PLHIV




Feature Story
100% Life: 20 years of fighting
04 May 2021
04 May 2021 04 May 2021100% Life, formerly known as the All-Ukrainian Network of People Living with HIV, the largest organization for people living with HIV in eastern Europe and central Asia, is marking its 20th anniversary on 5 May. Those 20 years have seen it work on the most challenging issues of the HIV response in Ukraine, on health-care reform and overcoming stigma and discrimination and barriers to accessing health services.
The organization works to provide 100% access to treatment to 100% of Ukrainian people living with HIV. It strives to improve the quality of life for people living with HIV and promotes the rights and freedoms of people living with HIV, tuberculosis and hepatitis C, including the right to self-determination and the right to make decisions that directly influence their lives.
Beginning with seven members in 2001, today it has grown to 474 members and 15 000 associate members. The first office was opened in Kyiv and now the organization unites 24 regional offices across the country.
In 2004, the organization, together with partners, prevented interruptions of antiretroviral therapy for 137 patients. At the end of 2019, 100% Life was purchasing HIV medicine for 113 000 people.
“Over the years of work, we have purchased 7 230 000 packs of antiretroviral therapy,” said Dmitry Sherembey, head of the 100% Life Coordinating Council. Think about these figures! Behind each of them is a saved life. We are grateful to all our partners who believed in us and continue to believe.”
In 2016, the first 100% Life medical centre was opened in Kyiv. Five years later, three more centres have been opened in Ukraine, in Poltava, Rivne and Chernihiv. These centres are the first clinics created by patients for patients, where services are provided free from stigma and discrimination.
“I have great respect for the struggle that the organization has waged against stigma and discrimination against people living with HIV and other vulnerable people. It is thanks to 100% Life that the first opioid substitution therapy programmes for people who use drugs in Ukraine started, sex workers began to speak openly about their rights and people living with HIV had hope for a normal life, medical care and help from the state,” said Raman Hailevich, the UNAIDS Country Director for Ukraine.
In 2016, the organization received the United States President’s Emergency Plan for AIDS Relief (PEPFAR) award for the best partnership among the 40 countries in which PEPFAR operates.
The same year, there was a breakthrough in state funding of the HIV response, which was increased by 2.3 times. The success of the 20/50/80 transition plan is partly because of the efforts of 100% Life, which worked with the government and advocated for increases in the HIV budget, access to treatment and the optimization of health-care systems.
The struggle of 100% Life won’t stop. New problems come along that need to be addressed.
“We are now facing a new challenge—the COVID-19 pandemic,” added Mr Sherembey. “Our experience gained over the years of interaction with government agencies, partners and donors allows us to contribute to the common cause of the struggle. With the support of the Global Fund to Fight AIDS, Tuberculosis and Malaria and USAID, almost a million pieces of personal protective equipment have been purchased for Ukrainian doctors and social workers, 200 000 tests for COVID-19 have been bought, equipment for oxygen stations at hospitals has been procured, information campaigns on vaccination against COVID-19 have been conducted, and much more is being done.”
Our work
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025


Feature Story
Regional network of people living with HIV launched in the Middle East and North Africa
19 April 2021
19 April 2021 19 April 2021The HIV epidemic in the Middle East and North Africa is still growing—an estimated 20 000 new HIV infections in 2019 marked a 25% increase over the 16 000 new infections in 2010. The region is far from controlling its HIV epidemic and HIV treatment coverage is low, with only 38% of people living with HIV accessing HIV treatment in 2019, resulting in 8000 people dying from AIDS-related illnesses in the region.
Community-based organizations can play important roles in the region’s HIV response, but they are constrained in many countries by limited civic space and resources. In response, community leaders living with HIV have come together to launch the first regional network of people living with HIV, MENA Plus, to strengthen the community HIV response in the region.
“It is time people living with HIV have a network where they make their own decisions and get our rights without stigma and discrimination,” said Amina Ibrahim (not her real name), a member of MENA Plus from Egypt.
With a vision of a society where people living with HIV live with respect and dignity, enjoy their full rights and have equal opportunities, MENA Plus aims to enhance the leadership, representation and effective engagement of people living with HIV across the Middle East and North Africa.
“We need to discuss the suffering of people living with HIV, and especially of children living with HIV, and how to educate them about living their lives,” said Soumayya Abdelwafi (not her real name), a member of MENA Plus from Morocco.
The network will advocate for HIV treatment and prevention services in the region, the sustainability of HIV funding and ending vertical (from mother to child) transmission of HIV and new HIV infections among children.
MENA Plus will put a strong emphasis on human rights, campaigning on sexual and reproductive rights, sensitization on gender diversity and sexual orientation and the rights of minorities and key populations—vital for a region whose HIV epidemic is highly concentrated among key populations and their sexual partners.
“With diversity, we enrich networking and advocacy to help achieve rights,” said Souhaila Abdalla (not her real name), a member of MENA Plus from Tunisia.
Through enhancing the leadership, representation and effective participation of people living with HIV, especially in decision-making around health and social and financial programmes, MENA Plus aims to empower people living with HIV in the region.
“MENA plus is a welcome addition to our UNAIDS team of partners across the Middle East and North Africa. Our friends, family and colleagues living with HIV have shown remarkable resilience, determination and innovation in responding to the interconnected challenges posed by HIV and COVID-19 in recent years. Through MENA Plus, their work has the potential for even greater impact, as the new global AIDS strategy puts community-led responses at the heart of UNAIDS’ work,” said Shereen El Feki, Director of the UNAIDS Regional Support Team for the Middle East and North Africa.
Programme area
Region/country
Related

Feature Story
Tuberculosis deaths among people living with HIV are declining globally, but worrying gaps in TB care persist
24 March 2021
24 March 2021 24 March 2021Globally, the number of people living with HIV who died from tuberculosis (TB), a curable and preventable disease, has fallen from almost 600 000 deaths in 2010 to just over 200 000 in 2019, a fall of 63%. In 2016, a global target was set by the United Nations to reduce TB deaths among people living with HIV by 75% between 2010 and 2020. Nine countries (Djibouti, Eritrea, Ethiopia, India, Malawi, South Africa, Sudan, Thailand and Togo) achieved or exceeded the global target by the end of 2019, one year ahead of schedule.
Further progress towards the global targets has been made in making TB preventive treatment more available to people living with HIV. TB preventive treatment greatly reduces their risk of falling ill and dying from TB. In just two years—2018 and 2019—5.3 million people living with HIV received life-saving TB preventive treatment. That is already 88% of the 6 million target set for 2022 in the 2018 United Nations Political Declaration to End TB.
While progress in some countries is to be applauded, these successes mask the many inequalities and gaps that remain in providing the best integrated care for people living with HIV and TB. These gaps resulted in an estimated 208 000 preventable TB-related AIDS deaths in 2019—about one in three AIDS-related deaths.
“One of the greatest disparities in the global response to HIV and TB is in reaching children,” said Shannon Hader, UNAIDS Deputy Executive Director for Programme. “Much better tools to prevent, diagnose and treat TB and drug-resistant TB for young children are now available, but they are still not enough. Too many children are still not being reached with these new tools. Some health-care workers lack the confidence to manage TB among children living with HIV and, for fear of causing harm and a desire to be protective, they don’t always act. Children are being “protected to death”. We need to build confidence to manage TB and HIV in young children and reach transformational goals.”
TB is especially difficult to diagnose among the youngest infants and children living with HIV—those less than two years of age. The most severe forms of TB—disseminated TB and TB meningitis—are common among this age group and they are life-threatening without prompt diagnosis and treatment. Major advances have been made in improving TB diagnosis for children. Child-friendly medicines for the treatment and prevention of TB are available at low cost from the Stop TB Partnership Global Drug Facility. The challenge is to take these innovations to the scale and quality needed to reach all children living with HIV in need.
The Rome Paediatric HIV & TB Action Plan, part of the UNAIDS and United States President’s Emergency Plan for AIDS Relief Faith Initiative, is closing the gaps for children living with HIV. It is a unique multistakeholder partnership that has stimulated unprecedented collaboration among the faith community, private sector, regulators, donors and others to accelerate the development and implementation of better diagnostic tests, preventive measure and treatments for HIV and TB among children living with HIV.
In 2019, less than half (49%) of the estimated 815 000 people living with HIV who also have TB disease were reported to be receiving both HIV treatment and TB treatment. This demonstrates that large gaps remain in screening, testing and treatment for both HIV and TB. To address this, national programmes need to go beyond traditional health facilities to find the missing millions of people who are still in need of treatment for HIV, TB or both. An integrated, community-based and person-centred approach is needed. Multidisease family and community screening for TB, HIV, COVID-19, high blood pressure, diabetes and other common conditions can be de-stigmatizing and can reduce costs for programmes and people. It is critical to encourage all people recently diagnosed with HIV, TB or COVID-19 to allow confidential screening of their family, household and community contacts, including children and young people.
Already, the clock is ticking for us to reach the ambitious new 2025 targets for TB and HIV laid out in the new global AIDS strategy for 2021–2026. Achieving these targets will place the world back on track to end AIDS and TB by 2030. A collaborative and integrated response to the pandemics of TB, HIV and COVID-19 is needed. The response must be rooted in affected communities and centred on the needs of the most affected people. Addressing the inequalities that drive TB and HIV will help to close the “deadly divide” between global commitments and the lived reality of TB- and HIV-affected communities. By ending inequalities, we can stop adults, young people and children living with HIV from dying of TB.
Our work
Related

Feature Story
Huge gaps in TB care for people living with HIV in some countries
24 March 2021
24 March 2021 24 March 2021All (100%) of people living with HIV newly started on antiretroviral therapy should receive either tuberculosis (TB) preventive treatment (blue bar) or TB treatment (orange bar)—together, they represent “optimal TB care”. The green bar shows the percentage of people newly started on antiretroviral therapy who did not receive optimal TB care and are vulnerable to falling ill or dying from TB.
All people living with HIV who are newly enrolled on antiretroviral therapy should receive “optimal TB care”—either TB preventive treatment or TB treatment. Since 2012, the World Health Organization has recommended that all people newly diagnosed with HIV should be screened for TB. If they do not any have symptoms of TB (cough, coughing up blood, fever, night sweats, weight loss, chest pain, shortness of breath or fatigue) they should receive TB preventive treatment. If they have any TB symptoms, they should be fully investigated for TB disease. If they are found to have TB disease, they should be started on TB treatment immediately. If there is no evidence of TB disease, they should be started on TB preventive treatment.
TB is the commonest cause of hospitalization and death among people living with HIV. In 2019, TB was responsible for 208 000 (30%) AIDS-related deaths. Yet, TB is curable and preventable. TB preventive treatment reduces the risk of developing TB disease and can reduce deaths among people living with HIV by almost 40%. Without treatment, a person living with HIV who has TB disease is likely to die.
Our work
Related


Feature Story
Positive Women with Disabilities in Uganda puts people at the centre during COVID-19 pandemic
29 March 2021
29 March 2021 29 March 2021The World Health Organization estimates that, globally, more than 1 billion people (15% of the world’s population) have a disability. Disability is increasing in prevalence due to ageing populations, trauma, accidents and chronic health conditions, including HIV, tuberculosis (TB) and COVID-19.
Persistent discrimination against and exclusion of people with disabilities, in particular women and girls with disabilities, increases their vulnerability, including their risk of HIV infection. People with disabilities, in particular women and girls with disabilities, also experience barriers to accessing HIV services and are left behind in HIV policy-planning, programme development, service delivery and data collection.
People with disabilities face stigma and discrimination in families and communities, lack transport to health-care facilities and are faced with poor attitudes of health workers while seeking health care.
Since 2004, the AIDS Service Organization (TASO), based in the Mulago Hospital Complex in Kampala, Uganda, has attempted to reach out to people with disabilities. However, it has had limited success due to the complexities of community-based care.
In 2016, in response to these challenges, Positive Women with Disabilities (POWODU) was formed out of TASO to pay special attention to people with disabilities living with HIV in order to reduce AIDS- and TB-related deaths, stigma and discrimination and to promote sexual and reproductive health and rights.
POWODU is headed by Betty Kwagala, a formidable advocate, trainer and woman living with HIV who has 25 years’ experience serving as a counsellor at TASO Mulago. Ms Kwagala is a respected and well-known figure in the community, who has uplifted the lives of many people living with HIV in Uganda.
POWODU, in partnership with TASO Mulago, reaches out to people with disabilities in the urban districts of Kampala, Wakiso and Mukono. According to TASO’s client register, there are more than 13 000 people with disabilities in Kampala and Wakiso enrolled into HIV care. Seventy per cent are women and the majority are homeless.
HIV testing and TB screening are integrated into every POWODU community outreach. “The services are always offered near to where people with disabilities reside because of mobility and transport challenges,” says Ms Kwagala.
If a client tests positive for HIV, POWODU offers immediate initiation of HIV treatment, as per the Ministry of Health guidelines. If a sputum TB test is positive, POWODU will refer the case to the main laboratory for further investigation and proper management. POWODU will then follow up, and, with the support of a TB focal person, arrange pick up for the client in a TASO van to escort him or her to receive the appropriate health service.
Other services offered on site by POWODU include sensitization on adherence to both HIV and TB treatment, prevention of HIV, TB and COVID-19 and accurate information on sexual and reproductive health and rights among people with disabilities.
“The COVID-19 pandemic has led to clients who have been lost to follow-up because they are homeless or reside in informal settlements. The lockdown caused more challenges, such as lack of food and a significant disruption to the usual activities that give them some income, such as begging,” says Ms Kwagala.
During the COVID-19 lockdown, UNAIDS supported 200 people with disabilities living with HIV with food rations, personal protective equipment and personal hygiene kits. It also supported a project to equip 40 people with disabilities with skills on how to identify income-generating activities. They were provided with popcorn-making machines and groundnut grinders.
TASO members were provided with megaphones and sensitized members of their communities on HIV, TB, COVID-19, sexual and reproductive health and gender-based violence.
“POWUDU and TASO have shown remarkable resilience by putting people at the centre during the COVID-19 pandemic by ensuring that people with disabilities living with HIV are safe and not left behind,” says Jotham Mubangizi, UNAIDS Country Director, a.i., for Uganda.
Our work
Region/country


Press Statement
UNAIDS warns that violence in Myanmar is impeding access to services for people living with and affected by HIV
17 March 2021 17 March 2021GENEVA, 17 March 2021—As the situation in Myanmar continues to deteriorate and fatalities rise, UNAIDS is warning that the violence also threatens access to life-saving essential services, including services for people living with and affected by HIV.
Ensuring the safety and protection of health-care workers and outreach and community volunteers across the country is critical, as is ensuring continuity in the procurement and delivery of essential life-saving services. Of priority concern across the country is maintaining access to HIV services, including the supply and delivery of antiretroviral medicines and harm reduction services for people who inject drugs.
“I express solidarity with the people of Myanmar and recognize the exceptional leadership of young people, women and social activists in trying to uphold human rights,” said UNAIDS Executive Director, Winnie Byanyima. “I also salute community networks of people living with and affected by HIV, civil society and activists who have mobilized to support and protect the most vulnerable people.”
UNAIDS further adds its voice to the urgent calls made by the United Nations Secretary-General, António Guterres, for all violence against civilians in Myanmar to cease.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Region/country

Feature Story
Stranded in Nepal without HIV medicine
15 March 2021
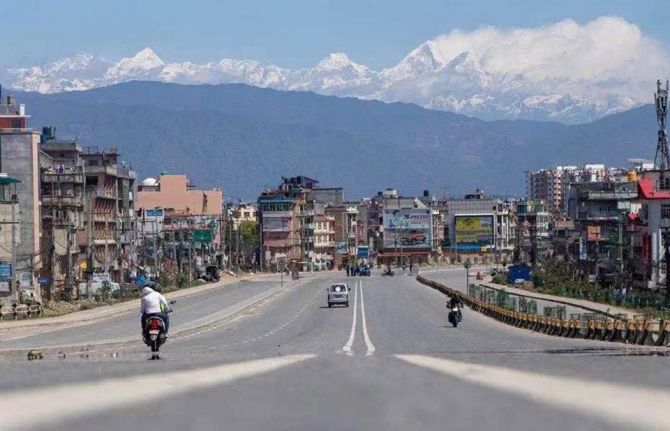
15 March 2021 15 March 2021Wang Tang (not his real name) had never been to Nepal before, but at the end of March 2020 it was one of the few countries that had not closed its borders with China. Since he was desperate to get away from Beijing after having had to stay at home for months after the coronavirus outbreak spread throughout China, he bought a ticket.
But days after he arrived, while he was staying in Pokhara, the fourth stop on his trip, the local government announced that the city would be shut down. He heard that the lockdown would not last longer than a month.
As someone who is living with HIV, he had brought along enough HIV treatment to last for a month. However, he soon learned that the re-opening of the city was to be postponed, which meant that he was at risk of running out of the medicine he needed to take regularly in order to suppress his HIV viral load and stay healthy.
Mr Wang swallowed hard while counting the remaining tablets. He had no idea how to get more.
As the lockdown dragged on, it seemed that no end was in sight. Mr Wang started to take his medicine every other day so that his supply would last a little bit longer.
He contacted his friends back at home, hoping that they could send medicine to Nepal, but they couldn’t. The country was under lockdown—nothing could be imported.
Then, Mr Wang contacted his friend Mu-Mu, the head of Beijing Red Pomegranate, a nongovernmental organization providing volunteer services for people living with HIV. It was with Mu-Mu’s help that Mr Wang learned how to obtain HIV treatment after he was diagnosed as living with HIV. Having known each other for many years, Mu-Mu had the trust of his friend. Mu-Mu contacted the UNAIDS Country Office for China to see if it was possible to deliver medicines to Mr Wang. A UNAIDS staff member quickly got in touch with the UNAIDS Country Office for Nepal.
Everything happened so quickly that Mr Wang was shocked when he received a message from Priti Acharya, who works for AHF Nepal and had been contacted by the UNAIDS Nepal office, saying that she would bring the medicine to him.
The next day, Ms Acharya rode her motorbike for 15 km on a dusty road before reaching the place where she would meet Mr Wang. When he came down from the mountains to meet her, Ms Acharya, drenched in sweat, was waiting under the midday sun.
“I was so happy and thankful for her hard work. She gave me a sunny Nepalese smile in return, as well as detailed instructions on the medicine’s dosage,” said Mr Wang.
They took a photograph together, then Mr Wang watched Ms Acharya as she left on her motorbike. Her image, disappearing in the distance, is carved into his memory. To attend the five-minute meeting, Ms Acharya had to ride a round trip of more than 30 km.
“For half a month or so, I had been suffering from pain and anxiety almost every day due to the lack of medication and the loneliness of being in a foreign country on my own. I could not believe that I got the HIV medicine in such a short time,” said Mr Wang. After the trip, he wrote to thank Ms Acharya, explaining how important the medicine he now had in his hand was: “it’s life-saving.”
At the end of his stay in Nepal, Mr Wang wanted to do something for UNAIDS. As he is an experienced photographer, he volunteered to carry out a photo shoot for UNAIDS’ Nepal office.
The subject he chose was former soccer player Gopal Shrestha, the face of an HIV charity in Nepal and the first person living with HIV to reach the summit of Mount Everest. After his HIV diagnosis in 1994, Mr Shrestha launched the Step-Up Campaign and spent many years climbing mountains worldwide, hoping to give strength and hope to people living with HIV.
In 2019, Mr Shrestha reached the peak of the world’s highest mountain, Mount Everest, recording a historic breakthrough for people living with HIV. “If 28 000 people have already climbed Mount Everest, why can’t I?" he said. “By climbing the highest mountain in the world, I want to prove that we are no different from anyone else and that we can all make a difference.”
“The moment I saw him, I could tell he was a sophisticated man,” said Mr Wang. Without instructions, Mr Shrestha posed naturally in front of the camera. He displayed confidence and charm. His eyes, content and clear, reflected nature’s beauty. “The eyes surely are the window to the soul,” Mr Wang said.
Mr Wang is looking forward to his next trip to Nepal. After the pandemic, Pokhara’s lakeside will be flooded with tourists, and he looks forward to seeing the mountain town bustling with people like it used to.
Our work
Region/country
Related


Feature Story
From HIV survivor to COVID-19 responder
03 March 2021
03 March 2021 03 March 2021Ingrid Bretón learned that she was living with HIV when she was 19 years old. It was 1994 and HIV treatment was not yet available in the Dominican Republic.
“I lasted almost five years alive, but dead inside,” she remembers. “I went through every denial process that a newly diagnosed person goes through. Health centres did not want to assist me. I lived every kind of stigma and discrimination.”
In her town, La Romana, she was known as “the AIDS girl”. It was impossible to find work.
HIV treatment helped changed the trajectory of her life. With the guidance of her doctor, José Román, she became the first woman living with HIV in La Romana known to have given birth to an HIV-free baby. As she continued treatment it occurred to her that she was perfectly healthy and could live a more meaningful life.
“I thought to myself, “I am not getting sick, my hair is not falling off, I do not have sores, I do not have AIDS. I want to do things,”” Ms Bretón remembers.
In 2002 she formed the Paloma Group Foundation (La Fundación Grupo Paloma), which provides psychosocial support, legal assistance and job opportunities for people living with and affected by HIV in the eastern region of the country. The organization also plays a key advocacy role, bringing visibility to issues such as treatment adherence, prevention and stigma and discrimination.
One of the foundation’s innovations is an agriculture project that employs people living with HIV.
“It’s a beautiful process,” Ms Bretón says while walking through the sunny, red earth fields, past tomatoes, papayas and bananas. “The idea is that people living with HIV are able to move forward, working and providing for their families.”
The families with whom the Paloma Group Foundation works have been directly affected by the COVID-19 pandemic. The work of the foundation has been critical during this time. Its volunteers do home deliveries of food, medicine and clothing. The foundation is a source of connection and emotional support at a time when communities living with HIV are more isolated than ever due to social distancing measures.
The first Rapid Survey on the Needs of People Living with HIV in the Dominican Republic in the context of COVID-19 found that while 92% of respondents received their antiretroviral therapy, roughly one in six had less than one month’s supply left. Thanks to the advocacy of the UNAIDS Country Office for the Dominican Republic, protocols have now been amended so that people living with HIV and accessing treatment through the public health system can receive a three- to six-month supply of their medicine at one time.
The country office has urged the government to strengthen comprehensive care programmes, including through alliances with civil society. For example, the Paloma Group Foundation provided assistance to people living with HIV at the Francisco Gonzalvo Provincial Hospital during a five-month period in 2020 when medical personnel were not available at the La Romana facility.
The UNAIDS Country Office for the Dominican Republic has also called for particular attention to be given to the social protection and food security needs of people living with HIV who are in economically fragile situations. The office responded quickly to the fallout of COVID-19, offering support to the Paloma Group Foundation and other community organizations contributing to the national HIV response. UNAIDS’ comprehensive response included the provision of personal protective equipment and information specifically for the community of people living with HIV. The second stage of their response included mobilization of nutrition support.
“This was of great value to families given the economic crisis caused by COVID-19,” Ms Bretón says.
“Civil society plays the leading role of bringing awareness to communities and advocating on their behalf,” says the UNAIDS Country Director for the Dominican Republic, Bethania Betances. “As we respond to two pandemics—HIV and COVID-19—is it vital that they are at the decision-making table to help shape an effective, humane response.”
Watch: The extraordinary story of a woman living with HIV in the Dominican Republic
Region/country
Related


Feature Story
COVID-19 spurs on multimonth dispensing of HIV treatment in Cambodia
25 February 2021
25 February 2021 25 February 2021When the COVID-19 pandemic broke out in Phnom Penh, Em Ra, pictured above, was worried.
She lives with HIV and she only had supplies of medicine to last a month.
“First, I was afraid that the medicine could not be shipped to Cambodia, the second is that when we don’t have medicine for a few months we have to come to the clinic often,” she said. “This increases my expenses but also raises my chances of getting COVID-19.”
During a recent visit to the National Center for HIV/AIDS, Dermatology and STDs (NCHADS) clinic, her doctor, Prak Narom, informed her that she would qualify for multimonth dispensing of HIV treatment. “Because of COVID-19, a patient in good health who takes their treatment daily can be prescribed HIV medicine for more than three months, and for some patients we can give them up to six months,” he explained.
Ms Ra is one of thousands in Cambodia who can now pick up a stock of medicine in one visit. There are an estimated 73 000 people living with HIV in Cambodia and now nearly 50% of people on treatment have access to multimonth dispensing of HIV treatment. Before the pandemic, that number stood at 34%.
The multimonth dispensing of HIV treatment programme in Cambodia began in 2019, long before the COVID-19 pandemic, but it has proven to be a godsend.
“When we started multimonth dispensing, there were some challenges because we had a shortage of drugs, but today we have overcome that so we can give medicine to people for up to six months,” said Ly Penh Sun, Director of NCHADS, pictured above.
The UNAIDS Country Director for Cambodia, Vladanka Andreeva, had feared the worse when COVID-19 shut down the country. “The biggest and oldest HIV treatment site in the capital was repurposed to serve as a COVID-19 centre and our outreach activities had to cease with public venues closed to the public.”
But UNAIDS, with the national AIDS programme and communities, worked together and helped with moving people to another treatment site, while providing face coverings and hand sanitizer to people living with HIV. UNAIDS also advocated that people living with HIV be integrated in the emergency cash transfer programme. As a result, more than 2500 households benefitted.
And more importantly, UNAIDS and partners pushed to introduce the home delivery of treatment and the rollout of multimonth dispensing of HIV medicine at the national level.
“We have used COVID-19 as an accelerator to further scale up and promote the multimonth dispensing of medicine,” Ms Andreeva said, pictured above.
It has been so successful that Mr Narom can’t believe it.
“In the past we used to see 30 patients in the morning, but now with multimonth dispensing we can reduce that by half or more than half,” he said. “I can now spend more time with my patients and carry out more in-depth check-ups.”
When a person is unable to take antiretroviral therapy regularly, their viral load increases, impacting the person’s health, which can ultimately lead to death. Even relatively short-term interruptions to HIV treatment can have a significant negative impact on a person’s health and potential to transmit HIV.
UNAIDS is advocating that all countries, ministries of health and national AIDS programmes grant access to three months or more of antiretroviral therapy for all people living with HIV, including refugees and migrants.
As for Ms Ra, she has joined a Telegram group started by the clinic for people living with HIV in case they have questions about their health or their medicine.
Watch: COVID-19 spurs on multimonth dispensing of HIV treatment in Cambodia
Photo credit: UNAIDS/S.Dara
Our work
Watch: COVID-19 spurs on multimonth dispensing of HIV treatment in Cambodia
Region/country
Related


Feature Story
“We must move forward, only forward”
25 February 2021
25 February 2021 25 February 2021Malohat Sharipova, pictured above, teaches in a primary school in Bohtar, Tajikistan, but in her spare time she works as an outreach worker for AFIF, a nongovernmental organization that helps people living with HIV, tuberculosis and key populations.
AFIF works closely with the regional AIDS clinics, providing outreach workers who support and work with people living with and affected by HIV. During the COVID-19 pandemic, AFIF’s outreach workers have provided people living with HIV with three-month supplies of antiretroviral medicines, food and personal protective equipment, including antiseptic, masks and gloves.
The outreach workers are trained to carry out screening to detect tuberculosis and hepatitis in people living with HIV and injecting drug users. “It is necessary to ask 10 to 12 questions on HIV and tuberculosis developed by specialists to determine the need for further diagnosis. If there are symptoms, a person is advised to undergo timely testing, either at the nearest medical centre or using a kit for self-testing, which we provide,” said Ikram Ibragimov, the Director of AFIF.
AFIF’s activities are supported by the Ministry of Health of Tajikistan and conducted within the UNAIDS Regional Cooperation Programme for Technical Assistance for HIV and Other Infectious Diseases in the Commonwealth of Independent States, funded by the Russian Federation. Since the beginning of the project in 2019, about 7500 people have undergone community-based testing.
Ms Sharipova has four children, two daughters who are married and have left home, an older son who works in another city and her youngest son, who is in the 11th grade in school.
“In 2010, my husband was admitted to hospital. Before that, he had been complaining of abdominal pain for a long time. I tried to persuade him to visit a doctor, but he didn’t. He was hospitalized when it got bad, was diagnosed with liver cirrhosis and died soon after. I got a call from the hospital, and they told me to get tested for HIV.”
“When they told me that I had HIV, I thought, “Thank God I'm still alive, I can walk and work.” After my husband’s death I needed to raise my children, support my mother-in-law, who I loved like a mother.”
She has been taking antiretroviral therapy since 2010. “I feel fine. Previously, it was necessary to take the pills strictly twice a day. Now doctors have prescribed a different scheme, so I can take medicine only once a day. I need to stay healthy for my children and be able to help them. I do not talk widely about my diagnosis, but I don’t hide it. I think I was seen by many at HIV prevention events and trainings.”
Ms Sharipova leads a group for women—“We have female consultants working with women and men work with men. When people first learn about their HIV-positive status, they usually feel confused and scared, do not know what to do next. We talk to them, invite them to our self-help groups, explain the therapy, the future. Sometimes it is challenging to work with them, but I always say: we must move forward, only forward.”
Photography: Nazim Kalandarov/UNAIDS
Our work
Region/country
Related
 Status of HIV programmes in Tajikistan
Status of HIV programmes in Tajikistan

05 March 2025
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025



