Sex workers and clients



Feature Story
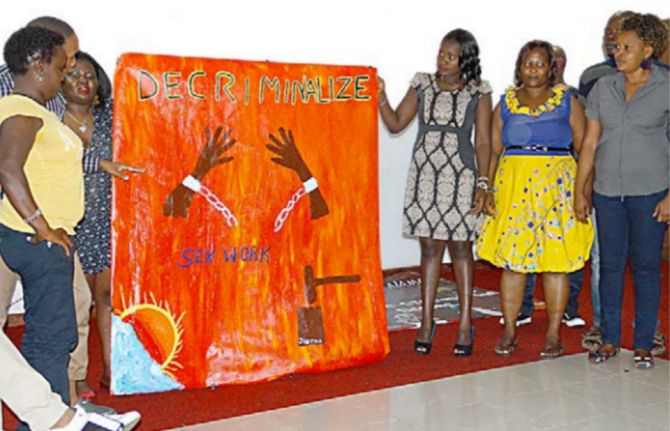
Sex Workers Academy Africa: increasing demand for rights-based HIV prevention services
21 November 2016
21 November 2016 21 November 2016The Sex Worker Academy Africa is a ground-breaking learning programme that aims to strengthen the rights of sex workers across 47 countries in Africa. It focuses on rapidly scaling up sex worker-led responses to HIV, increasing demand for and access to high-quality rights-based HIV prevention and treatment services for female, male and transgender sex workers and increasing HIV testing, leading ultimately to a fall in new HIV infections among sex workers.
The academy’s curriculum is based on the Sex Worker Implementation Tool. Developed by UNAIDS and partners in 2013, the tool outlines recommendations for the prevention and treatment of HIV and other sexually transmitted infections among sex workers in low- and middle-income countries.
Launched in 2015 and since held several times a year, the academy brings together sex workers from across the continent to explore issues such as community empowerment, addressing violence against sex workers, condom and lubricant programming, community-led services and capacity-building. The curriculum includes knowledge-sharing, art and dance advocacy projects, site visits, thematic workshops and feedback sessions. Each academy lasts a week and includes up to 18 participants.
Since its launch, more than 130 sex workers from 17 African countries have graduated from the academy. It has enabled sex workers from Namibia, the United Republic of Tanzania, Zambia and Zimbabwe to form their own national sex worker networks. In addition, sex workers from Lesotho and Swaziland have organized grass-roots organizations for sex workers where previously none had existed.
The academy is an African Sex Workers Alliance initiative implemented by the Kenya Sex Workers Alliance in Nairobi, Kenya. The curriculum was developed in cooperation with the Ashodaya Academy and the VAMP Institute in India, the Asia Pacific Network of Sex Workers and the Global Network of Sex Workers.
Initial funding for the development of the academy was provided by the United Nations Population Fund and the Dutch-funded nongovernmental organization Bridging the Gaps. Bridging the Gaps and the Robert Carr Fund have provided funding for the ongoing implementation of the academy’s work.
HANDS UP FOR #HIVPREVENTION — WORLD AIDS DAY CAMPAIGN


Feature Story
HIV prevention among key populations
22 November 2016
22 November 2016 22 November 2016Since 2010, the annual global number of new HIV infections among adults (15 years and older) has remained static, at an estimated 1.9 million. Members of key populations, including sex workers, people who inject drugs, transgender people, prisoners and gay men and other men who have sex with men, and their sexual partners accounted for 45% of all new HIV infections in 2015.
In some countries and regions, infection rates among key populations are extremely high—HIV prevalence among sex workers varies between 50% and 70% in several countries in southern Africa. One study from Zimbabwe found HIV prevalence rates of 27% for male inmates, 39% for female inmates and 60% for sex workers, with 9.6% of these getting newly infected between 2009-2014. New infections among gay men and other men who have sex with men have been increasing in all regions in recent years. Across countries, key populations are between 10 and 50 times in greater risk of HIV infection compared to other adults.
Criminalization and stigmatization of same-sex relationships, sex work and drug possession and use, and discrimination, including in the health sector, are preventing key populations from accessing HIV prevention services. Effective government support and community-based and implemented HIV prevention and treatment programmes that provide tailored services for each group are currently too few and too small to result in a significant reduction in new infections.
In order to achieve the target of reducing new HIV infections among key populations by 75% by 2020, a large-scale increase of programmes and the creation of an enabling social and legal environment are needed.
We must reduce new HIV infections among key populations
The global number of new HIV infections among adults has remained static, at an estimated 1.9 million, since 2010, threatening further progress towards the end of the AIDS epidemic.
New HIV infections among gay men and other men who have sex with men are rising globally, and there has been no apparent reductions of new infections among sex workers, transgender people, people who use drugs or prisoners. Studies conducted in southern Africa have found HIV prevalence 10–20 times higher among sex workers than among adults in the general population, with rates of HIV infection reaching 50% of all sex workers tested, and HIV prevalence reaching 86% in one study in Zimbabwe. A synthesis of studies including more than 11 000 transgender people worldwide estimates HIV prevalence to be 19.1%.
Key populations remain among the most vulnerable to HIV. Analysis of the data available to UNAIDS suggests that more than 90% of new HIV infections in central Asia, Europe, North America, the Middle East and North Africa in 2014 were among people from key populations and their sexual partners, who accounted for 45% of new HIV infections worldwide in 2015.
Reinvigorating HIV prevention among key populations requires domestic and international investments to provide key populations with tools, such as condoms and lubricants, pre-exposure prophylaxis and sterile needles and syringes, and testing and treatment. However, the design and delivery of such HIV combination prevention services is often limited by a reluctance to invest in the health of key populations and to reach out to them.
In many countries, key populations are pushed to the fringes of society by stigma and the criminalization of same-sex relationships, drug use and sex work. Marginalization, including discrimination in the health sector, limits access to effective HIV services. There is an urgent need to ensure that key populations are fully included in AIDS responses and that services are made available to them.
Guidelines and tools have been developed for and with the participation of key populations in order to strengthen community empowerment and improve the delivery of combination prevention services by community-led civil society organizations, governments and development partners.
The available evidence shows that when services are made available within an environment free of stigma and discrimination and involving key population communities, new HIV infections have declined significantly. For example, street youth in St Petersburg had a 73% decrease in HIV seroprevalence from 2006 to 2012, primarily due to decreased initiation of injection drug use. This marked reduction in the HIV epidemic among street youth occurred after implementation of extensive support programs and socio-economic improvements.
The replication of such successes and the scale-up of combination prevention programmes in all cities and sites where key populations live and work, implemented by countries and community organization networks, will help prevention efforts get back on track to achieving the target of reducing new HIV infections by 75% by 2020.
Quotes
“WHAT MATTERS IS THE LACK OF INCLUSION AND WIDESPREAD DISCRIMINATION. IT IS CLEAR THAT WE CANNOT END THE AIDS EPIDEMIC WITHOUT TAKING CARE OF THE NEEDS OF KEY POPULATIONS.”
Hands up for #HIVprevention — World AIDS Day campaign
Related

Update
HIV prevention among key populations
21 November 2016
21 November 2016 21 November 2016Since 2010, the annual global number of new HIV infections among adults (15 years and older) has remained static, at an estimated 1.9 million. Members of key populations, including sex workers, people who inject drugs, transgender people, prisoners and gay men and other men who have sex with men, and their sexual partners accounted for 45% of all new HIV infections in 2015.
In some countries and regions, infection rates among key populations are extremely high—HIV prevalence among sex workers varies between 50% and 70% in several countries in southern Africa. One study from Zimbabwe found HIV prevalence rates of 27% for male inmates, 39% for female inmates and 60% for sex workers, with 9.6% of these getting newly infected between 2009-2014. New infections among gay men and other men who have sex with men have been increasing in all regions in recent years. Across countries, key populations are between 10 and 50 times in greater risk of HIV infection compared to other adults.
Criminalization and stigmatization of same-sex relationships, sex work and drug possession and use, and discrimination, including in the health sector, are preventing key populations from accessing HIV prevention services. Effective government support and community-based and implemented HIV prevention and treatment programmes that provide tailored services for each group are currently too few and too small to result in a significant reduction in new infections.
In order to achieve the target of reducing new HIV infections among key populations by 75% by 2020, a large-scale increase of programmes and the creation of an enabling social and legal environment are needed.
Hands up for #HIVprevention — World AIDS Day campaign
Related
Documents
Get on the Fast-Track — The life-cycle approach to HIV
21 November 2016
In this report, UNAIDS is announcing that 18.2 million people now have access to HIV treatment. The Fast-Track response is working. Increasing treatment coverage is reducing AIDS-related deaths among adults and children. But the life-cycle approach has to include more than just treatment. Tuberculosis (TB) remains among the commonest causes of illness and death among people living with HIV of all ages, causing about one third of AIDS-related deaths in 2015. These deaths could and should have been prevented. Download slide deck


Update
Implementing comprehensive HIV and STI programmes with transgender people
06 April 2016
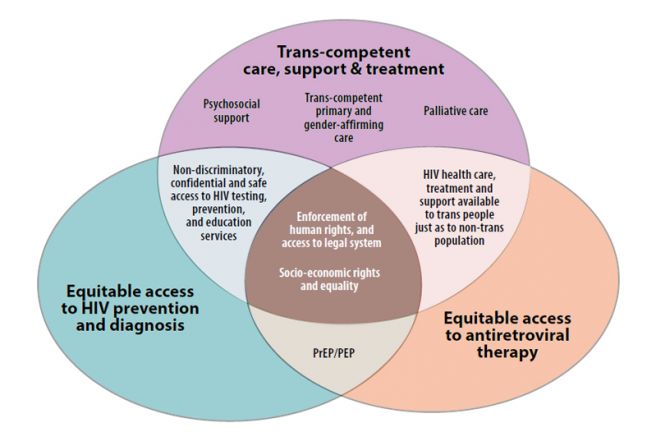
06 April 2016 06 April 2016In collaboration with UNAIDS and other partners, the United Nations Development Programme (UNDP) and IRTG, a Global Network of Trans Women and HIV, have released a new publication today entitled Implementing comprehensive HIV and STI programmes with transgender people: practical guidance for collaborative interventions. The publication presents concrete steps that public health officials, health workers and nongovernmental organizations can adopt to implement HIV and sexually transmitted infection (STI) programmes with transgender people.
Topics covered in the publication include community empowerment and human rights, addressing violence, stigma and discrimination, and delivering transgender-competent services, especially for HIV and STI prevention, diagnosis, treatment and care. The publication also covers community-led outreach, safe spaces and the use of information and communications technology in service delivery. It describes how to manage programmes and build the capacity of organizations led by transgender people and shows how services can be designed and implemented to be acceptable and accessible to transgender women. Wherever possible, it gives particular attention to programmes run by transgender organizations.
The publication was developed in collaboration with transgender people and advocates, service providers, researchers, government officials and representatives of nongovernmental organizations from all over the world. UNDP and IRTG coordinated its production, with the support of the United Nations Population Fund, the University of California, San Francisco, Center of Excellence for Transgender Health, the Johns Hopkins Bloomberg School of Public Health, the World Health Organization, the United States Agency for International Development, the United States President’s Emergency Plan for AIDS Relief and UNAIDS.
The document is based on recommendations included in the Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations, published in 2014 by the World Health Organization.
Transgender women continue to be heavily affected by HIV, being 49 times more likely to become infected with HIV than non-transgender adults.
Quotes
“Discrimination, violence and criminalization deter transgender people from getting the services they need to be healthy and stay healthy. This tool helps planners put into action comprehensive programmes across the whole spectrum.”
“There is an urgent need to ensure that community engagement, policies and programming for transgender people are implemented. This publication, developed with the engagement of transgender activists globally, is an important step forward to making sure this happens.”
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Documents
Implementing comprehensive HIV and STI programmes with transgender people: practical guidance for collaborative interventions
06 April 2016
This tool describes how services can be designed and implemented to be acceptable and accessible to transgender women. To accomplish this, respectful and ongoing engagement with them is essential. This tool gives particular attention to programmes run by transgender people themselves, in contexts where this is possible. It is itself the product of collaboration among transgender people, advocates, service-providers, researchers, government officials and non-governmental organizations (NGOs) from around the world, as well as United Nations agencies, and development partners from the United States.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment
Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment

21 January 2025

Press Statement
UNAIDS welcomes South Africa’s groundbreaking National Sex Worker HIV Plan
11 March 2016 11 March 2016Deputy President Cyril Ramaphosa launches a comprehensive plan to prevent and treat HIV among sex workers
GENEVA, 11 March 2016—UNAIDS welcomes the roll-out of South Africa’s National Sex Worker HIV Plan, 2016–2019. Launched by the Deputy President of South Africa, Cyril Ramaphosa, in his role as the Chairperson of the South African National AIDS Council (SANAC), this unique plan will ensure equitable access to health and legal services for sex workers in South Africa.
Sex workers experience a disproportionate burden of HIV, sexually transmitted infections, tuberculosis, violence, and stigma and discrimination. This progressive plan outlines a comprehensive and nationally coordinated response that is tailored to their specific needs and includes a core package of services for sex workers, their partners, their clients and their families.
As well as delivering access to health services to prevent and treat HIV, sexually transmitted infections and tuberculosis, the plan also aims to provide sex workers with access to justice and legal protection services. These services will be made available through a combination of peer educators, community-driven outreach and referrals, and specialized clinics, as well as through primary health-care clinics, with training for all health workers.
The plan includes making HIV testing available and accessible for sex workers. Sex workers who test HIV-positive will be offered antiretroviral therapy. Sex workers who are HIV-negative will be offered antiretroviral medicines to prevent HIV infection—pre-exposure prophylaxis (PrEP)—in combination with other HIV prevention services.
“South Africa continues to lead and innovate,” said UNAIDS Executive Director Michel Sidibé. “By listening to sex workers and collaborating with the community, South Africa’s tailor-made national HIV plan offers real hope for sex workers, who are often left behind in the AIDS response.”
The results of the Integrated Biological and Behavioural Surveillance survey, launched alongside the report today, demonstrate that HIV prevalence among female sex workers can be as high as 72% in South Africa, but with marked variation in prevalence between different urban settings. Furthermore, the study shows that uptake of antiretroviral therapy by female sex workers already know to be living with HIV is lower than the national average. In 2013, a rapid size estimation study commissioned by SANAC estimated that there were approximately 153 000 sex workers (female, male and transgender) in South Africa; most live and work in the main cities. Studies indicate that HIV prevalence among female sex workers is three to four times higher than among adult women in the general population.
Comprehensive HIV combination prevention, treatment and care services need to reach people who are at higher risk. Ending the AIDS epidemic relies on leaving nobody behind.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Press centre
Download the printable version (PDF)
Region/country


Update
Insights, advances and partnerships to reach key populations in Africa
23 December 2015
23 December 2015 23 December 2015The Second African Conference on Key Populations in the HIV Epidemic, devoted to key insights, key advances and key partnerships, took place in Dar es Salaam, Tanzania, from 16 to 18 December.
The conference brought together more than 200 researchers, policymakers, community actors, health service providers and government representatives from across Africa to discuss experiences, lessons learned and research findings regarding HIV and key populations. They include sex workers, transgender people, gay men and other men who have sex with men, people who inject drugs and others.
Key populations are vulnerable to HIV infection and have been left behind by the AIDS response. Punitive laws, stigma and discrimination are serious barriers throughout the continent for all key populations, with gender inequality contributing to the challenges faced by female sex workers. Migration of key populations within and between countries is another factor linked to their vulnerability to HIV.
Conference participants agreed that peer–led and community-based approaches work best and need scaling up. Effective interventions should be developed with close collaboration of key populations, as well. They also noted that data is important in policy dialogue and in facilitating community engagement.
The conference concluded with a call to action to ensure services for key populations are aligned to their needs and experiences and that key populations meaningfully participate in all areas that pertain to their health and well-being. Participants also called on governments to take down punitive legal barriers, to facilitate access to the justice system and to allocate more resources to serving key populations in the AIDS response.
Quotes
"The next phase of the response should focus on leaving no one behind as a way to end the AIDS epidemic by 2030. This needs addressing a combination of social, political, legal and programmatic gaps for key populations in our countries.”
“We will not reach zero new HIV infections, zero AIDS-related deaths and zero discrimination without the key and vulnerable populations.”
“Grassroot action on HIV is the most important way forward for the global response. Knowledge is only meaningful when shared.”
Region/country

Press Statement
UNAIDS Executive Director opens the Community Village at ICASA and urges countries to leave no one behind in the response to HIV
30 November 2015 30 November 2015Zero discrimination and full engagement of key populations will be crucial to ending the AIDS epidemic by 2030
HARARE/GENEVA, 30 November 2015—On the eve of World AIDS Day 2015, the Executive Director of UNAIDS, Michel Sidibé, stressed the need to reach people most affected by HIV as he spoke at the opening of the Community Village at the 18th International Conference on AIDS and STIs in Africa (ICASA).
Mr Sidibé joined hundreds of civil society members, people living with and affected by HIV and other participants at the official opening of the Community Village, where he also underlined the importance of engaging key populations in global, national and local responses to HIV.
“Key populations are helping us to break the conspiracy of silence,” said Mr Sidibe. “I commend your courage and leadership for building an inclusive and effective response to HIV.”
The Community Village provides a space for grassroots and community-based organizations to present innovative, local responses to the AIDS epidemic and to share information on programmes that are working best among their communities.
“Being here is an opportunity to stand in solidarity with African key populations—sex workers, men who have sex with men, women who have sex with women, trans-diverse persons, people who use drugs, people with disabilities and people living with HIV—in order to end AIDS,” said Regional Coordinator and Executive Director of the African Sex Workers Alliance, Daughtie Ogutu.
The knowledge shared in the Community Village is critical as the most marginalised in society continue to face the greatest challenges in accessing HIV prevention, treatment, care and support services. This is due in large part to persistent stigma and discrimination and other human rights violations, which are drastically increasing the vulnerability of key populations to HIV.
“Coming from a network of women living with HIV, this is a safe space to learn and share with fellow communities,” said Lilian Mworeko, Executive Director, International Community of Women Living with HIV East Africa. “It gives a voice to some of the issues and concerns we have and helps us find solutions.”
Ahead of the conference, UNAIDS joined representatives of key populations including people who inject drugs, gay men and other men who have sex with men, sex workers, transgender people and people with disabilities who came together at a pre-conference meeting to discuss common challenges and approaches to advancing health and protection for their communities. The participants explored innovative programmes and solutions led by key populations to increase access to HIV services, monitor human rights violations, eliminate discrimination in health-care and other settings and create the leadership required for inclusive AIDS responses in Africa.
The 18th ICASA conference comes at a critical time in the response to HIV in Africa, as UNAIDS urges countries to Fast-Track their efforts over the next five years, focusing on the locations and populations most affected by HIV to end the AIDS epidemic by 2030.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Press centre
Download the printable version (PDF)
Documents
AIDS by the numbers 2015
24 November 2015
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment
Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment

21 January 2025