HIV testing and counselling

Feature Story
Chatbot answers young people’s questions about HIV, health and relationships
15 October 2020
15 October 2020 15 October 2020A chatbot named Eli that can answer questions about growing up, love, relationships and sexual health, including HIV prevention and treatment, has been launched on the VKontakte social network, adding to the resources for health available to young people in eastern Europe and central Asia.
Created by the United Nations Educational, Scientific and Cultural Organization (UNESCO) Institute for Information Technologies in Education (IITE), Eli answers questions on six topics—psychology, physiology, sex, relationships, family and health. The knowledge base was created by an editorial team in collaboration with health workers and psychologists using materials on, for example, sexual and reproductive health, psychological well-being and HIV prevention, testing and treatment from UNESCO, UNAIDS and other United Nations agencies.
A large proportion of Eli’s knowledge base is on HIV prevention, testing and treatment. In a dialogue with a user, Eli explains why young people who have sex may need to be tested for HIV, what kind of tests are available, where and how they can be done and why it is crucial to start antiretroviral therapy immediately if the test results show that the person is HIV-positive. Eli helps to overcome fears and concerns and motivates its users to seek medical help.
“The use of modern innovative information technologies is an indispensable element of successful HIV education and prevention among young people, and UNESCO remains the leader in this area,” said Alexander Goliusov, Director, a.i., of the UNAIDS Regional Support Team for Eastern Europe and Central Asia.
Machine learning technologies were used to create the chatbot. Users can ask Eli a question of their own or choose one of the suggested questions. Artificial intelligence powers the response, taking into account possible connections—for example, when talking about sexually transmitted infections, Eli will give information about symptoms and diagnostic methods and will also tell the user what to do if his or her partner does not want to use protection.
Eli’s language combines expertise and respect for the user and its speech is as gender neutral as possible and free from stigma.
“Eli is an irreplaceable assistant for those who are growing up and discovering new feelings and relationships and who often need truthful information without edification and stereotypes. Eli is another step in implementing UNESCO's global strategy to empower girls and boys to increase their health literacy and to build and maintain healthy, respectful and rewarding relationships,” said Tigran Yepoyan, Head of ICT and Health Education at UNESCO IITE.
In the first week after its launch, more than 4000 people subscribed to the Eli VKontakte group and Eli answered more than 150 000 questions from 10 000 users. People also shared their feedback: “Cool and important topic!” “Eli learns and shares it with us! Go for it, Bot!” “This is very cool guys!” “I would like to thank the creators of this project. You are doing great!”
Eli is available right now and instructions are available for those who have never used such a service.
Eli will serve as a prototype for the creation of similar chatbots in Russian and in the national languages of Kazakhstan and Kyrgyzstan this year and in the languages of other countries in eastern Europe and central Asia in the future.
Our work
Additional information
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025

Feature Story
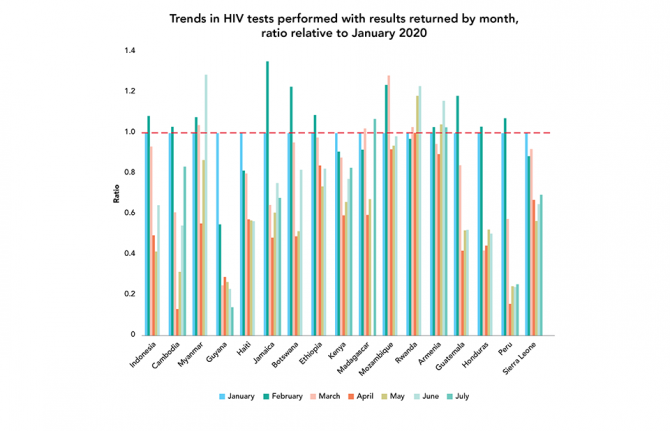
COVID-19 impacting HIV testing in most countries
13 October 2020
13 October 2020 13 October 2020Monthly data routinely reported to UNAIDS on disruptions to HIV testing and treatment services have found significant decreases in HIV testing services in nearly all countries with available data.
Since the start of the COVID-19 pandemic, UNAIDS, the World Health Organization and the United Nations Children's Fund have collected data from countries through an online platform (https://hivservicestracking.unaids.org) to identify national, regional and global disruptions of routine HIV services caused by COVID-19.
Fifty-six countries reported at least one month of HIV testing data to the platform between January and July 2020, with 17 supplying enough data to calculate trends over time. To measure the impact of COVID-19 on HIV testing services, a ratio was calculated relative to January—for example, if the number of tests in April was the same as in January, the ratio is 1; if there was a decline, the ratio is less than 1.
Large, sustained decreases in HIV testing services have been seen across all countries except Rwanda, with reduced services reported for most countries starting in April. Five countries, Myanmar, Mozambique, Madagascar, Rwanda and Armenia, have rebounded to pre-COVID-19 testing levels, while in other countries, such as Guyana and Peru, testing remains low.
Our work

Update
New HIV infections: men outnumber women
12 October 2020
12 October 2020 12 October 2020Men living with HIV are less likely to access HIV testing and antiretroviral therapy, and they also experience higher levels of new HIV infections.
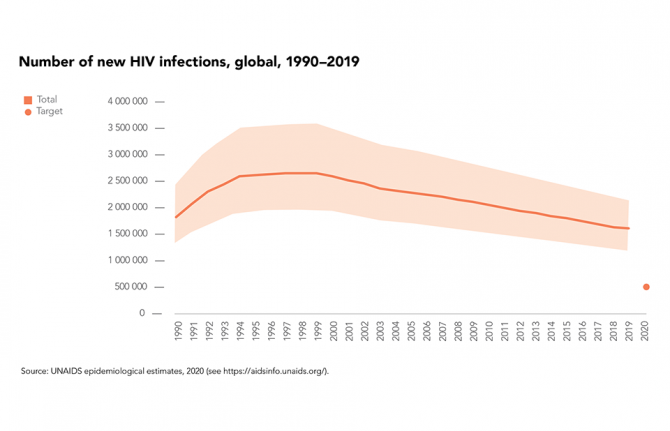
In 2019, the estimated 1.7 million people who acquired HIV worldwide marked a 23% decline in new HIV infections since 2010, although progress on HIV prevention remains far too slow, with the estimated total number of new infections in 2019 more than three times higher than the milestone of 500 000 that was set for 2020.
There were fewer new HIV infections in 2019 worldwide among women and girls (48% of total infections) than among men and boys (52%) in 2019—globally the annual number of new infections has been falling more rapidly among women and girls (a 27% decrease since 2010) than among men and boys (an 18% decrease).
Number of new HIV infections by sex, global, 2019-2019. Source: UNAIDS epidemiological estimates, 2020
RESOURCES

Update
Women living with HIV are more likely to access HIV testing and treatment
05 October 2020
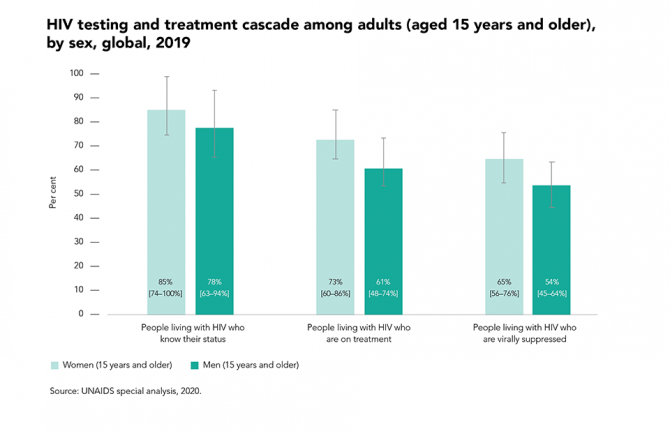
05 October 2020 05 October 2020In nearly all regions, women living with HIV are more likely to access HIV testing and antiretroviral therapy than men, in part due to better health-seeking behaviour among women and the existence of HIV-related services designed specifically to reach women (such as services to prevent mother-to-child HIV transmission that are provided during antenatal care).
In 2019, treatment coverage globally was 12 percentage points higher among women living with HIV than among men living with HIV, and viral suppression was 10 percentage points higher. This treatment gap among men living with HIV contributes to the higher number of new HIV infections among women in sub-Saharan Africa. Recent longitudinal studies have shown how closing these gaps accelerates declines in the incidence of HIV among women, especially young women.
Resources
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025


Feature Story
HIV recency testing programme launched in eastern Europe and central Asia
25 September 2020
25 September 2020 25 September 2020A new project aimed at helping countries to incorporate recency testing into national HIV reporting systems has been launched by UNAIDS in seven countries of eastern Europe and central Asia.
A recency test is a laboratory-based test that detects whether an HIV infection is recent (less than six months) or not. The incorporation of HIV recency testing in national HIV case reporting systems will help to assess how HIV is being transmitted, describe behaviours that are facilitating HIV transmission and optimize HIV-related data collection and information on risk factors.
Many countries in eastern Europe and central Asia report that despite significant progress in the epidemiological surveillance, prevention and treatment of HIV, a substantial number of new HIV diagnoses are made late. In Armenia, for example, according to national data, almost 66% of all new diagnoses of HIV infection in 2019 were made at the stage when the CD4 count was less than 350 cells/mm3 (in Kyrgyzstan, the percentage was 53%, while in Tajikistan it was 56%).
“The average time from infection to the moment a person enters the health-care system in the region varies from five to seven years,” said Lev Zohrabyan, a UNAIDS Regional Strategic Information Adviser. “All those few years, a person could be putting at risk his or her own health and the health of a partner. Moreover, prevention measures are often based on old data on transmission.”
By determining recent infections among people newly diagnosed as living with HIV, countries can identify the geographic areas and subpopulations where HIV transmission is happening. They can then effectively interrupt HIV transmission by building evidence-informed policies, guiding resources to the right place and measuring the impact of HIV prevention programmes.
“We often understand the situation as it was—what happened five years ago. This test allows us to identify and characterize cases that occurred a maximum of six months ago. Thanks to this system, we may better understand where the latest cases of HIV infection occurred,” said Meerim Sarybaeva, UNAIDS Country Manager for Kyrgyzstan.
After a multicountry study, the testing has been thoroughly evaluated and discussed with national partners with the aim of developing the most effective way of incorporating HIV recency testing into national HIV case reporting systems. The innovative technology has been transferred to national experts through extensive training programmes provided by UNAIDS for epidemiologists and laboratory experts.
This innovative approach is being integrated into routine HIV surveillance in several countries in eastern Europe and central Asia in the framework of the UNAIDS Regional Cooperation Programme (RCP) for Technical Assistance on HIV and Other Infectious Diseases, funded by the Government of the Russian Federation. The RCP aims to strengthen health systems, ensure better epidemiological surveillance of HIV and promote the scale up of HIV prevention programmes among key populations at higher risk in Armenia, Belarus, Kyrgyzstan, Tajikistan and Uzbekistan.
Our work
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025

Update
90–90–90: good progress, but the world is off-track for hitting the 2020 targets
21 September 2020
21 September 2020 21 September 2020In 2016, the United Nations General Assembly’s Political Declaration on Ending AIDS committed countries to the 90–90–90 targets, which aim to bring HIV testing and treatment to the vast majority of people living with HIV by the end of 2020 and to reduce the amount of HIV in their bodies to undetectable levels, so they keep healthy and to prevent the further spread of the virus.
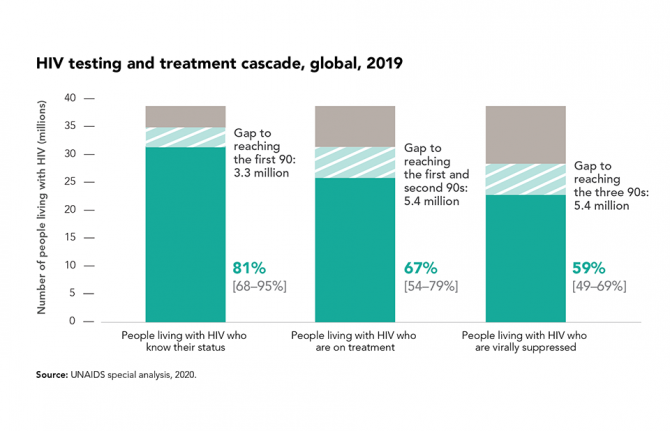
Globally, there have been remarkable gains across the HIV testing and treatment cascade. At the end of 2019, 81% of people living with HIV knew their HIV status, and more than two thirds (67%) were on antiretroviral therapy, equal to an estimated 25.4 million of the 38.0 million people living with HIV—a number that has more than tripled since 2010.
Gains in treatment effectiveness, as well as increases in the number of people who know their status and are on treatment, are reflected in the fact that viral load suppression levels among all people living with HIV increased by 18 percentage points between 2015 and 2019. Almost 59% of people living with HIV globally had suppressed viral loads in 2019. However, achieving the 90–90–90 targets results in a minimum of 73% of people living with HIV having suppressed viral loads, so the global target for the end of 2020 is unlikely to be met.
The COVID-19 pandemic also could have an impact on viral load. Early modelling showed that a severe disruption in HIV treatment could result in additional AIDS-related deaths in sub-Saharan Africa. Some countries have reported reductions in medicine collections of up to 20% in some areas and there have been multiple reports of people living with HIV not having enough antiretroviral medicine for a lockdown of more than 60 days, as well as reports of people having abandoned their HIV treatment due to a lack of food. However, monthly data from January to June 2020 reported by countries to UNAIDS have not shown substantial declines in the numbers of people currently on treatment over the six-month period.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025


Feature Story
“Do not guess, get tested” - Free testing for HIV, syphilis, and hepatitis B and C in Yerevan
27 August 2020
27 August 2020 27 August 2020In Yerevan, the capital of Armenia, all polyclinics are now providing free, anonymous, and fast testing for HIV, Syphilis, Hepatitis B and C as part of the “Do not guess, get tested” campaign launched by the Ministry of Health and the Yerevan Municipality on World Hepatitis Day.
“It is an important signal to the population that we keep providing all necessary HIV services to people and that the COVID-19 pandemic has not stopped our prevention and testing work,” said Alexander Bazarchyan, Director of the National Institute of Health.
In preparation for this initiative, the Ministry of Health together with the National Institute of Health and the Municipality of Yerevan, conducted training sessions for medical staff in 20 polyclinics in Yerevan. More than 300 health workers—family doctors, infectious disease specialists, general practitioners, laboratory specialists, etc—received theoretical and practical information on “Management skills of Tuberculosis, Hepatitis B and C” and “HIV testing and counselling services in primary healthcare facilities”.
The activities continued during the COVID-19 epidemic through an educational website developed with support from UNAIDS. The site is a platform where specialists can post accredited online courses so that health professionals can continue their education for free.
In addition, rapid tests for HIV, Syphilis, Hepatitis B and C were purchased within the framework of the UNAIDS Regional Cooperation Programme (RCP) for Technical Assistance on HIV and other Infectious Diseases funded by the Government of the Russian Federation. The RCP aims to strengthen health systems, ensure better epidemiological surveillance of HIV, and promote the scale up of HIV prevention programmes among key populations at higher risk in Armenia, Belarus, Kyrgyzstan, Tajikistan, and Uzbekistan.
“We welcome such timely support as this initiative can facilitate access to testing for people through primary healthcare services and make another step towards achieving Armenia’s commitments to increase access to early diagnosis and treatment,” said Roza Babayan, UNAIDS Representative in Armenia.
Region/country
Related
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025
Documents
2020 Global AIDS Update — Seizing the moment — Tackling entrenched inequalities to end epidemics
06 July 2020
UNAIDS report on the global AIDS epidemic shows that 2020 targets will not be met because of deeply unequal success; COVID-19 risks blowing HIV progress way off course. Missed targets have resulted in 3.5 million more HIV infections and 820 000 more AIDS-related deaths since 2015 than if the world was on track to meet the 2020 targets. In addition, the response could be set back further, by 10 years or more, if the COVID-19 pandemic results in severe disruptions to HIV services.
Visit the special page to read this report interactively and access all related materials
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025

Press Release
UNAIDS report on the global AIDS epidemic shows that 2020 targets will not be met because of deeply unequal success; COVID-19 risks blowing HIV progress way off course
06 July 2020 06 July 2020Missed targets have resulted in 3.5 million more HIV infections and 820 000 more AIDS-related deaths since 2015 than if the world was on track to meet the 2020 targets. In addition, the response could be set back further, by 10 years or more, if the COVID-19 pandemic results in severe disruptions to HIV services.
GENEVA, 6 July 2020—A new report by UNAIDS shows remarkable, but highly unequal, progress, notably in expanding access to antiretroviral therapy. Because the achievements have not been shared equally within and between countries, the global HIV targets set for 2020 will not be reached. The report, Seizing the moment, warns that even the gains made could be lost and progress further stalled if we fail to act. It highlights just how urgent it is for countries to double down and act with greater urgency to reach the millions still left behind.
“Every day in the next decade decisive action is needed to get the world back on track to end the AIDS epidemic by 2030,” said Winnie Byanyima, the Executive Director of UNAIDS. “Millions of lives have been saved, particularly the lives of women in Africa. The progress made by many needs to be shared by all communities in all countries. Stigma and discrimination and widespread inequalities are major barriers to ending AIDS. Countries need to listen to the evidence and step up to their human rights responsibilities.”
Fourteen countries have achieved the 90–90–90 HIV treatment targets (90% of people living with HIV know their HIV status, of whom 90% are on antiretroviral treatment and of whom 90% are virally supressed), including Eswatini, which has one of the highest HIV prevalence rates in the world, at 27% in 2019, and which has now surpassed the targets to achieve 95–95–95.
Millions of lives and new infections have been saved by the scale-up of antiretroviral therapy. However, 690 000 people died of AIDS-related illnesses last year and 12.6 million of the 38 million people living with HIV were not accessing the life-saving treatment.
“We cannot rest on our successes, nor be discouraged by setbacks. We must ensure that no one is left behind. We must close the gaps. We are aiming for 100–100–100,” said Ambrose Dlamini, the Prime Minister of Eswatini.
The world is far behind in preventing new HIV infections. Some 1.7 million people were newly infected with the virus, more than three times the global target. There has been progress in eastern and southern Africa, where new HIV infections have reduced by 38% since 2010. This is in stark contrast to eastern Europe and central Asia, which has seen a staggering 72% rise in new HIV infections since 2010. New HIV infections have also risen in the Middle East and North Africa, by 22%, and by 21% in Latin America.
Seizing the moment shows unequal progress, with too many vulnerable people and populations left behind. Around 62% of new HIV infections occurred among key populations and their sexual partners, including gay men and other men who have sex with men, sex workers, people who inject drugs and people in prison, despite them constituting a very small proportion of the general population.
Stigma and discrimination, together with other social inequalities and exclusion, are proving to be key barriers. Marginalized populations who fear judgement, violence or arrest struggle to access sexual and reproductive health services, especially those related to contraception and HIV prevention. Stigma against people living with HIV is still commonplace. At least 82 countries criminalize some form of HIV transmission, exposure or non-disclosure, sex work is criminalized in at least 103 countries and at least 108 countries criminalize the consumption or possession of drugs for personal use.
Women and girls in sub-Saharan Africa continue to be the most affected and accounted for 59% of all new HIV infections in the region in 2019, with 4500 adolescent girls and young women between 15 and 24 years old becoming infected with HIV every week. Young women accounted for 24% of new HIV infections in 2019, despite making up only 10% of the population in sub-Saharan Africa.
However, where HIV services are comprehensively provided, HIV transmission levels are reduced significantly. In Eswatini, Lesotho and South Africa, a high coverage of combination prevention options, including social and economic support for young women and high levels of treatment coverage and viral suppression for previously unreached populations, have narrowed inequality gaps and driven down the incidence of new HIV infections.
The COVID-19 pandemic has seriously impacted the AIDS response and could disrupt it more. A six-month complete disruption in HIV treatment could cause more than 500 000 additional deaths in sub-Saharan Africa over the next year (2020–2021), bringing the region back to 2008 AIDS mortality levels. Even a 20% disruption could cause an additional 110 000 deaths.
“Those of us who survived HIV and fought for life and access to treatment and care cannot afford losing the gains that took so much effort to win. In some Latin American countries we are seeing how HIV resources, medicines, medical staff and equipment are being moved to the fight against COVID-19,” said Gracia Violeta Ross, President of the Bolivian Network of People Living with HIV. “Some good lessons and practices of the HIV response, such as meaningful participation and accountability, are being ignored. We will not allow HIV to be left behind.”
To fight the colliding epidemics of HIV and COVID-19, UNAIDS and partners are leading a global call for a People’s Vaccine for COVID-19, which has been signed by more than 150 world leaders and experts demanding that all vaccines, treatments and tests be patent-free, mass produced and distributed fairly and free for all.
UNAIDS is also urging countries to increase investments in both diseases. In 2019, funding for HIV fell by 7% from 2017, to US$ 18.6 billion. This setback means that funding is 30% short of the US$ 26.2 billion needed to effectively respond to HIV in 2020.
“We cannot have poor countries at the back of the queue. It should not depend on the money in your pocket or the colour of your skin to be protected against these deadly viruses,” said Ms Byanyima. “We cannot take money from one disease to treat another. Both HIV and COVID-19 must be fully funded if we are to avoid massive loss of life.”
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 22 791 1697 / +41 79 514 6896
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org
Press centre
Download the printable version (PDF)
Documents
Report of the UNAIDS Executive Director — Opening of the 46th meeting of the UNAIDS Programme Coordinating Board
23 June 2020
2020 is a critical year for our Joint Programme as we collectively define the path to getting back on track to ending the AIDS epidemic by 2030. Our revised timelines for adoption of the next strategy are highly ambitious. We need the full support of all the tremendously dedicated people in UNAIDS-within our staff, our board and all our stakeholders to make this happen.