Sex workers and clients
Related
 UNAIDS calls for rights, equality and empowerment for all women and girls on International Women’s Day
UNAIDS calls for rights, equality and empowerment for all women and girls on International Women’s Day

06 March 2025
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025


Feature Story
No end to AIDS without respecting human rights
28 June 2019
28 June 2019 28 June 2019“Sex workers are 13 times more at risk of becoming HIV positive than the general population globally. But, in Australia, where sex work is decriminalised, we have the same rate of infection as the general population. This is evidence of the importance of the legal environment” says Jules Kim, head of the Scarlet Alliance, the Australian Sex Workers Association.
The Human Rights Council first examined the question of HIV and human rights 29 years ago, in 1990. Since then, it has been steadfast in its assertion that progress in the response to the AIDS epidemic is indissociable from progress on human rights issues. Today, as it discusses new recommendations on human rights and HIV, its work is more important than ever.
A total of 48 countries and territories still maintain travel restrictions on people living with HIV. One in five people living with HIV report having been refused health care because of their HIV status, and in many parts of the world, people who use drugs and sex workers live in fear of arrest for being in possession of clean syringes or condoms.
Adolescent girls and young women are among those worst affected because of a lack of respect for their rights. In 2017, 79% of new infections among 10-19 year-old young people in eastern and southern Africa were among females. Inequalities and institutional barriers increase vulernabilities and decrease access to services. Young people in 45 countries are unable to access sexual and reproductive health services or HIV testing services without parental permission.
At a meeting held on the sidelines of the 41st session of the Human Rights Council, co-convened by Brazil, Colombia, Mozambique, Portugal and Thailand, UNAIDS Deputy Executive Director, Shannon Hader, called on countries to dismantle barriers that prevent people accessing essential services. “It has been four years since the world committed to ending the AIDS epidemic by 2030 and three years since the United Nations General Assembly adopted the High-Level Political Declaration on Ending AIDS, which included a commitment to remove human rights barriers by 2020. We have less than two years to deliver on that promise”.
The event marks the presentation of a report and recommendations on HIV and human rights being presented by Michelle Bachelet to the Human Rights Council on July 1. The report, resulting from consultations with civil society, experts, governments and UN mandate holders in February, includes best practise examples, including on the training of health workers on ending stigma and discrimination, on decriminalizing drug use and same-sex sexual activity, model laws on HIV, the training of judges and lawyers, civil society advocacy, and international funding opportunities specifically for human rights programming.
“We cannot address the human rights dimensions of HIV without civil society, who plays a critical role” stated Rui Macieira, Ambassador of Portugal to the United Nations in Geneva.
“The 2030 Agenda for Sustainable Development is an important agenda for people, planet, prosperity, peace and partnership. In order not to leave anyone behind. States should increase their efforts to reach the most marginalized,” said Peggy Hicks, director of the Thematic Engagement, Special Procedures and Right to Development Division of the Office of the High Commissioner for Human Rights.
Member states will examine the recommendations that highlight how reforming criminal laws is critical to advancing progress towards the elimination of HIV, including laws criminalizing gender expression or adult consensual sex, including sex work and same sex relations, as well as drug use. The recommendations include a call for strengthening cooperation at regional, sub-regional and global levels to support and invest in programmes and services that promote the right to health and rights of people living with HIV. This is important in the context of shrinking donor funding for HIV and health programmes, including in newly transitioned middle-income countries.
“I live with HIV, I come from a very small community, a slum area of a Kenyan city. If the recommendations of this report are implemented in a facility that I walk to everyday – a health facility, a police station, then it will work and provide us with the services we need and deserve as a basic human right.” concludes Lucy Wanjiku, a young woman living with HIV.
Related


Feature Story
“Be the change”: creating a voice for male sex workers in Malawi
27 May 2019
27 May 2019 27 May 2019“If I want to see the change, I need to be the change,” said Aniz Mitha, the Executive Director of Community Health Rights Advocacy (CHeRA), an organization that works with male sex workers in Malawi. When Mr Mitha speaks of change, he does so with the quiet and unwavering authority of someone who knows what he is talking about.
From a conservative Muslim family in Malawi, Mr Mitha was thrown out of the house at a young age when his parents found out that he was gay. With nowhere to go and no means to support himself, he fled to Johannesburg, South Africa, where he spent many years as a sex worker. “For me, I was looking to survive; I wasn’t thinking about my health,” he said.
When he became ill, he took an HIV test, and he learned that he was living with HIV. Being an illegal immigrant, he couldn’t access health-care services in South Africa. He returned to Malawi, where he began HIV treatment and started CHeRA. “I thought: how can I help others not go through the same experience that I did?” he said.
CHeRA raises awareness and builds the capacity of male sex workers on HIV prevention and treatment, sexual and reproductive health and rights, economic empowerment, psychosocial support and access to justice. Through a UNAIDS funding arrangement, it recently reached more than 250 male sex workers in three priority districts in Malawi, distributed more than 30 000 condoms and lubricant and linked six male sex workers living with HIV to care and treatment. In another programme funded by the Global Fund to Fight AIDS, Tuberculosis and Malaria, the organization has trained 50 peer educators and distributed more than 6000 condoms and condom-compatible lubricant.
Mr Mitha is keenly aware of the many challenges that face male sex workers, having faced them himself. “In Malawi, sex work is not recognized as work, so there are no laws to protect sex workers. Also, most of our male sex workers are gay men or men who have sex with men, so they live in fear of arrest because homosexuality is illegal in Malawi,” he said.
Stigma and discrimination is institutional, he said. “Male sex workers are not recognized as a key population in the HIV response in Malawi, so we are not prioritized in government plans. And negative attitudes from health-care workers push us away from care.”
“Say I am being abused or beaten and I go to a police station,” continues Mr Mitha, “I will get questions like “Why you are dressed like this or why do you speak like this?” The abuse is institutionalized. It pushes us away, so even in terms of health care, we go to private hospitals where we pay money even if we don’t have money.”
CHeRA is now registered as a nongovernmental organization. Although started in 2016, it was only registered in 2017 after UNAIDS played a pivotal role in amending provisions in the Malawi HIV and AIDS Management Control Act of 2018 that criminalized or discriminated against certain groups, such as sex workers. This paved the way for organizations of lesbian, gay, bisexual, transgender and intersex people and sex workers to be registered.
Like many people who serve others, his work has spilled over into his private life. Knowing what it feels like to be disowned by one’s family, Mr Mitha gives shelter to people who have nowhere else to go, who stay as long as it takes until they can look after themselves.
He has built an unshakeable sense of self, family and community through his work and his life. “I am living openly with HIV and as a gay person; I am a role model to so many. They see that it is possible. I see a lot more people like me opening up and living openly as gay and with HIV,” he said.
Mr Mitha wants to grow CHeRA into an organization that is a strong advocate for equitable access to health care for male sex workers.
“We need more financial support to expand the work we do,” he said. “We provide access to HIV prevention information and services to a population that is being left behind. It is making a difference. When you are working as a community organization, it means what affects my community affects me too,” he said.
Related information
Region/country
Related
Documents
How to reach the most vulnerable?
10 April 2019
If people need to hide then they often miss out on health services. REVS PLUS/Coalition PLUS started offering HIV testing by going to sex worker sites in Burkina Faso. They also built trust among the community to tackle another problem. Music courtesy: mobygratis.
Related
UNAIDS data 2024
02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024

Feature Story
Health and safety: sex workers reaching out to sex workers
26 February 2019
26 February 2019 26 February 2019Leaving the meeting of the REVS PLUS nongovernmental organization, the women bid each other farewell, saying, “A demain soir (See you tomorrow night).” They had gathered at a health drop-in centre that also acts as a network hub for various HIV networks in Bobo-Dioulasso, Burkina Faso, to discuss the following evening’s plan: HIV testing among their peers at selected sites.
“We share our experiences and act as confidantes,” said Camille Traoré (not her real name), a sex worker and peer educator. Her colleague, Julienne Diabré (not her real name), wearing a long flowing dress, chimed in, “In our line of work, it’s hard to confide in someone, so confidentiality is key.”
REVS PLUS/Coalition PLUS advocacy manager, Charles Somé, described the group of women as an essential link in the chain to reach out to sex workers.
“Because of stigma and discrimination, many sex workers hide and move around so they miss out on health services and are much more likely to be infected with HIV,” he said. HIV prevalence among sex workers is 5.4% in Burkina Faso, while it’s 0.8% among all adults in the country.
By recruiting peer educators who know the realities of the job and can relate to other women, Mr Somé said that HIV awareness has increased in the community.
“We also innovated and started HIV testing in the evenings in places where sex workers gather,” he said. Prostitution in Burkina Faso is not illegal, but the penal code forbids soliciting.
The following evening, along a darkened street, REVS PLUS set up foldable tables with two stools at each table. A solar lamp allowed the peer educators to see in the pitch dark and jot down information. Donning plastic gloves, the trained peer educators sat with women, who had their finger pricked and within five minutes were given their HIV test result. No doctors, no nurses were needed. The testing was done by peers because sex workers are afraid to be identified as sex workers.
Mr Somé explained that over the years REVS PLUS outreach has gained the trust of sex workers.
Peer educators, he said, regularly called him to complain about police violence. “It went from arbitrary arrests, to stealing their money, to rape,” Mr Somé said.
Ms Diabré described her dealings with the police. “During the day they point a finger at you and discriminate, while at night they become all nice to get favours and if we don’t deliver then it gets ugly,” she said.
After documenting police abuse for a year with the help of bar owners and feedback from sex workers, REVS PLUS met with government officials and then the police.
“Our approach got their attention and we started awareness training with police officers based on law basics and sex work,” Mr Somé said.
Slowly, REVS PLUS identified allies in each police station, facilitating dialogue whenever an issue occurred. In addition, all sex workers now need to carry a health card showing that they have had regular health check-ups.
A Nigerian woman wearing purple lipstick, Charlotte Francis (not her real name), said, “We still have issues and stay out of their way, but it’s gotten better.” She waved her blue health card, which she says bar owners regularly demand.
Showing off his bar and a series of individual rooms around an outdoor courtyard, Lamine Diallo said that the police no longer raid his establishment. “Before, police would haul away all the women and even my customers,” he said.
UNAIDS, with funds from Luxembourg, is currently partnering with REVS PLUS to scale up the police awareness training across the country. Trainings have taken place in the capital city, Ouagadougou, and in Bobo-Dioulasso.
UNAIDS Burkina Faso Community Mobilization Officer Aboubakar Barbari sees the programme as two-fold. “We supported the awareness sessions for police and security forces because it not only reduces stigma, it also puts a spotlight on basic human rights.”
Special page
Region/country
Documents
Transactional sex and HIV risk: from analysis to action
20 September 2018
This reference document provides a detailed analysis of transactional sex and discusses policy options and principles of engagement around transactional sex in the context of HIV prevention. Although transactional sex is practiced by men and women in all regions of the world, this document focuses specifically on the determinants and consequences of adolescent girls’ and young women’s engagement in transactional sex in sub-Saharan Africa. We focus on this population because of the potential importance of transactional sex for young women’s HIV risk in this region. The document will not address men who have sex with men or gay men and transgender people and the engagement around transactional sex.
Related
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025

Feature Story
Undetectable = untransmittable
20 July 2018
20 July 2018 20 July 2018Undetectable = untransmittable is the message of a new UNAIDS Explainer. With 20 years of evidence demonstrating that HIV treatment is highly effective in reducing the transmission of HIV, the evidence is now clear that people living with HIV with an undetectable viral load cannot transmit HIV sexually.
Three large studies of sexual HIV transmission among thousands of couples, one partner of which was living with HIV and the other was not, were undertaken between 2007 and 2016. In those studies, there was not a single case of sexual transmission of HIV from a virally suppressed person living with HIV to their HIV-negative partner. The Explainer cautions, however, that a person can only know whether he or she is virally suppressed by taking a viral load test.
For many people living with HIV, the news that they can no longer transmit HIV sexually is life-changing. In addition to being able to choose to have sex without a condom, many people living with HIV who are virally suppressed feel liberated from the stigma associated with living with the virus. The awareness that they can no longer transmit HIV sexually can provide people living with HIV with a strong sense of being agents of prevention in their approach to new or existing relationships.
The new UNAIDS Explainer series aims to inform readers about key or emerging issues in the AIDS response. With recommendations for programme managers and advice for national responses, they are short but informative snapshots of the current knowledge about an area of the AIDS response.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025



Press Release
UNAIDS warns that progress is slowing and time is running out to reach the 2020 HIV targets
24 July 2018 24 July 2018New HIV infections are rising in around 50 countries, AIDS-related deaths are not falling fast enough and flat resources are threatening success. Half of all new HIV infections are among key populations and their partners, who are still not getting the services they need
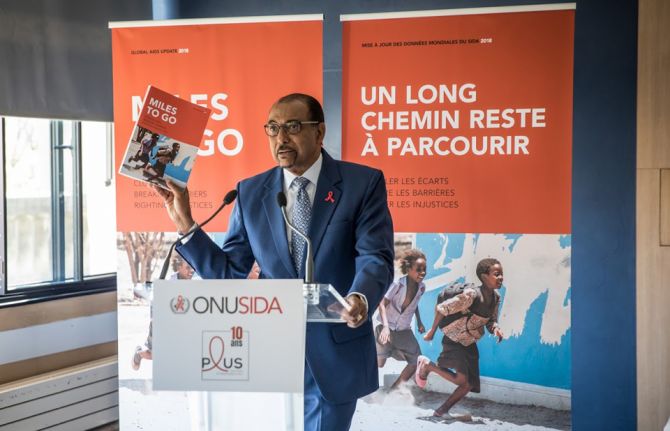
PARIS/GENEVA, 18 July 2018—UNAIDS is issuing countries with a stark wake-up call. In a new report, launched today in Paris, France, at an event co-hosted with Coalition PLUS, UNAIDS warns that the global response to HIV is at a precarious point. At the halfway point to the 2020 targets, the report, Miles to go—closing gaps, breaking barriers, righting injustices, warns that the pace of progress is not matching global ambition. It calls for immediate action to put the world on course to reach critical 2020 targets.
“We are sounding the alarm,” said Michel Sidibé, Executive Director of UNAIDS. “Entire regions are falling behind, the huge gains we made for children are not being sustained, women are still most affected, resources are still not matching political commitments and key populations continue to be ignored. All these elements are halting progress and urgently need to be addressed head-on.”
HIV prevention crisis
Global new HIV infections have declined by just 18% in the past seven years, from 2.2 million in 2010 to 1.8 million in 2017. Although this is nearly half the number of new infections compared to the peak in 1996 (3.4 million), the decline is not quick enough to reach the target of fewer than 500 000 by 2020.
The reduction in new HIV infections has been strongest in the region most affected by HIV, eastern and southern Africa, where new HIV infections have been reduced by 30% since 2010. However, new HIV infections are rising in around 50 countries. In eastern Europe and central Asia the annual number of new HIV infections has doubled, and new HIV infections have increased by more than a quarter in the Middle East and North Africa over the past 20 years.
Treatment scale-up should not be taken for granted
Due to the impact of antiretroviral therapy roll-out, the number of AIDS-related deaths is the lowest this century (940 000), having dropped below 1 million for the first time in 2016. Yet, the current pace of decline is not fast enough to reach the 2020 target of fewer than 500 000 AIDS-related deaths.
In just one year, an additional 2.3 million people were newly accessing treatment. This is the largest annual increase to date, bringing the total number of people on treatment to 21.7 million. Almost 60% of the 36.9 million people living with HIV were on treatment in 2017, an important achievement, but to reach the 30 million target there needs to be an annual increase of 2.8 million people, and there are indications that the rate of scale-up is slowing down.
West and central Africa lagging behind
Just 26% of children and 41% of adults living with HIV had access to treatment in western and central Africa in 2017, compared to 59% of children and 66% of adults in eastern and southern Africa. Since 2010, AIDS-related deaths have fallen by 24% in western and central Africa, compared to a 42% decline in eastern and southern Africa.
Nigeria has more than half (51%) of the HIV burden in the region and there has been little progress in reducing new HIV infections in recent years. New HIV infections declined by only 5% (9000) in seven years (from 179 000 to 170 000) and only one in three people living with HIV is on treatment (33%), although HIV treatment coverage has increased from just 24% two years ago.
Progress for children has slowed
The report shows that the gains made for children are not being sustained. New HIV infections among children have declined by only 8% in the past two years, only half (52%) of all children living with HIV are getting treatment and 110 000 children died of AIDS-related illnesses in 2017. Although 80% of pregnant women living with HIV had access to antiretroviral medicines to prevent transmission of HIV to their child in 2017, an unacceptable 180 000 children acquired HIV during birth or breastfeeding—far away from the target of fewer than 40 000 by the end of 2018.
“One child becoming infected with HIV or one child dying of AIDS is one too many,” said Mr Sidibé. “Ending the AIDS epidemic is not a foregone conclusion and the world needs to heed this wake-up call and kick-start an acceleration plan to reach the targets.”
Key populations account for almost half of all new HIV infections worldwide
The report also shows that key populations are not being considered enough in HIV programming. Key populations and their sexual partners account for 47% of new HIV infections worldwide and 97% of new HIV infections in eastern Europe and central Asia, where one third of new HIV infections are among people who inject drugs.
“The right to health for all is non-negotiable,” said Mr Sidibé. “Sex workers, gay men and other men who have sex with men, prisoners, migrants, refugees and transgender people are more affected by HIV but are still being left out from HIV programmes. More investments are needed in reaching these key populations.”
Half of all sex workers in Eswatini, Lesotho, Malawi, South Africa and Zimbabwe are living with HIV. The risk of acquiring HIV is 13 times higher for female sex workers, 27 times higher among men who have sex with men, 23 times higher among people who inject drugs and 12 times higher for transgender women.
“Communities are echoing UNAIDS’ call,” said Vincent Pelletier, positive leader and Executive Director of Coalition PLUS. “We need universal access to adapted prevention services, and protection from discrimination. We call upon world leaders to match commitments with funding, in both donor and implementing countries.”
Stigma and discrimination persists
Discrimination by health-care workers, law enforcement, teachers, employers, parents, religious leaders and community members is preventing young people, people living with HIV and key populations from accessing HIV prevention, treatment and other sexual and reproductive health services.
Across 19 countries, one in five people living with HIV responding to surveys reported being denied health care and one in five people living with HIV avoided visiting a health facility for fear of stigma or discrimination related to their HIV status. In five of 13 countries with available data, more than 40% of people said they think that children living with HIV should not be able to attend school with children who are HIV-negative.
New agenda needed to stop violence against women
In 2017, around 58% of all new HIV infections among adults more than 15 years old were among women and 6600 young women between the ages of 15 and 24 years became infected with HIV every week. Increased vulnerability to HIV has been linked to violence. More than one in three women worldwide have experienced physical or sexual violence, often at the hands of their intimate partners.
“Inequality, a lack of empowerment and violence against women are human rights violations and are continuing to fuel new HIV infections,” said Mr Sidibé. “We must not let up in our efforts to address and root out harassment, abuse and violence, whether at home, in the community or in the workplace.”
90–90–90 can and must be achieved
There has been progress towards the 90–90–90 targets. Three quarters (75%) of all people living with HIV now know their HIV status; of the people who know their status, 79% were accessing treatment in 2017, and of the people accessing treatment, 81% had supressed viral loads.
Six countries, Botswana, Cambodia, Denmark, Eswatini, Namibia and the Netherlands, have already reached the 90–90–90 targets and seven more countries are on track. The largest gap is in the first 90; in western and central Africa, for example, only 48% of people living with HIV know their status.
A big year for the response to tuberculosis
There have been gains in treating and diagnosing HIV among people with tuberculosis (TB)—around nine out of 10 people with TB who are diagnosed with HIV are on treatment. However, TB is still the biggest killer of people living with HIV and three out of five people starting HIV treatment are not screened, tested or treated for TB. The United Nations High-Level Meeting on Tuberculosis in September 2018 is an opportunity to bolster momentum around reaching the TB/HIV targets.
The cost of inaction
Around US$ 20.6 billion was available for the AIDS response in 2017—a rise of 8% since 2016 and 80% of the 2020 target set by the United Nations General Assembly. However, there were no significant new commitments and as a result the one-year rise in resources is unlikely to continue. Achieving the 2020 targets will only be possible if investments from both donor and domestic sources increase.
Ways forward
From townships in southern Africa to remote villages in the Amazon to mega-cities in Asia, the dozens of innovations contained within the pages of the report show that collaboration between health systems and individual communities can successfully reduce stigma and discrimination and deliver services to the vast majority of the people who need them the most.
These innovative approaches continue to drive the solutions needed to achieve the 2020 targets. When combination HIV prevention—including condoms and voluntary medical male circumcision—is pursued at scale, population-level declines in new HIV infections are achieved. Oral pre-exposure prophylaxis (PrEP) is having an impact, particularly among key populations. Offering HIV testing and counselling to family members and the sexual partners of people diagnosed with HIV has significantly improved testing access.
Eastern and southern Africa has seen significant domestic and international investments coupled with strong political commitment and community engagement and is showing significant progress in achieving the 2020 targets.
“For every challenge there is a solution,” said Mr Sidibé. “It is the responsibility of political leaders, national governments and the international community to make sufficient financial investments and establish the legal and policy environments needed to bring the work of innovators to the global scale. Doing so will create the momentum needed to reach the targets by 2020.”
In 2017, an estimated:
36.9 million [31.1 million–43.9 million] people globally were living with HIV
21.7 million [19.1 million–22.6 million] people were accessing treatment
1.8 million [1.4 million–2.4 million] people became newly infected with HIV
940 000 [670 000–1.3 million] people died from AIDS-related illnesses
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Documents
Miles to go—closing gaps, breaking barriers, righting injustices
13 August 2018
The global AIDS response is at a precarious point—partial success in saving lives and stopping new HIV infections is giving way to complacency. At the halfway point to the 2020 targets, the pace of progress is not matching the global ambition. This report is a wake-up call—action now can still put us back on course to reach the 2020 targets.