PMTCT


Feature Story
COVID-19’s impact on HIV vertical transmission services reversed
27 October 2020
27 October 2020 27 October 2020Recent data collection has shown that the COVID-19 pandemic has had a significant impact on HIV testing services, but the impact on HIV treatment has been less than originally feared. The impact on services for the prevention of vertical transmission of HIV (from mother to child) is mixed—by April, countries generally saw a decline in the number of women tested for HIV at their first antenatal clinic visit, but by June that decline had been reversed.
As of August 2020, the UNAIDS, World Health Organization and United Nations Children's Fund data collection exercise to identify national, regional and global disruptions of routine HIV services caused by COVID-19 had collected data on the prevention of vertical transmission of HIV from 43 countries, of which 17 countries reported data that enable the identification of trends.
To measure the impact of COVID-19 on vertical transmission of HIV services, a ratio was calculated relative to January—for example, if the number of women reached in April was the same as in January, the ratio is 1; if there was a decline, the ratio is less than 1.
All countries except Mozambique and Jamaica experienced declines in women tested for HIV at their first antenatal clinic visit in April compared to January. By June or July, 14 of the 17 countries were back to the February level of testing (all except Indonesia, Botswana and Sierra Leone).
Among the 15 countries reporting on treatment among pregnant women living with HIV, all but five have recovered to the February numbers of women receiving treatment (except Botswana, South Africa, Sierra Leone, Togo and Guatemala).
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025


Press Release
Despite great progress since the early days, the HIV response is still failing children
07 July 2020 07 July 2020GENEVA, 7 July 2020—The latest report on the progress towards the Start Free, Stay Free, AIDS Free targets shows that despite great progress made since the early days of the epidemic, the HIV response for children has fallen behind. Year after year, the bold target of eliminating new HIV infections among children is being missed and children are dying needlessly from AIDS-related illnesses—deaths that could be prevented with simple and cheap treatments if the children were diagnosed and treated in time.
“To see so many tools available, so many new HIV infections among children that have been prevented, so many children living with HIV doing well, but to see others missed and still left behind is a tragedy,” said Winnie Byanyima, Executive Director of UNAIDS. “We cannot accept that tens of thousands of children still become infected with HIV and die from AIDS-related illnesses every year.”
The Start Free, Stay Free, AIDS Free framework has three simple concepts. First, babies have a right to enter the world free from HIV. Second, through HIV prevention, children, adolescents and young women have a right to stay free from the virus. Third, children and adolescents who do acquire HIV have the right to be diagnosed, treated and cared for, so that they can remain AIDS-free.
The world’s countries have agreed to a range of HIV prevention and treatment targets. So that children start out their lives HIV-free, one of those targets was to reduce new child (aged 0–14 years) HIV infections to less than 40 000 by 2018 and 20 000 by 2020. However, newly published estimates show that 150 000 children were newly infected with HIV in 2019—a 52% reduction since 2010, but still four times the 2018 target.
By ensuring that pregnant women living with HIV are diagnosed, started on and retained on antiretroviral medicines during pregnancy, delivery and breastfeeding, the chance that they will pass on the virus is less than 1%. Globally, 85% of pregnant women living with HIV received those medicines in 2019. But despite this high coverage, children are still becoming infected due to unequal access to treatment services (primarily in western and central Africa), women falling out of care and pregnant and breastfeeding women becoming newly infected with HIV.
“As a global community, we have made remarkable progress toward controlling the HIV pandemic, yet we are still missing far too many children, adolescents and young women,” said Angeli Achrekar, Principal Deputy United States Global AIDS Coordinator, United States President’s Emergency Plan for AIDS Relief. “We must all redouble our efforts to urgently reach these critical populations—and PEPFAR remains deeply committed to doing its part.”
The stay-free component set a target of reducing new HIV infections among adolescent girls and young women to less than 100 000 by 2020. Adolescent girls and young women have long been disproportionately affected by HIV—among the Start Free, Stay Free, AIDS Free focus countries, adolescent girls and young women make up 10% of the total population but represent 25% of new HIV infections and are at an almost twofold higher risk of HIV infection compared with their male peers. However, new HIV infections among young women have been falling. In South Africa, where combination prevention programmes for adolescent girls and young women are in place, new HIV infections among this age group have dropped by 35%. And in Eswatini, new HIV infections among young women aged 15–24 years have dropped by 54%.
“For too long, the response to HIV has overlooked children, adolescent girls and young women,” said Henrietta Fore, the Executive Director of the United Nations Children’s Fund. “But there is hope. The recent momentum in reducing new infections among adolescent girls and young women in countries like Eswatini and South Africa show us what is possible when governments and communities, led by girls themselves, join forces. We must not let COVID-19 and its economic headwinds slow us down. We must remain bold and ambitious in our joint efforts to ensure that the next generation of children remain free of HIV and AIDS.”
So that children and adolescents stay AIDS-free, countries called for ambitious but achievable targets for HIV treatment for children—to provide 1.4 million children living with HIV with antiretroviral therapy by 2020. In 2019, however, only 950 000 (53%) of the 1.8 million children living with HIV were receiving HIV treatment—much lower than the 67% of adults on treatment. It is clear that to save lives, the missing 840 000 children not on treatment —an estimated two thirds of whom are estimated to be between 5 and 14 years—must be diagnosed and treated as a matter of urgency.
“The lack of optimal HIV medicines with suitable paediatric formulations has been a longstanding barrier to improving health outcomes for children living with HIV, contributing towards low treatment coverage,” said Tedros Adhanom Ghebreyesus, the Director-General of the World Health Organization. “Access to services for vulnerable groups must be expanded through stronger community engagement, improved service delivery and tackling stigma and discrimination.”
Despite the failures, the positive news is that we do know how the world could have met the Start Free, Stay Free, AIDS Free targets. And with enough commitment, we can still overcome the main obstacles to the targets and reverse the failures.
“The past decade has been marked by innovation and progress in the field of paediatric HIV, but the dramatic miss on targets for children in this latest report is simply unacceptable. We must urgently renew our commitment to fighting for an AIDS-free generation, but today, as a global community, we are failing the most vulnerable among us: children and youth,” said Chip Lyons, President and Chief Executive Officer, Elizabeth Glaser Pediatric AIDS Foundation.
“We can do better. We must do better,” added Ms Byanyima. “We know how to save lives and stop new HIV infections among children. I demand that we spare no effort. Anything less is shameful.”
UNAIDS and the United States President’s Emergency Plan for AIDS Relief launched the Start Free, Stay Free, AIDS Free framework in 2016 to build on the achievements of the Global Plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive, which ended in 2015.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 79 514 68 96
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org
Press centre
Download the printable version (PDF)

Update
How are babies becoming infected with HIV in Africa?
11 February 2020
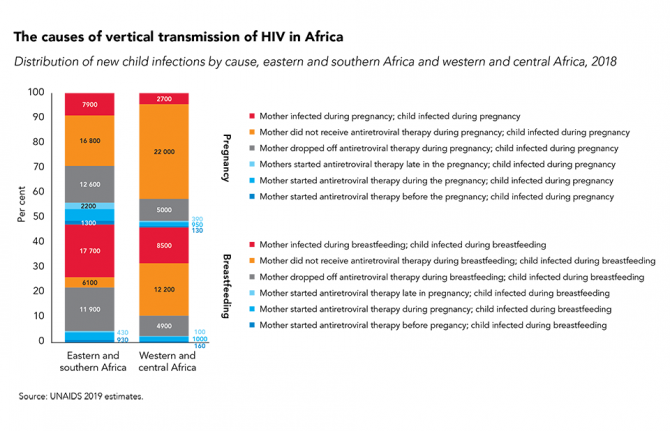
11 February 2020 11 February 2020In Africa, where a pregnant woman living with HIV lives has a big influence on whether her baby will be born HIV-free, and, if not, how her infant will acquire HIV.
There are a many reasons for vertical (mother-to-child) transmission of HIV, including: women not receiving antenatal and prevention of vertical HIV transmission services during pregnancy or breastfeeding; women starting antiretroviral therapy but falling out of care during pregnancy or breastfeeding; and women becoming infected with HIV during breastfeeding or pregnancy. However, not all countries face the same challenges, and to make rapid progress in eliminating vertical transmission it is crucial to know which means of transmission is contributing to the most new HIV infections among children in a country or region.
While the causes of vertical transmission of HIV in different regions vary, one thing is sure: far too many babies are still becoming infected with HIV.
Related






Feature Story
Advocacy toolkit for African first ladies launched
10 February 2020
10 February 2020 10 February 2020An advocacy toolkit to support a campaign by the first ladies of Africa to end childhood HIV and keep mothers healthy has been launched. The toolkit was developed as part of the Free to Shine campaign, an initiative of the Organization of African First Ladies for Development (OAFLAD) and partners to address the growing complacency in the response to childhood HIV in Africa.
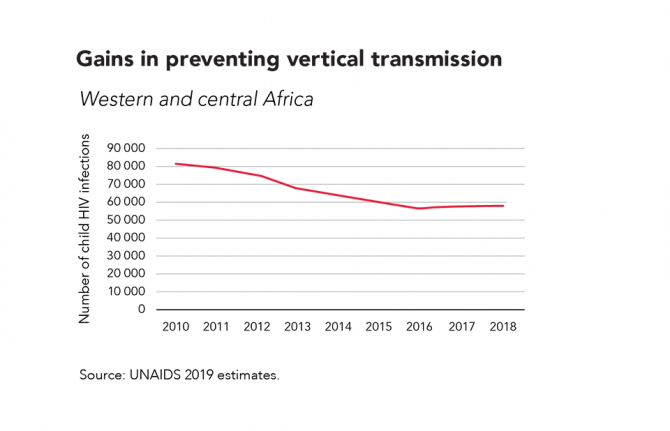
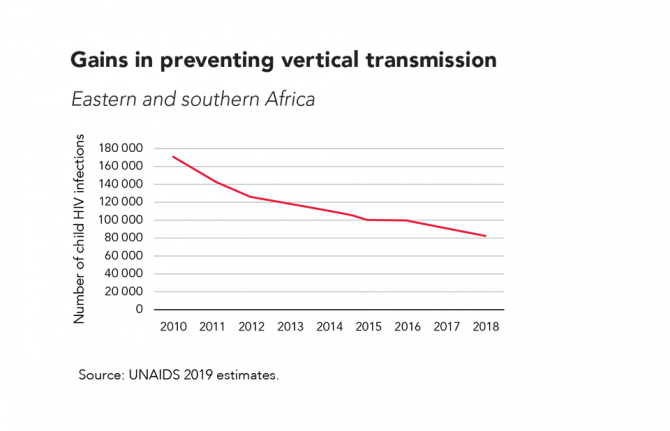
Important gains have been made in the AIDS response for women and children. An estimated 1.5 million new HIV infections among children aged 0–14 years have been averted since 2010 in Africa. The proportion of pregnant women living with HIV on antiretroviral therapy increased from 44% in 2010 to 84% in 2018. However, challenges remain across the continent. AIDS remains the leading cause of death among women of reproductive age. Only half of all children living with HIV have access to antiretroviral therapy, leaving 742 000 children who are neither tested not treated for HIV. Coverage of services to prevent vertical (mother-to-child) transmission of HIV has stalled in eastern and southern Africa and decreased in western and central Africa in the past three years.
The toolkit sets out three areas that the first ladies should focus their advocacy efforts on: keeping women and girls HIV-free; preventing vertical transmission of HIV; and finding missing children and adolescents living with HIV and ensuring that they receive HIV services. Showing how to take the advocacy focus areas forward, the toolkit sets out the background to the three focus areas and gives key messages. A framework for action outlines how the first ladies should use their unique position to raise awareness, convene stakeholders, take action and promote community leadership.
Speaking at the launch, Winnie Byanyima, Executive Director of UNAIDS, said, “We must focus on what is needed next to achieve progress, accelerate our efforts to keep women and girls HIV-free, prevent HIV transmission from a mother to her baby and find the missing children and adolescents living with HIV.”
“We have made critical strides in the fight to end AIDS, but there’s still so much more to be done. We are seeing mother-to-child transmission rates rising in several countries, and we have to prioritize these vulnerable populations. Only with stronger, targeted programmes and campaigns like Free to Shine can we put women and children’s needs at the centre and achieve a generation free of AIDS,” said Chip Lyons, President and Chief Executive Officer of the Elizabeth Glaser Pediatric AIDS Foundation.
OAFLAD, the Elizabeth Glaser Pediatric AIDS Foundation and UNAIDS launched the toolkit on 9 February in Addis Ababa, Ethiopia, during the general assembly meeting of OAFLAD.
Documents
Advocacy toolkit — Africa united against childhood HIV — Free to Shine campaign
10 February 2020
This toolkit proposes three areas for advocacy for first ladies to take the Free to Shine campaign forward, bearing in mind the specific needs of their country:
- ADVOCACY FOCUS 1: Keeping women and girls HIV-free.
- ADVOCACY FOCUS 2: Preventing vertical transmission of HIV.
- ADVOCACY FOCUS 3: Finding missing children and adolescents living with HIV and ensuring that they receive HIV services.
This toolkit shows how to take the advocacy focus areas forward, recalling international and regional commitments relevant to the Free to Shine campaign. This document is also available in Arabic. French and Portuguese.
Related
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
UNAIDS data 2024
02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
Domestic revenues, debt relief and development aid: Transformative pathways for ending AIDS by 2030, Report on Western and Central Africa
18 September 2024
Domestic revenues, debt relief and development aid: Transformative pathways for ending AIDS by 2030, Report on Eastern and Southern Africa
18 September 2024
UNAIDS information/guidance note on the mpox response
30 August 2024
Documents
Power to the people
04 December 2019
A new report by UNAIDS, Power to the people, released ahead of World AIDS Day, shows that where people and communities living with and affected by HIV are engaged in decision-making and HIV service delivery, new infections decline and more people living with HIV gain access to treatment. When people have the power to choose, to know, to thrive, to demand and to work together, lives are saved, injustices are prevented and dignity is restored.
Related
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Zambian football star Racheal Kundananji named UNAIDS Goodwill Ambassador for Education Plus in Zambia
Zambian football star Racheal Kundananji named UNAIDS Goodwill Ambassador for Education Plus in Zambia

23 January 2025




Feature Story
The pros and cons of being small
27 September 2019
27 September 2019 27 September 2019Being small has its advantages. In most Caribbean countries, a local clinic or hospital isn’t very far away. Strong primary health-care systems and high levels of health-care access for pregnant women are at the heart of the region’s success in preventing new HIV infections among children. Seven Caribbean islands have been validated by the World Health Organization as having eliminated mother-to-child transmission of HIV. They range from the British overseas territory of Montserrat, with a population of 5000, to Cuba, home to more than 11 million people.
Antigua and Barbuda received its elimination of mother-to-child transmission of HIV validation in 2017. According to its Chief Medical Officer, Rhonda Sealey-Thomas, the Ministry of Health devised strategies to make certain that all pregnant women feel empowered and supported to start antenatal care as early as possible. The twin-island state employs a community nursing model in which district nurses conduct home visits to encourage women to go to health centres near the start of their pregnancies and to keep their appointments. The country uses its 26 community clinics to ensure that every woman had easy geographical access to antenatal care.
In the Bahamas, the Ministry of Health and the wider AIDS response are working towards validation. It was among five Caribbean countries that achieved 100% coverage for early infant diagnosis in 2018.
Nikkiah Forbes, Director of the National HIV/AIDS and Infectious Disease Programme at the Bahamas Ministry of Health, points to the importance of having a robust health-care system with available and free antenatal care and strong laboratories. Antenatal care is universal in the Bahamas and available at community clinics throughout the island chain. Mothers are encouraged to access care as early as possible and an HIV test is offered during the first visit. Laboratory screening is repeated at 32 weeks. Dedicated nurses ensure that all mothers and infants are retained in care and receive the additional support they need.
“You have to get out in the field if you are going to provide HIV care. We go to clinics to meet the women so we can provide support and counselling. We go into the field and test their partners. We really follow up to ensure they come to the clinic, feel comfortable and are expedited. We ensure they are getting their medication, all their labs are in and that they have nutrition support. If they don’t come to us,” one nurse explained, “we go to them.”
But a small population size also comes with challenges. For migrants, there is often the added vulnerability of standing out when accessing services. Antigua and Barbuda provides health care to all migrants. “Services in the community health clinics are free of cost. Nationality does not matter. If migrants are not afforded health care, it costs more in the long run. By protecting the health of migrants, you are indirectly protecting the health of your own population,” Ms Sealey-Thomas explained.
In the Bahamas, there are also mechanisms for Haitian migrants to access care. “We have translators that speak Haitian Creole at a one-stop-shop clinic. Translations of education materials are also available in Haitian Creole,” said Ms Forbes.
But for citizens who are members of close-knit communities, special care had to be taken to strengthen confidentiality and address stigma and discrimination in health-care settings. Throughout the region, health-care providers have received anti-stigma and discrimination training to address issues that include unconscious bias and confidentiality.
Still, in any Caribbean country the likelihood of people knowing or recognizing others where they access care is relatively high. It’s a challenge that countries must overcome in order to accelerate results across the continuum of care, for adolescents, women and men alike.
Region/country
Related


Press Release
UNAIDS calls on countries to accelerate efforts and close service gaps to end the AIDS epidemic among children and adolescents
22 July 2019 22 July 2019As global 2018 targets are unmet, Start Free, Stay Free, AIDS Free report shows that efforts need to focus on the countries falling behind
GENEVA/MEXICO CITY, 22 July 2019—A new report released today at the 10th IAS Conference on HIV Science in Mexico City, Mexico, shows that the world is lagging behind in its commitment to end the AIDS epidemic among children and adolescents. The report, Start Free, Stay Free, AIDS Free, shows that the pace of progress in reducing new HIV infections among children and expanding access to treatment for children, adolescents and pregnant women living with HIV has slowed significantly and that global targets set for 2018 have been missed, despite important gains being made in some countries.
Globally, around 160 000 children aged 0–14 years became newly infected with HIV in 2018. This is a major decrease from 240 000 new infections in 2010. However, the bold and important target set for 2018 was fewer than 40 000 new infections.
“The failure to reach the 2018 targets to reduce new HIV infections among children and adolescents and to widen access to life-saving treatment is both disappointing and frustrating,” said Gunilla Carlsson, UNAIDS Executive Director, a.i. “We need to act quickly to turn this situation around and honour the commitment to end the AIDS epidemic for the next generation.”
Around 82% of pregnant women living with HIV now have access to antiretroviral medicines. There has been considerable progress among countries in eastern and southern Africa, with more than 90% of pregnant women accessing antiretroviral medicines in Ethiopia, Kenya, Uganda, United Republic of Tanzania and Zimbabwe and 95% or higher in Botswana, Malawi, Mozambique, Namibia and Zambia. This has resulted in a 41% reduction in new HIV infections among children, with remarkable reductions achieved in Botswana (85%), Rwanda (83%), Malawi (76%), Namibia (71%), Zimbabwe (69%) and Uganda (65%) since 2010. The progress made by these countries shows what can be achieved through strong political leadership, rapid policy adoption and concerted efforts by all stakeholders.
The report throws light on where gaps need to be filled to prevent new HIV infections occurring among children. For example, in eastern Africa, 10 000 of 26 000 new HIV infections among children in 2018 were the result of women not being retained on treatment throughout pregnancy and breastfeeding. In southern Africa, 17 000 of 53 000 new infections among children were the result of the mother becoming infected with HIV during pregnancy or breastfeeding. A total of 16 000 new infections could have been averted in southern Africa by retaining mothers on treatment throughout pregnancy and breastfeeding. In western and central Africa, almost 27 000 of the 44 000 new infections could have been averted if their mothers had accessed antiretroviral medicines.
“These new data show that many countries have made important progress toward reaching the 2020 targets, and yet others are lagging significantly behind,” said Deborah Birx, United States Global AIDS Coordinator and Special Representative for Global Health Diplomacy. “These stark disparities highlight the critical role of political commitment, rapid policy implementation and data-driven investments in accelerating impact.”
Country-level analysis of how mother-to-child transmission of HIV happens can provide vital information to shape national responses.
“Ending AIDS and achieving universal health coverage means leaving no one behind. Yet, too many children and adolescents with HIV are still missing out on the chance to grow up in full health as they can’t access treatment,” said Ren Minghui, the World Health Organization’s Assistant Director-General for Universal Health Coverage/Communicable and Noncommunicable Diseases. “We need to intensify our efforts to and keep our promise to these children.”
Children living with HIV are also being left behind in HIV treatment scale-up and are not being diagnosed and treated early enough. An estimated 940 000 children aged 0–14 years were accessing treatment in 2018, double the number that were on treatment in 2010 but far short of the target of 1.6 million set for 2018.
Children living with HIV are still less likely to have access to HIV treatment than adults living with HIV, a disparity that is widening in some countries, especially in western and central Africa. As a result, the AIDS epidemic is still claiming the lives of many children aged 0–14 years. Children in this age group comprised 5% of all people living with HIV in 23 focus countries but accounted for 15% of people who died from AIDS-related illnesses in those countries in 2018.
"We know how to prevent children from contracting HIV, and we know how to prevent the onset of AIDS in children if they do become infected. They need to be tested and linked to care and treatment as a matter of urgency, but we are missing these opportunities,” said Henrietta Fore, Executive Director of the United Nations Children’s Fund. “Knowing what to do is not enough. We must come together and act with renewed commitment to children and adolescents living with HIV and give them the best chance to survive and thrive.”
For optimal outcomes, children who become infected with HIV must access treatment as quickly as possible. However, in 2018, only 63% of the 1.1 million infants exposed to HIV in the 23 countries worst affected by the epidemic were tested for HIV by the age of two months.
“In many ways, we as a community have settled for a substandard quality of care for children living with HIV,” said Chip Lyons, President and Chief Executive Officer, Elizabeth Glaser Pediatric AIDS Foundation, “We must not allow children to perpetually receive less than the basic standard of care we demand for adults. Especially when the ultimate consequence of that approach is that children and young people are dying of HIV at disproportionally and unacceptably high rates.”
The report also shows that the target of reducing the annual number of new HIV infections among young women and adolescent girls aged 15–24 years to less than 100 000 by 2020 is unlikely to be reached. Globally, new HIV infections among young women and adolescent girls were reduced by 25% between 2010 and 2018, to 310 000. While new HIV infections among adolescent girls and young women aged 15–24 years have declined by over 40% in Botswana, Burundi, Lesotho and South Africa, missing the global target has meant that 6000 adolescent girls and young women are still becoming infected with HIV every week.
The root factors driving the vulnerability of young women and girls to HIV infection are social, structural and behavioural and must be addressed in order to achieve sustainable prevention outcomes. Gender discrimination, gender-based violence, restricted access to opportunities and a lack of tailored services all compound their vulnerability to HIV. Effective responses prioritize an approach combining access to HIV and sexual and reproductive health services with social, structural and behavioural programmes.
“The disparity in viral load suppression rates among adolescents with HIV compared to adults is unacceptable and behoves the global community to advocate for more robust, potent antiretroviral therapy regimens for adolescents as well as to hasten efforts to prevent new infections in this critically vulnerable population,” said Fatima Tsiouris, Deputy Director of the Clinical and Training Unit and Prevention of Mother-to-Child Transmission Lead at ICAP, Columbia University.
The number of voluntary medical male circumcisions undertaken between 2015 and 2018 stood at over 11 million among all age groups, which means that at least 13 million procedures need to be carried out by 2020 in order to reach the target of voluntarily circumcising 25 million men and boys between 2015 and 2020.
UNAIDS and the United States President’s Emergency Plan for AIDS Relief launched the Start Free, Stay Free, AIDS Free framework in 2016 to build on the achievements of the Global Plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive, which ended in 2014.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.


Feature Story
Malawi: remember where we have come from to move forward
05 June 2019
05 June 2019 05 June 2019Dan Namarika, the Principal Secretary for Health in Malawi, graduated from the College of Medicine in 1999 as one of the first students to follow their entire medical training in Malawi. His long career as a medical doctor, which included four years as personal physician to the late President Bingu wa Mutharika, was prompted by a desire to act against AIDS.
“The reason I chose medicine was because of AIDS. I couldn’t believe there was an illness like this with no cure. I remember the first case in my neighbourhood. It was a lady who succumbed to AIDS after a chronic illness. I have had family members that have died. My long history has been impacted on by AIDS,” he says.
Since the peak of the HIV epidemic to which Mr Namarike refers, when there were 110 000 new infections (in 1993 and 1994) and 65 000 deaths because of AIDS-related illnesses (in 2004 and 2005), Malawi has made good progress in its HIV response.
This progress can be attributed to the introduction of innovations such as the test and start strategy in 2016, which offers immediate HIV treatment for all people living with HIV and Option B+ in 2011, a prevention of mother-to-child transmission of HIV strategy that ensures that all pregnant women living with HIV have lifelong access to HIV treatment.
As a result, new HIV infections in Malawi have dropped by 40%, from 64 000 in 2010 to 39 000 in 2017, and AIDS-related deaths by half, from 34 000 in 2010 to 17 000 in 2017. Life expectancy continues to rise, from a mere 46 years in 2004 to 64 in 2018, and projections are that it will rise to 74 by 2030.
In 2017, 92% of pregnant women living with HIV in Malawi accessed services to prevent mother-to-child transmission of HIV. This lowered the number of new HIV infections among children (0–14 years) to an all-time low of 4900 in 2017.
Mr Namarika attributes these successes in large part to the multisectoral HIV response and high-level political commitment and leadership. “Besides policies being made at the highest levels of government, we also have ministries other than health involved, such as the treasury, gender, education and local government; we have civil society, the faith-based sector, cultural leaders and technical assistance from development partners, such as UNAIDS,” he says.
He also praises programmatic innovations, such as task shifting from doctors to nurses and community health-care workers, which has helped to reach more people with HIV testing and treatment services.
The 2015–2020 National Strategic Plan for HIV and AIDS has the 90–90–90 targets at its heart, with ending AIDS by 2030 in Malawi as the end goal. Malawi has made good progress in the number of people living with HIV who know their status (90%) and the number of people living with HIV who are on HIV treatment (71%). More work is needed to increase the number of people living with HIV who have suppressed viral loads (61%), which puts Malawi at risk of not meeting the targets in the next 500 days.
The major obstacle to Malawi’s progress in meeting the targets, according to Mr Namarika, is people being left behind because of socioeconomic and structural disparities driven by power relationships, such as poverty, unemployment and gender inequality. He also believes that a location–population approach is needed to address vulnerabilities exacerbated by migration and natural disasters, such as the drought–flood cycle experienced by people located in the south-east of the country.
Another challenge in the national AIDS response is high new HIV infections among adolescent girls and young women between the ages of 15 and 24 years, who accounted for 9500 new infections in 2017—more than double that of their male counterparts (4000).
“Most young people cannot make ends meet. This puts girls most at risk—their rights can be easily trampled on by older men. Also, health-seeking behaviour among young men needs to be improved,” says Mr Namarika.
However, Mr Namarika believes that the biggest obstacle to progress in the AIDS response is complacency.
“When I was a young medical doctor on some days we would have 19 deaths just in the paediatric ward alone. Not in the whole hospital, just in that one ward. Now, the young doctors don’t see that anymore, so they don’t believe that HIV is real,” he says.
He believes that it is critical to continue to engage with communities on AIDS with the same urgency that there was in the early 2000s, so that the significant gains that the country has made are not lost.
“If the cost of AIDS is not regarded as one of the biggest historical disasters we have experienced in the 54 years of our independence, then we have lost our history,” he insists.
The way forward primarily is to continue financing the AIDS response and to put more emphasis on HIV prevention. This will require a growing domestic investment, as well as convincing development partners to put more external sources of funding into HIV prevention, he says.
Related information
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025


Update
HIV infections among children falling
13 May 2019
13 May 2019 13 May 2019The continuing fall in the number of children becoming infected with HIV is a major public health triumph. Globally, 1.6 million new child infections were averted between 2008 and 2017, an achievement that stems from a steep increase in the percentage of pregnant women living with HIV who receive antiretroviral medicines to prevent mother-to-child transmission of HIV or as lifelong therapy, from 25% in 2008 to 80% in 2017.
However, much remains to be done. Efforts to prevent mother-to-child transmission have been slowed by inconsistent treatment adherence among expectant and breastfeeding mothers living with HIV and by the significant numbers of pregnant and breastfeeding women with undiagnosed HIV. A high risk of HIV acquisition faced by women in Africa during pregnancy and breastfeeding has also been underappreciated.