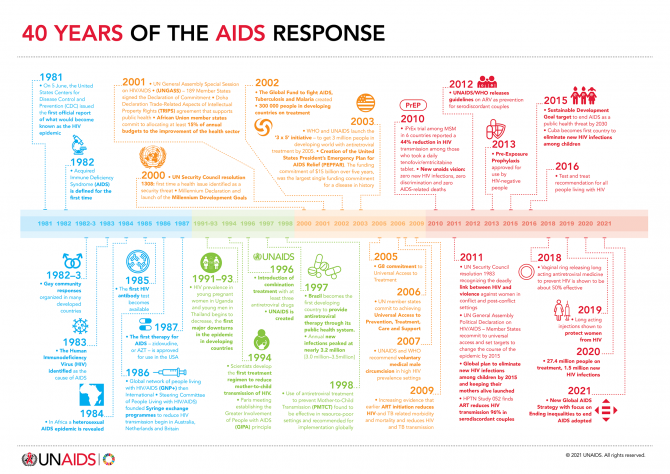
40 years of the AIDS response
HIV testing and counselling
14 July 2021
UNAIDS report shows that people living with HIV face a double jeopardy, HIV and COVID-19, while key populations and children continue to be left behind in access to HIV services. Read the press release | Data slides | This document is also available in Arabic

06 March 2025

27 February 2025

18 February 2025


10 December 2021
10 December 2021 10 December 2021Despite the remarkable progress made in the AIDS response in Africa, considerable gaps and challenges remain for achieving the 95–95–95 testing and treatment targets by 2025 and putting the continent on track to ending the AIDS epidemic by 2030. UNAIDS, the World Health Organization (WHO) and partners came together at a satellite session at the 2021 International Conference on AIDS and STIs in Africa to discuss how differentiated service delivery can bring the world closer to the targets.
People-centred differentiated service delivery is critical to accelerating access to and uptake of HIV testing and treatment services. While the COVID-19 pandemic has made many countries adapt HIV services to include delivery outside health facilities and by communities, and by scaling up multimonth dispensing of HIV and other medicines, it has also revealed a lack of resilience in key areas of systems for health, including the ability to ensure uninterrupted supplies of medicines and commodities, adequate funding for community-led organizations to provide services and support and the provision of integrated services for multiple health conditions. These adaptations and gaps have underlined the feasibility and importance of delivering differentiated, decentralized, integrated and community-based models of testing and treatment services across different settings.
During the session, representatives of ministries of health and communities, programme implementers, researchers and development partners highlighted ways in which differentiated service delivery has enhanced national efforts to reach their testing and treatment targets for all relevant population groups. They also presented new partnerships, tools, policies and best practices, and called attention to important policy shifts and innovations for scaling up differentiated service delivery, such as targeted community testing and self-testing for HIV, wider spacing of antiretroviral therapy dispensing and clinic visits, community antiretroviral therapy distribution and peer support for linkage to and retention in care for key and vulnerable populations.
“We see huge differences in testing and treatment uptake in different populations across different settings in Africa. For example, children are lagging behind adults, men are lagging behind women, and key populations living with HIV are lagging behind the general population of people living with HIV. Ensuring people- and community-centred differentiated service delivery approaches that respond to barriers to access and the diverse needs across all relevant populations together with conventional facility-based service delivery is critical to leaving no one behind,” said Ani Shakarishvili, UNAIDS Special Adviser, Access to Treatment, Care and Integration.
In April 2021, WHO released new guidelines on HIV prevention, testing, treatment, service delivery and monitoring. Updated service delivery recommendations include the initiation of antiretroviral therapy outside of the health facility, clinic visit spacing and dispensing of antiretroviral therapy every three to six months. The criteria for when a person is eligible to benefit from differentiated service delivery for HIV treatment have also been updated.
“The changes that have been made allow more people to access differentiated services for HIV treatment earlier in order to support their retention in care, meeting their needs and preferences and moving away from one-size-fits-all to more person-centred approaches,” said Clarice Pinto, a consultant on differentiated service delivery for HIV treatment at WHO.
On implementing and scaling differentiated models in countries, Anthony Ashinyo, the Deputy Programme Manager for the National AIDS/STI Control Programme in Ghana, underlined the need for multisectoral collaboration and partnerships between the government, implementers and communities to increase the uptake of differentiated service delivery.
“I see us being in the driving seat. I see us strengthening the influence of people living with HIV, recipients of care and affected communities in the design and implementation of national strategies and plans, so that they adequately reflect and respond to our lived realities and needs,” said Elsie Ayeh, the President of the Network of Persons Living with HIV/AIDS, Ghana.
The session concluded with the launch of a call to action to leave no one behind by scaling up differentiated HIV testing and treatment service delivery in Africa.
Read more about the session and watch pre-recorded presentations on differentiated service delivery from the speakers here.

27 February 2025
30 January 2025

21 January 2025
02 December 2024
26 November 2024
29 November 2021
This document is also available in Arabic

27 February 2025
30 January 2025
29 November 2021

GENEVA, 29 November 2021—UNAIDS issued a stark warning today that if leaders fail to tackle inequalities the world could face 7.7 million* AIDS-related deaths over the next 10 years. UNAIDS further warns that if the transformative measures needed to end AIDS are not taken, the world will also stay trapped in the COVID-19 crisis and remain dangerously unprepared for the pandemics to come.
“This is an urgent call to action,” said UNAIDS Executive Director Winnie Byanyima. “Progress against the AIDS pandemic, which was already off track, is now under even greater strain as the COVID-19 crisis continues to rage, disrupting HIV prevention and treatment services, schooling, violence-prevention programmes and more. We cannot be forced to choose between ending the AIDS pandemic today and preparing for the pandemics of tomorrow. The only successful approach will achieve both. As of now, we are not on track to achieve either.”
The warning comes in a new report by UNAIDS launched ahead of World AIDS Day (1 December) entitled Unequal, unprepared, under threat: why bold action against inequalities is needed to end AIDS, stop COVID-19 and prepare for future pandemics.
Some countries, including some with the highest rates of HIV, have made remarkable progress against AIDS, illustrating what is feasible. However, new HIV infections are not falling fast enough globally to stop the pandemic, with 1.5 million new HIV infections in 2020 and growing HIV infection rates in some countries. Infections are also following lines of inequality. Six in seven new HIV infections among adolescents in sub-Saharan Africa are occurring among adolescent girls. Gay men and other men who have sex with men, sex workers and people who use drugs face a 25–35 times greater risk of acquiring HIV worldwide.
COVID-19 is undercutting the AIDS response in many places. The pace of HIV testing declined almost uniformly and fewer people living with HIV initiated treatment in 2020 in 40 of 50 countries reporting to UNAIDS. HIV prevention services have been impacted—in 2020, harm reduction services for people who use drugs were disrupted in 65% of 130 countries surveyed.
“It is still possible to end the epidemic by 2030,” affirmed United Nations Secretary-General António Guterres in his World AIDS Day message. “But that will require stepped up action and greater solidarity. To beat AIDS—and build resilience against the pandemics of tomorrow—we need collective action.”
This new report from UNAIDS examines five critical elements of the plan agreed by Member States at the United Nations General Assembly High-Level Meeting on AIDS that must be urgently implemented to halt the AIDS pandemic and which are critical but under-funded and under-prioritized for pandemic prevention, preparedness and response. These include:
The call for upscaled investments and shifts in laws and policies to end the inequalities that drive AIDS and other pandemics is backed by leaders in global health and pandemic response from across the world.
“If we do not take the steps needed to tackle the inequalities driving HIV today, not only will we fail to end the AIDS pandemic, we will also leave our world dangerously unprepared for future pandemics,” said Helen Clark, Co-Chair of the Independent Panel for Pandemic Preparedness and Response, in a special foreword to the UNAIDS report. “Pandemics find space to grow in the fractures of divided societies. The amazing scientists, doctors, nurses and communities who work to end pandemics cannot succeed unless world leaders take the steps that will enable them to do so.”
UNAIDS and global health experts emphasize that while business as usual would kill millions and leave the world trapped with colliding pandemics going on for decades, leaders can, by acting boldly and together to tackle the inequalities in which pandemics thrive, end AIDS, overcome the COVID-19 crisis and be protected from the pandemic threats of the future.
“Pathogens ranging from HIV to the virus behind COVID-19 invade the cracks and fissures in our society with startling opportunism,” said Paul Farmer of Partners in Health, a nonprofit that for decades has effectively treated AIDS in settings of material poverty. “That the AIDS pandemic is shaped by deep structural inequalities need not resign us to inaction, however. Our teams, in rural Haiti and across the world, have routinely shown that with comprehensive care delivery, robust forms of accompaniment and social support and a larger dose of social justice, disparities in HIV outcomes can be rapidly narrowed, and health systems swiftly strengthened. We shouldn’t settle for anything less.”
This year marks 40 years since the first cases of AIDS were reported. Since that time, where investments have met ambition, there has been huge progress, particularly in expanding access to treatment. By June 2021, 28.2 million people had access to HIV treatment, up from 7.8 million in 2010, although progress has slowed considerably.
Countries with laws and policies aligned to evidence, strong community engagement and participation and robust and inclusive health systems have had the best outcomes, whereas the regions with the largest resource gaps and countries with punitive laws and that have not taken a rights-based approach to health have fared the worst.
“We know what works from seeing brilliant AIDS responses in some places,” said Ms Byanyima, “but we need to apply that everywhere for everyone. We have an effective strategy that leaders adopted this year, but it needs to be implemented in full. Ending inequalities to end AIDS is a political choice that requires bold policy reforms and requires money. We have reached a fork in the road. The choice for leaders to make is between bold action and half-measures.”
* The estimate of 7.7 million AIDS-related deaths between 2021 and 2030 is what UNAIDS models predict if HIV service coverage is held constant at 2019 levels. If the Global AIDS Strategy 2021–2026: End Inequalities, End AIDS is executed and the 2025 targets are achieved, UNAIDS estimates that at least 4.6 million of those deaths can be averted over the decade.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.




The President of Senegal, Macky Sall, pledges an additional $3.5 million to support the HIV response and the call for action
DAKAR/GENEVA, 3 November 2021—A three-day regional summit on HIV/AIDS held in Dakar, Senegal, has concluded with a call to action that urges stronger support for community-led responses, policies driven by science and data, increased investment in the HIV response and putting HIV at the centre of pandemic preparedness and response. In his closing remarks, the President of Senegal, Macky Sall, committed to advancing the call to action with the African Union and pledged additional funds to implement it in Senegal and across the region.
Western and Central Africa is home to 4.7 million people living with HIV—12% of those living with HIV globally—but experiences 22% of all HIV deaths in the world. Countries in the region, on average, have seen slower declines in HIV infections than other countries on the continent and HIV prevalence in women is significantly higher than in men. Access to HIV testing and treatment reached 73% of people living with HIV in 2020, up from 38% in 2015, but short of the 81% goal that was set for 2020. The region has the world’s highest number of HIV-positive pregnant women still waiting for treatment, and just 24% of children living with HIV were virally suppressed.
The Dakar Call to Reinvent the Response to the HIV Pandemic calls for urgent action in four main areas:
1. Expand community-led infrastructure and organizations to strengthen national systems for health and shift policies to enable sustained funding for community organizations. Too many of the most vulnerable people in Western and Central Africa region do not have access to conventional health systems. Evidence shows community-led organizations and networks are critical to filling the gaps. This includes expanding the provision of HIV treatment and prevention services by community-led organizations in partnership with the public health system, ensuring that organized civil society and affected communities are included as key partners in decision-making bodies, and building accountability structures such as community-led monitoring.
2. Update health policies to align with the latest HIV science and evidence. Countries that have aligned their HIV policies and programmes with the current science have made greater progress against HIV/AIDS. Governments are urged to review their health policies in consideration of the latest scientific data and evidence. This is as a key step to improve the HIV response, and particularly to address the needs of those most vulnerable to HIV.
3. Increase national and international resources for HIV in the region by 33% by 2025 and remove financial barriers to access health services by people living with HIV. UNAIDS studies show that $2.67 billion by 2025, representing a 33% increase, would ensure sufficient funding for a comprehensive response to HIV in the region. Insufficient progress in the response to the HIV pandemic is only increasing the long-term costs that will strain already overburdened health budgets.
4. Put HIV and COVID-19 at the centre of pandemic preparedness and response. Many of the measures needed to accelerate the HIV response will also help prevent future pandemics. These measures include strengthening and protecting the formal and informal health workforce, collecting quality epidemic data to inform decision-making, implementing rights-based responses, and ensuring equitable access to new medical technologies.
These four actions are achievable in the next three years and would move the region closer to the 2025 global target of 95% of people knowing their HIV status; 95% of people who know their HIV status initiating treatment; 95% of people on treatment being virally suppressed. They would contribute to a dramatic reduction in the number of AIDS-related deaths and new HIV infections in the region.
Western and Central Africa has been at the forefront of some of the most innovative and successful efforts in the global response to HIV. Ending the AIDS epidemic as part of the 2030 Sustainable Development Agenda remains a priority even though the region faces multiple challenges including the response to the COVID-19 pandemic, numerous economic and security crises, and climate change.
During the summit governments, civil society actors, community-led organizations, scientists, and other partners reviewed new data and progress against HIV in the last 5 years and took note of the new UNAIDS Global AIDS Strategy 2021-2026 and the United Nations General Assembly Political Declaration on HIV and AIDS: Ending Inequalities and Getting on Track to End AIDS by 2030. The summit was co-organized by UNAIDS and the Civil Society Institute of HIV and Health in Western and Central Africa and hosted by the President of Senegal, Macky Sall. It was held with the support of Luxembourg and the Bill and Melinda Gates Foundation.
“The key word today more than ever is mobilization. Let us mobilize for funding, for research and for vaccination. I am committed to working with you to advocate with the African Union and with partners to ensure that funding for the fight against HIV is strengthened and that this strengthening can begin with our African states themselves. I commit 2 billion CFA ($3.5 million) more in the fight against HIV, of which one billion will be given to the community fight by civil society and the other billion will go to the National AIDS Council to help people living with HIV.”
“Evidence shows the AIDS response is most effective when community-led organizations provide services as an integral part of the public response, are involved as co-planners, can highlight experiences and concerns, and play their essential role to ensure accountability. This conference issues a bold call to remove legal, policy and programmatic barriers that hold the region back from ending AIDS and to scale up resources to unleash the power of local organizations to help us end AIDS-related deaths and stop HIV infections.”
“This was an important development for West and Central Africa as the government of Senegal and UNAIDS co-hosted this high-level summit with civil society as equal partners-- showing what can happen when government, international stakeholders and civil society join together to respond to a pandemic.”
“If we want to achieve the SDGs, we need to increase public support for development. We need to strengthen systems that have suffered during the COVID-19 pandemic and make health systems more resilient.”
“We know that pandemics such as COVID-19, HIV and tuberculosis both exacerbate and thrive on inequalities—the world must take action to tackle inequalities and other barriers to health to end the HIV epidemic.”
“Paediatric care is weak in our region. Children born with HIV too often die from AIDS-related illnesses. We count on your leadership and political will so that children are no longer forgotten. For civil society, Dakar represents a new beginning.”
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
24 September 2021
This brief was developed following a consultation with members of the UNAIDS Scientific and Technical Advisory Committee (STAC) and other key stakeholders following the results from four community trials in Africa that showed decreased HIV incidence (by approximately 20–30%) and decreased HIV-related mortality (by approximately 20%) within three years of implementing a community-wide universal test and connect programme compared with current standard care.
Universal test and connect is an intensive community-wide strategy to accelerate HIV epidemic transition to rapidly reduce new HIV infections and deaths from AIDS-related illnesses across a specific community. This brief captures the highlights of the core findings of the STAC meeting and is focused on explaining universal test and connect in clear terms, with an emphasis on what it is and isn’t and on what to consider if a country is interested in implementing the approach at the subnational level. It also highlights the implications of the current and possible future COVID-19 contexts on opportunities for universal test and connect.
30 January 2025
21 January 2025

20 September 2021
20 September 2021 20 September 2021Progress against HIV has been uneven. The gains made through people-centred approaches within the highest performing HIV programmes have been tempered by insufficient action in other countries.
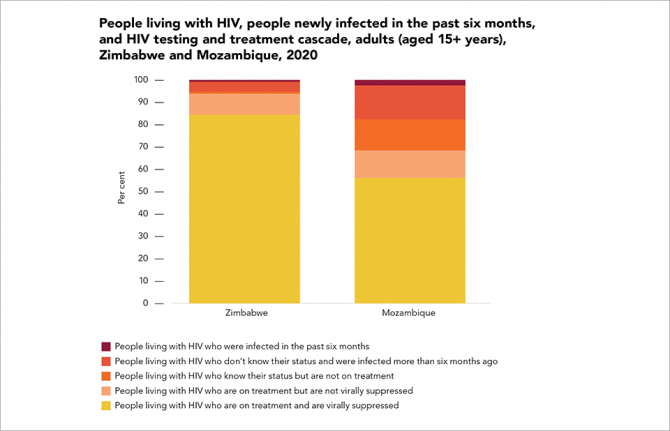
Zimbabwe has been an HIV testing and treatment leader. The southern African country’s AIDS Levy has mobilized a significant amount of domestic funding, communities are strongly engaged in service delivery and international financial and technical support has been strong and consistent. Eighty-two per cent of adults living with HIV in the country have suppressed viral loads. Neighbouring Mozambique, by contrast, has lagged behind the regional average, leaving nearly half (44%) of adults living with HIV in the country with unsuppressed viral loads. Conflict, climate change, high levels of poverty and poor health infrastructure are among the country’s many challenges.