the people who use the services and putting them at the heart of the system. “Before, I didn’t have anything to say about the care offered to me,” said Joséphine Ntumba (not her real name), who is living with HIV. “Now I can give my opinion and make a difference.”
The concept of a “community observatory” has been shown to be a success and is now integrated in the concept note for the Democratic Republic of the Congo of the Global Fund to Fight AIDS, Tuberculosis and Malaria. However, there is still a long way to go—only three out of 23 provincial health departments are covered.

27 February 2025

19 February 2025


15 February 2021
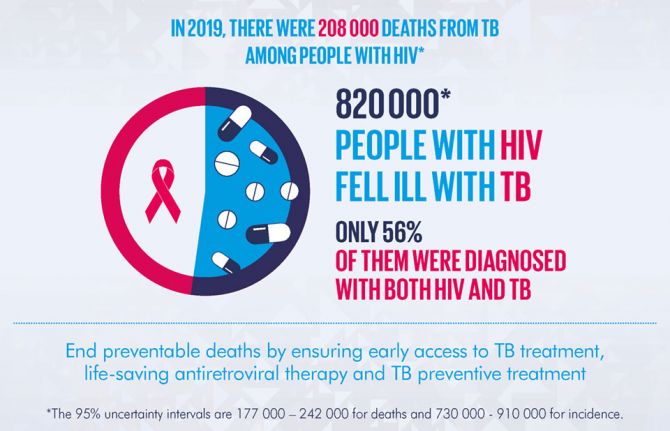
15 February 2021 15 February 2021The risk of developing tuberculosis among the 38 million people living with HIV in 2019 was 18 times higher than in the rest of the world’s population. Tuberculosis remains the single largest cause of premature death among people living with HIV.
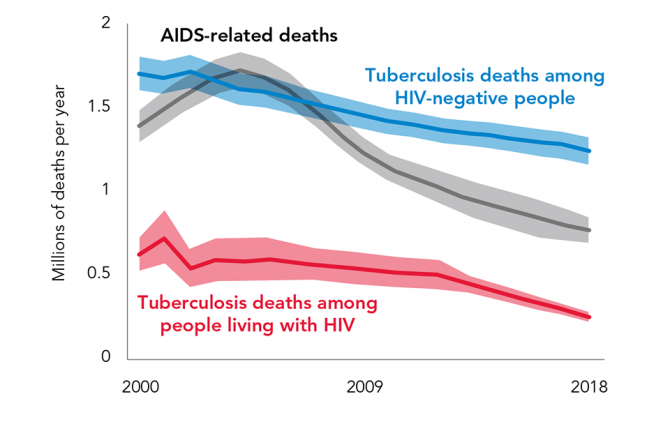
Scale-up of antiretroviral therapy and improvements in the integrated delivery of HIV and tuberculosis services have reduced tuberculosis-related deaths among people living with HIV by 69% globally, from 678 000 in 2000 to 208 000 in 2019. Among the 131 countries that reported data to UNAIDS and the World Health Organization in 2020, 48.9% of the estimated 815 000 people living with HIV who developed tuberculosis (incident cases) received treatment for both HIV and tuberculosis.
The tuberculosis testing gap—the gap between the number of people living with HIV who are estimated to have tuberculosis and the number of people living with tuberculosis who have tested positive for HIV—is narrowing. However, the 456 426 tuberculosis cases among people living with HIV that were notified in 2019 represented just 56% of the estimated number of incident tuberculosis cases among people living with HIV that year. Among people living with HIV who were notified tuberculosis cases, 88% were on antiretroviral therapy in 2019.
Estimated global number of incident HIV-positive TB cases compared with the global number of notified new and relapse tuberculosis cases known to be HIV-positive and the global number of tuberculosis patients started on antiretroviral therapy, 2004-2019



20 October 2020
20 October 2020 20 October 2020The 51st Union World Conference on Lung Health opened today under the theme “Advancing Prevention”. In light of the COVID-19 pandemic, the conference is taking place virtually for the first time in its 100-year history. The event will feature cutting edge science around tuberculosis (TB), air pollution and tobacco control, but also deliver special sessions dedicated to COVID-19 and its intersection with lung health and infectious diseases. Speakers include Her Imperial Highness Crown Princess Akishino of Japan, President Bill Clinton, Shannon Hader, UNAIDS Deputy Executive Director and Divya Sojan—a nurse and TB survivor—among others.
According to the World Health Organization (WHO) Global Tuberculosis Report 2020, there has been an encouraging 63% reduction in tuberculosis deaths among people living with HIV since 2010. This is approaching the 75% global target reduction adopted in the 2016 United Nations Political Declaration on Ending AIDS. However, the report also shows that TB remains the leading cause of death among people living with HIV, resulting in just over 200 000 deaths in 2019—30% of all AIDS-related deaths.
Less than half of the estimated 815 000 people living with HIV who developed tuberculosis disease in 2019 were found, diagnosed and reported to national programmes as receiving treatment for both conditions. The remainder are either missed by programmes, not diagnosed or treated appropriately, or their treatment is incorrectly reported. Once diagnosed however, at least 90% of people with tuberculosis knew their HIV status in over 80 countries and territories and 88% of people living with HIV on TB treatment received lifesaving antiretroviral therapy.
Tuberculosis is curable and preventable. Tuberculosis preventive treatment has been recommended by WHO since 2004 for all people newly diagnosed with HIV. It prevents tuberculosis disease and save lives. Until recently, coverage had been woefully inadequate. However, a combination of advocacy, political commitment, increased availability of shorter, more acceptable treatment options, adequate funding and community engagement has led to an impressive increase in the number of people living with HIV who received TB preventative treatment.
In 2019, WHO reported that 3.5 million people living with HIV started TB preventative treatment – compared with 1.8 million in 2018. The total for 2018 and 2019—5.3 million—already represents 88% of the 6 million target set for 2022 in the 2018 United Nations Political Declaration on Tuberculosis; suggesting that this target could be achieved ahead of schedule.
“It took decades to overcome health worker and community doubts, mobilize specific funding for TB preventative treatment and to invest in research for shorter, more effective and more acceptable treatment regimens,” said Shannon Hader, Deputy Executive Director of UNAIDS, “Now we should raise the target and increase access to and use of the best TB preventative treatment regimens for all in need.”
COVID-19 is already disrupting TB and HIV services, adding to the dual stigma that prevents people from accessing services; lockdown measures that are a further barrier to people being tested or collecting their treatment for TB and HIV and diverting human, financial and laboratory resources away from tuberculosis and HIV.
It has been estimated that globally, a three-month lockdown and a protracted 10-month restoration could lead to an additional 6.3 million people falling ill with TB and an additional 1.4 million TB deaths over the next five years. That would result in a setback of at least five to eight years in the fight against TB – bringing 2021 global TB incidence and deaths to levels not seen since 2013 and 2016 respectively – due to the COVID-19 pandemic.
“Now, more than ever, is the time for the HIV and TB communities to team up and call for investment in shorter treatment and prevention regimens and better infection control, supported by the socioeconomic and human rights protections people need,” said Shannon Hader, UNAIDS Deputy Executive Director. “Overcoming COVID-19, TB, HIV and future pandemics requires global solidarity. Together we must develop and equitably distribute combination prevention, including vaccines, and treatment to all—true universal access that prioritizes those who need it most.”


27 August 2020
27 August 2020 27 August 2020In Yerevan, the capital of Armenia, all polyclinics are now providing free, anonymous, and fast testing for HIV, Syphilis, Hepatitis B and C as part of the “Do not guess, get tested” campaign launched by the Ministry of Health and the Yerevan Municipality on World Hepatitis Day.
“It is an important signal to the population that we keep providing all necessary HIV services to people and that the COVID-19 pandemic has not stopped our prevention and testing work,” said Alexander Bazarchyan, Director of the National Institute of Health.
In preparation for this initiative, the Ministry of Health together with the National Institute of Health and the Municipality of Yerevan, conducted training sessions for medical staff in 20 polyclinics in Yerevan. More than 300 health workers—family doctors, infectious disease specialists, general practitioners, laboratory specialists, etc—received theoretical and practical information on “Management skills of Tuberculosis, Hepatitis B and C” and “HIV testing and counselling services in primary healthcare facilities”.
The activities continued during the COVID-19 epidemic through an educational website developed with support from UNAIDS. The site is a platform where specialists can post accredited online courses so that health professionals can continue their education for free.
In addition, rapid tests for HIV, Syphilis, Hepatitis B and C were purchased within the framework of the UNAIDS Regional Cooperation Programme (RCP) for Technical Assistance on HIV and other Infectious Diseases funded by the Government of the Russian Federation. The RCP aims to strengthen health systems, ensure better epidemiological surveillance of HIV, and promote the scale up of HIV prevention programmes among key populations at higher risk in Armenia, Belarus, Kyrgyzstan, Tajikistan, and Uzbekistan.
“We welcome such timely support as this initiative can facilitate access to testing for people through primary healthcare services and make another step towards achieving Armenia’s commitments to increase access to early diagnosis and treatment,” said Roza Babayan, UNAIDS Representative in Armenia.

20 February 2025





10 July 2020
10 July 2020 10 July 2020The COVID-19 pandemic has spread globally at a speed and magnitude unprecedented in modern times, claiming more than half a million lives and damaging societies and economies. In low- and middle-income countries especially, the COVID-19 pandemic and response is interacting with the global pandemics of tuberculosis (TB) and HIV, creating additional barriers to accessing essential prevention, diagnosis, treatment and care services.
During the opening plenary of the fourth TB/HIV pre-conference of the 2020 International AIDS Conference, the United Nations Deputy Secretary-General, Amina Mohammed, noted that, “COVID-19, like HIV decades before it, and tuberculosis centuries before that, brings into stark reality how inequalities of all types can hollow out our societies, institutions and systems, making us all more vulnerable to health, climate, economic and human security threats. COVID-19 is affecting everyone but not everyone is equally affected.” People must be placed at the centre of the response through rights-based and gender-transformative approaches that also put an end to stigma and discrimination of all types.
TB is the leading infectious cause of death globally and remains the main cause of death among people living with HIV, being responsible for one in three AIDS-related deaths (251 000) in 2018. World Health Organization and UNAIDS estimates suggest that the COVID-19 epidemic and response could cause hundreds of thousands of new HIV infections, a doubling of AIDS-related deaths in sub-Saharan Africa and an additional 6.3 million more TB cases and 1.4 million more TB deaths over the next five years.
The presenters emphasized the need to learn lessons from our experience with the interlinked pandemics of HIV and TB. Rapid transfer of COVID-19 innovations and technology to everyone in need is critical. “Rapid and equitable access to COVID-19 innovations is non-negotiable!” said Winnie Byanyima, UNAIDS Executive Director. “It is imperative that people come before profits, patents and intellectual property. UNAIDS is co-leading the global campaign for a People’s Vaccine to make the COVID-19 vaccine and other technologies patent-free, mass produced, distributed fairly and free at the point of use.”
Over the past decade, billions of dollars have been invested in strengthening health systems infrastructure to deliver TB and HIV services. With the support of civil society and COVID-19 investments this existing infrastructure can be rapidly employed to scale up the COVID-19 response and reach those being left behind while maintaining quality TB and HIV services. TB and HIV civil society organizations are already assisting in finding and testing people with COVID-19 and helping to deliver multimonth supplies of TB and HIV treatment in order to reduce the burden on health-care workers and reduce the risk of transmission of COVID-19.
Few low-income countries would have the capacity to test for COVID-19 without the TB and HIV investments in the multipurpose laboratory testing equipment currently used to diagnose drug-resistant TB and in early infant diagnosis of HIV and monitoring of HIV viral load.
Less than half of all people living with HIV who develop TB disease are diagnosed and treated for both HIV and TB. Increased community testing for COVID-19 provides an opportunity to test for TB and HIV to find the missing millions of cases of TB and HIV in low- and middle-income countries.
While COVID-19 threatens the fragile gains we have made in the HIV and TB response in recent decades, it also offers opportunities to strengthen the response to TB and HIV and systems for health in general.
Ms Byanyima concluded her remarks by saying, “The COVID-19 crisis is a decisive moment for all of us. The right to health has never been higher on the global agenda. This is the time to strengthen the resilience of systems for health and future-proof the health and well-being of generations to come. This is how we will overcome this crisis and finally end AIDS and TB.”
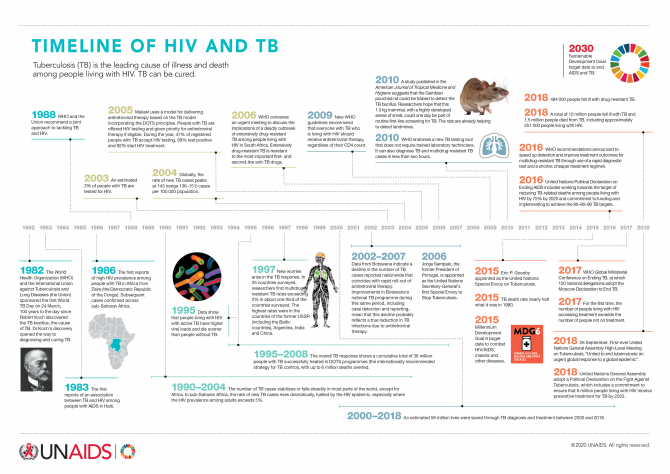
Tuberculosis is the leading cause of illness and death among people living with HIV. TB can be cured.


24 March 2020
24 March 2020 24 March 2020It is no surprise that Birknesh Teferi’s first name means “revolution” in Amharic, the language spoken in Ethiopia. She exudes passion and self-pride; she’s the picture of health and well-being.
Her journey to this point in her life is indeed revolutionary—a story of resilience, hope and transformation. She has beaten tuberculosis (TB), survived cervical cancer and is living positively with HIV.
Ms Teferi was diagnosed with HIV and TB in 2003, a time when information about HIV, TB and sexual and reproductive health in Ethiopia was scarce and stigma and discrimination high.
According to the World Health Organization (WHO), Ethiopia is one of the 48 high-burden TB countries globally. In 2018 in the country, 165 000 people fell ill with TB and there were 27 000 deaths; 2200 of which were among people living with HIV.
After waiting 15 days for her test results, while the health-care worker went on leave, Ms Teferi was told that she was “positive”.
“I thought it was good news. I hugged the nurse in relief, only for her to tell me that being HIV-positive meant I had the virus,” she said.
Ms Teferi successfully underwent the WHO recommended treatment for TB—directly observed treatment short-course (DOTS)—which cured the TB but did not help her with her struggle to accept her HIV status.
“What followed was a period of hurt and heartbreak … Waiting for death,” she recalled of the aftermath of her diagnosis.
She describes herself then as a “drifter.” She did not disclose her HIV status because of stigma and worked as a sex worker to make ends meet.
“If a client had a condom, we would use it. If he didn’t, we didn’t. I tried to use them, but I had no money to buy them. That’s how I developed a sexually transmitted infection.”
During the treatment of the infection, Ms Teferi was diagnosed with cervical cancer and was referred from one health facility to the next, often in different towns.
She eventually found a “caring” doctor and had an operation to treat the cancer. “I was in so much pain, I couldn’t sit. I was miserable,” she remembers.
But when Ms Teferi started to take HIV treatment in 2008, her life slowly changed. She started to look after herself more. She insisted on condom use with her clients.
She met a group of women living with HIV from the Tilla Association of HIV-Positive Women in Hawassa, Ethiopia. The association focuses on capacity-building and training and support of women living with HIV. It runs an embroidery centre as an income-generating activity for women living with HIV, where Ms Teferi now works.
“I am now free of drifting. Life is so much better. If people feel that it is possible to live, possible to work, then life can change,” she said.
For the first eight months of her time at the centre, the manager assigned her a volunteer to help her with her physical recovery from her operation. For the first time, she had support from other women who understood what it was like to be her.
The women at the centre invited her to watch a film about living positively with HIV. “That movie gave me hope,” she says. “I started to learn more about HIV from my manager. I gradually got relief, better medical services and Tilla supported me financially and emotionally.”
While Ms Teferi is on HIV treatment and has been cured of TB, there are millions of people worldwide who still lack access to prevention and treatment for both conditions. TB is the leading cause of death among people living with HIV globally.
In 2018, there were an estimated 1.2 million TB deaths, 251 000 of which were among people living with HIV—this is a 60% reduction from 620 000 in 2000. Between 2000 and 2018, TB treatment alone averted an estimated 48 million deaths among HIV-negative people and TB treatment supported by antiretroviral therapy averted an additional 10 million deaths. However, progress is slow and needs to be accelerated in order to end TB by 2030 as part of the Sustainable Development Goals.
“TB is curable and preventable,” said Aeneas Chuma, the Director for the UNAIDS Regional Support Team for Eastern and Southern Africa, a.i. “It is critical in this moment of history, in the context of the global COVID-19 pandemic, that we ensure that people living with HIV who are diagnosed with TB have uninterrupted access to HIV and TB treatment. UNAIDS is working with governments and community partners to ensure that we adapt to a rapidly changing health context, with kindness, compassion and humanity.”

27 February 2025

24 February 2025


25 March 2020
25 March 2020 25 March 2020There is clear urgency for bringing quality and effective tuberculosis (TB) prevention, treatment and care closer to communities. These efforts should entail empowering communities to use innovative community-based TB services, which have been shown to have a high impact and to be cost-effective.
There has been an unprecedented global mobilization to support countries to end the TB epidemic. These efforts saw the scaling up of TB treatment for an additional 7 million people in 2018 and a reduction in TB-related deaths among people living with HIV by 52% since 2010.
Significant progress has been made towards reaching the United Nations High-Level Meeting on Tuberculosis target of 6 million people living with HIV accessing TB prevention services by 2022—1.8 million people living with HIV started TB preventive treatment (TPT), which reduces their risk of developing active TB disease, in 2018.
However, there are major issues of concern. During 2018, a total of 1.5 million lives were lost to TB, including 251 000 among people living with HIV, which is a third of that year’s 770 000 AIDS-related deaths. Around 10 million people fell ill with TB, 9% of whom were coinfected with HIV. We are still far away from reaching the global target of reducing TB deaths among people living with HIV by 75% by the end of 2020. While the estimated number of new TB cases among people living with HIV in 2018 was 862 000, only 56% of them were aware of their TB status. Less than half of the people living with HIV who newly initiated antiretroviral therapy in 2018 reported also initiating TPT.
More people-centred and community-based approaches that bring services closer to people in need are real game-changers and need be scaled up. For example, as an alternative to the six-month daily TB treatment regimen requiring patients to visit a clinic daily and be monitored by health-care workers that is implemented in some countries—the so-called directly observed therapy (DOT) approach—many programmes are experimenting with digital adherence technologies.
The medication event monitoring box approach involves the patient’s medicines being in a box—a signal is sent to the clinic each time the patient opens the box to access his or her TB medicines. The video DOT method involves patients recording themselves and sending a daily medication update video to their clinic.
These technologies are user-friendly and reduce the time that people are away from their regular activities and reduce the cost of daily transport to the clinic. They provide people with autonomy and empower them to manage their treatment and their health in their home while being monitored for treatment adherence, as well as improving access by vulnerable groups and reducing stigma.
The LF-LAM (lateral flow urine TB mycobacterial lipoarabinomannan) is a simple rapid point of care urine test that the World Health Organization recommends as a game-changer and as a part of a diagnostic algorithm for people living with HIV. It allows the testing of adults and children in health facilities and community-based settings. To date, however, only seven countries among 30 high-burden countries are implementing the LF-LAM tests.
Newer shorter regimens for TPT, such as three months of weekly rifapentine and isoniazid, have been increasingly available owing to recent price reductions and policy shifts. The regimens have fewer side-effects than longer regimens and higher rates of completion. Communities play a key role in supporting people living with HIV to initiate and complete TB preventive treatment, monitor side-effects and seek care for early signs or symptoms of TB.
“Especially in this time of COVID-19, we absolutely need to move on innovative models that allow people to continue their care at home. This means putting in place the quality and supports that people can access virtually, by telephone and in the community. It means delivery models that recognize and respond to the daily constraints on people’s lives and putting the tool directly in their hands to succeed. Let’s empower people to stay connected, continue their care and access additional supports including facilities when they matter most,” said Shannon Hader, the Deputy Executive Director, Programme, of UNAIDS.

23 March 2020
23 March 2020 23 March 2020Tuberculosis (TB) is the 10th leading cause of death worldwide, the worldwide top infectious killer and the leading cause of death among people living with HIV.
The good news is that TB is both preventable and curable, and countries have committed to end TB by 2030. The set of milestones committed to in the 2016 United Nations Political Declaration on Ending AIDS included a 75% reduction from 2010 in TB deaths among people living with HIV by 2020.
The bad news is that, in 2018, 10 million people fell ill with TB worldwide and 1.5 million people lost their lives to the disease, including 251 000 people living with HIV. While there has been a 60% reduction in deaths from TB among people living with HIV since 2000, the world is not on track to reach the 75% reduction by 2020.
As the world is commemorating World TB Day on 24 March in the midst of the COVID-19 pandemic, it is critical to remember that we need to sustain services for addressing TB epidemics and TB/HIV coinfections globally. There is still a US$ 3.3 billion yearly funding shortfall for TB prevention and care.
It is also timely to remember that programmes already in place to combat TB and other major infectious diseases can be leveraged to make the response to COVID-19 more rapid and effective. However, the need for an urgent response to TB, HIV or COVID-19 should not mean that human rights, autonomy and confidentiality are not respected.
The role of communities remains essential, as does the resilience of health system, for ensuring innovative people-centred and community-based and community-led approaches for service delivery, including differentiated service delivery models, digital health and innovative tools to diagnose TB infection and empower people living with HIV-associated TB to manage their treatment and care. Investments in systems for health, including communities, already made will make a real difference in the battle against COVID-19.