HIV integration

Press Release
New HIV Policy Lab uses law and policy data in the HIV response
29 September 2020 29 September 2020WASHINGTON, D.C./GENEVA, 29 September 2020—Despite decades of scientific advance in the HIV response, progress remains uneven, with some countries rapidly reducing AIDS-related deaths and new HIV infections and others seeing increasing epidemics. Laws and policies are driving a significant part of that divergence.
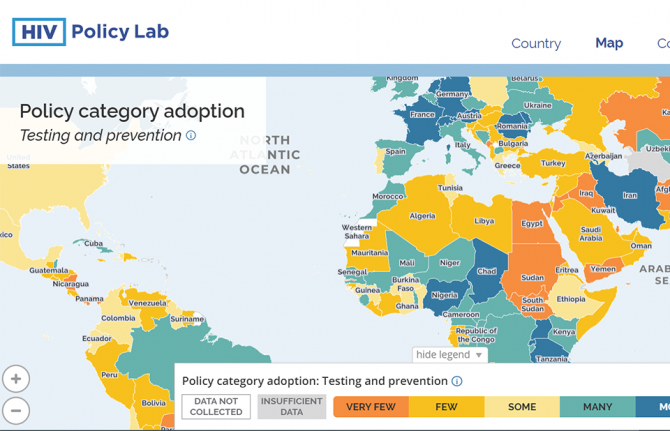
Launched today, the HIV Policy Lab is a unique initiative to gather and monitor HIV-related laws and policies around the world.
“Laws and policies are life or death issues when it comes to HIV. They can ensure access to the best that science has to offer and help people to realize their rights and live well, or they can be barriers to people’s well-being. Like anything that matters, we need to measure the policy environment and work to transform it as a key part of the AIDS response,” said Winnie Byanyima, UNAIDS Executive Director.
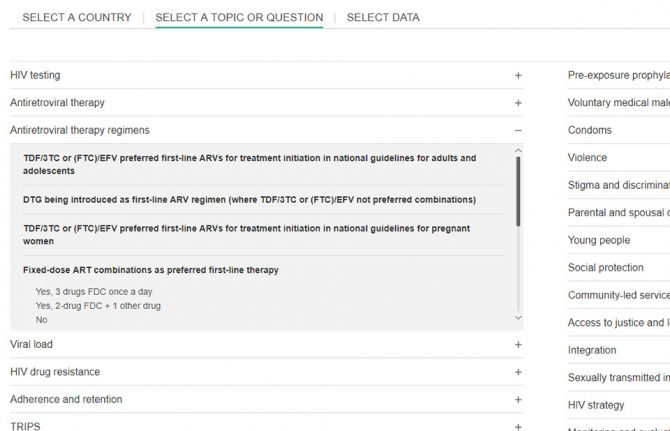
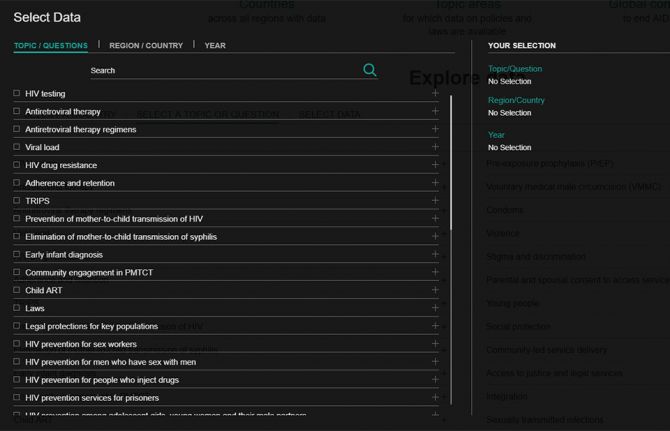
The HIV Policy Lab is a data visualization and comparison tool that tracks national policy across 33 different indicators in 194 countries around the world, giving a measure of the policy environment. The goal is to improve transparency, the ability to understand and use the information easily and the ability to compare countries, supporting governments to learn from their neighbours, civil society to increase accountability and researchers to study the impact of laws and policies on the HIV pandemic.
According to Matthew Kavanagh, Director of the Global Health Policy & Politics Initiative at Georgetown University’s O’Neill Institute, “Policy is how governments take science to scale. If we want to improve how policy is used to improve health outcomes, it is essential to monitor and evaluate the policies that comprise it.”
“Reducing stigma and making care easier to access are fundamental for improving the lives of people living with HIV—and those are all consequences of policy choices. Tracking these choices is a key tool for improving them, and ensuring justice and equity for people living with HIV,” said Rico Gustav, Executive Director of the Global Network of People Living with HIV.
The HIV Policy Lab draws information from the National Commitments and Policy Instrument, legal documents, government reports and independent analyses to create data sets that can be compared across countries and across issues. The goal of the HIV Policy Lab is to help identify and address the gaps between evidence and policy and to build accountability for a more inclusive, effective, rights-based and science-based HIV policy response.
The HIV Policy Lab is a collaboration between Georgetown University and the O’Neill Institute for National and Global Health Law, UNAIDS, the Global Network of People Living with HIV and Talus Analytics.
About the Georgetown University O’Neill Institute for National and Global Health Law
The O’Neill Institute, housed at Georgetown University, was established to create innovative solutions to the most pressing national and international health concerns, with the essential vision that the law has been, and will remain, a fundamental tool for solving critical health problems. The Georgetown University Department of International Health is home to scholarship in public health, economics, political science, and medicine. Georgetown’s Global Health Initiative serves as a university-wide platform for developing concrete solutions to the health challenges facing families and communities throughout the world. Read more at oneillinstitute.org and connect with us on Twitter and Facebook.
About UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
About GNP+
GNP+ is the global network for and by people living with HIV. GNP+ works to improve the quality of life of all people living with HIV. GNP+ advocates for, and supports fair and equal access to treatment, care and support services for people living with HIV around the world. Learn more at gnpplus.net and connect with GNP+ on Facebook, Twitter and Instagram.
Contact
O’Neill InstituteLauren Dueck
Lauren.Dueck@Georgetown.edu
UNAIDS
Sophie Barton-Knott
bartonknotts@unaids.org
GNP+
Lesego Tlhwale
ltlhwale@gnpplus.net
Press centre
Download the printable version (PDF)

Press Release
UNAIDS report on the global AIDS epidemic shows that 2020 targets will not be met because of deeply unequal success; COVID-19 risks blowing HIV progress way off course
06 July 2020 06 July 2020Missed targets have resulted in 3.5 million more HIV infections and 820 000 more AIDS-related deaths since 2015 than if the world was on track to meet the 2020 targets. In addition, the response could be set back further, by 10 years or more, if the COVID-19 pandemic results in severe disruptions to HIV services.
GENEVA, 6 July 2020—A new report by UNAIDS shows remarkable, but highly unequal, progress, notably in expanding access to antiretroviral therapy. Because the achievements have not been shared equally within and between countries, the global HIV targets set for 2020 will not be reached. The report, Seizing the moment, warns that even the gains made could be lost and progress further stalled if we fail to act. It highlights just how urgent it is for countries to double down and act with greater urgency to reach the millions still left behind.
“Every day in the next decade decisive action is needed to get the world back on track to end the AIDS epidemic by 2030,” said Winnie Byanyima, the Executive Director of UNAIDS. “Millions of lives have been saved, particularly the lives of women in Africa. The progress made by many needs to be shared by all communities in all countries. Stigma and discrimination and widespread inequalities are major barriers to ending AIDS. Countries need to listen to the evidence and step up to their human rights responsibilities.”
Fourteen countries have achieved the 90–90–90 HIV treatment targets (90% of people living with HIV know their HIV status, of whom 90% are on antiretroviral treatment and of whom 90% are virally supressed), including Eswatini, which has one of the highest HIV prevalence rates in the world, at 27% in 2019, and which has now surpassed the targets to achieve 95–95–95.
Millions of lives and new infections have been saved by the scale-up of antiretroviral therapy. However, 690 000 people died of AIDS-related illnesses last year and 12.6 million of the 38 million people living with HIV were not accessing the life-saving treatment.
“We cannot rest on our successes, nor be discouraged by setbacks. We must ensure that no one is left behind. We must close the gaps. We are aiming for 100–100–100,” said Ambrose Dlamini, the Prime Minister of Eswatini.
The world is far behind in preventing new HIV infections. Some 1.7 million people were newly infected with the virus, more than three times the global target. There has been progress in eastern and southern Africa, where new HIV infections have reduced by 38% since 2010. This is in stark contrast to eastern Europe and central Asia, which has seen a staggering 72% rise in new HIV infections since 2010. New HIV infections have also risen in the Middle East and North Africa, by 22%, and by 21% in Latin America.
Seizing the moment shows unequal progress, with too many vulnerable people and populations left behind. Around 62% of new HIV infections occurred among key populations and their sexual partners, including gay men and other men who have sex with men, sex workers, people who inject drugs and people in prison, despite them constituting a very small proportion of the general population.
Stigma and discrimination, together with other social inequalities and exclusion, are proving to be key barriers. Marginalized populations who fear judgement, violence or arrest struggle to access sexual and reproductive health services, especially those related to contraception and HIV prevention. Stigma against people living with HIV is still commonplace. At least 82 countries criminalize some form of HIV transmission, exposure or non-disclosure, sex work is criminalized in at least 103 countries and at least 108 countries criminalize the consumption or possession of drugs for personal use.
Women and girls in sub-Saharan Africa continue to be the most affected and accounted for 59% of all new HIV infections in the region in 2019, with 4500 adolescent girls and young women between 15 and 24 years old becoming infected with HIV every week. Young women accounted for 24% of new HIV infections in 2019, despite making up only 10% of the population in sub-Saharan Africa.
However, where HIV services are comprehensively provided, HIV transmission levels are reduced significantly. In Eswatini, Lesotho and South Africa, a high coverage of combination prevention options, including social and economic support for young women and high levels of treatment coverage and viral suppression for previously unreached populations, have narrowed inequality gaps and driven down the incidence of new HIV infections.
The COVID-19 pandemic has seriously impacted the AIDS response and could disrupt it more. A six-month complete disruption in HIV treatment could cause more than 500 000 additional deaths in sub-Saharan Africa over the next year (2020–2021), bringing the region back to 2008 AIDS mortality levels. Even a 20% disruption could cause an additional 110 000 deaths.
“Those of us who survived HIV and fought for life and access to treatment and care cannot afford losing the gains that took so much effort to win. In some Latin American countries we are seeing how HIV resources, medicines, medical staff and equipment are being moved to the fight against COVID-19,” said Gracia Violeta Ross, President of the Bolivian Network of People Living with HIV. “Some good lessons and practices of the HIV response, such as meaningful participation and accountability, are being ignored. We will not allow HIV to be left behind.”
To fight the colliding epidemics of HIV and COVID-19, UNAIDS and partners are leading a global call for a People’s Vaccine for COVID-19, which has been signed by more than 150 world leaders and experts demanding that all vaccines, treatments and tests be patent-free, mass produced and distributed fairly and free for all.
UNAIDS is also urging countries to increase investments in both diseases. In 2019, funding for HIV fell by 7% from 2017, to US$ 18.6 billion. This setback means that funding is 30% short of the US$ 26.2 billion needed to effectively respond to HIV in 2020.
“We cannot have poor countries at the back of the queue. It should not depend on the money in your pocket or the colour of your skin to be protected against these deadly viruses,” said Ms Byanyima. “We cannot take money from one disease to treat another. Both HIV and COVID-19 must be fully funded if we are to avoid massive loss of life.”
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 22 791 1697 / +41 79 514 6896
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org
Press centre
Download the printable version (PDF)





Feature Story
Health kiosks expanding HIV services in Zimbabwe
18 December 2019
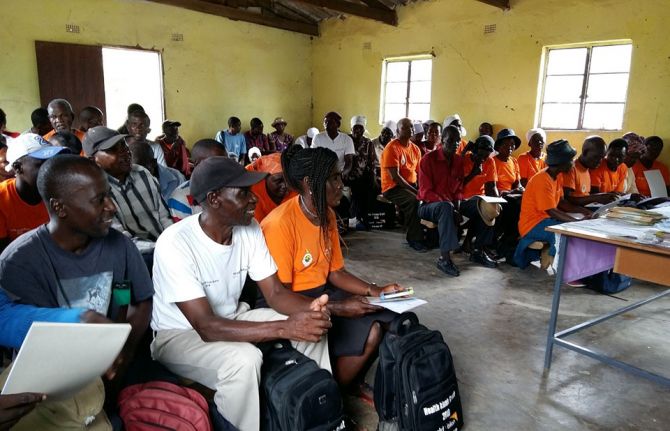
18 December 2019 18 December 2019If you drive through Zimbabwe on a typical Saturday or Sunday, you will see many places of religious worship. Some are static structures, while others are mobile. Some services are held under trees or in open spaces.
Many people in Zimbabwe follow a religious faith. The Apostolic community is a major religious sect that discouraged its members from seeking medical care, including HIV services, preferring to use prayer for healing―this led to many people becoming ill and dying from preventable diseases. However, with the implementation of so-called health kiosks, the community is now encouraging its members to access medical care.
David Adashe (not his real name), an Apostolic leader in Gokwe North, explained that health kiosks staffed by church volunteers trained by the Zimbabwe health ministry helped his congregation to access much needed information on HIV prevention. He described it as like, “Going from a thick cloud of darkness into a plane of light of splendour.”
Ms Adashe said that his congregation’s views about seeking medical assistance from health facilities have changed. They now seek out medical care, receive counselling from trained volunteers and are referred to a health facility for additional services, if needed. “I was naive and reluctant to take health issues seriously, but since the emergence of the health kiosk programme, I am now more empowered. I’m now encouraging my family to access health services from the clinic,” he said.
Since March 2018, World Vision Zimbabwe, in collaboration with the Ministry of Health and Child Care, has been empowering faith leaders like Mr Adashe and church volunteers through training and creating safe spaces to bring health information and services to their congregations.
A health kiosk volunteer in Gwanda said, “As a volunteer, I observed that previously it was difficult for some individuals to travel to the local clinic on their own to seek medical advice, but since the programme started it is easy now, since they can access the information on their doorstep through the health kiosks.”
Many faith worship centres participating in the health kiosk programme have seen a threefold increase in the uptake of HIV and health information. Half of the people requesting information on HIV take an HIV test and receive their results. People who test positive for HIV are referred for antiretroviral therapy and supported to stay in care through the help of the trained church volunteers.
Faith leaders and church volunteers are essential in controlling the HIV epidemic. They provide care for their members, create safe space for information-sharing and are trusted by their members. Regular contact with the congregations enables the volunteers to bridge the gap in services for those who need them the most. The health kiosks also serve as effective and sustainable platforms to bring together both faith and non-faith communities to address the health needs of their members and to provide safe spaces to engage on other health matters.
“The findings from the health kiosk programme are promising for addressing the HIV epidemic. This is a key example of community-led responses by, for and within faith communities providing safe spaces and support for their members. These kinds of responses are essential for ending new HIV infections and AIDS-related deaths and critical for reaching universal health coverage,” said Laurel Sprague, Chief of the UNAIDS Community Mobilization, Community Support, Social Justice and Inclusion Department.
Region/country
Related


Press Release
Global leaders unite to tackle health inequalities
09 September 2019 09 September 2019Delegates from more than 300 municipalities join global Fast-Track Cities conference on urban HIV, tuberculosis, and viral hepatitis
LONDON, UNITED KINGDOM, 9 September 2019 — London Mayor Sadiq Khan today welcomed city, municipal, and global leaders to Fast-Track Cities 2019, the inaugural conference of more than 300 cities and municipalities prioritizing their responses to urban HIV, tuberculosis (TB), and viral hepatitis. Speaking at the conference, Mayor Khan highlighted the problem of health inequalities across the world, as well as the need to end the stigma still associated with HIV. He also reiterated the bold ambition for London to achieve the target of no new HIV infections, deaths, and stigma by 2030.
“I’m honoured that city and health leaders from all around the world are uniting today in London. The first international gathering of Fast-Track Cities will be a truly historic event in our fight against HIV and health inequalities,” said Mayor Khan. “I’m also proud of the work London is doing to tackle HIV and inequality, and am pleased that we will be able to share our knowledge and experience with others. But despite our progress, there is still much more to be done as too many people continue to catch the virus. To truly end all new cases of HIV in London, it’s high time the Government made PrEP available via the NHS for all those who need it. No ifs, no buts, and no more pilots – we know it works, it stops the spread of infection and saves money in the long run.”
More than half of the world’s population currently lives in urban centers where the risk of contracting HIV, TB, and hepatitis is significantly higher due to urban dynamics such as social behavior, migration, unemployment, and social and economic inequalities. However, cities and municipalities also have inherent advantages and offer important opportunities to accelerate health responses and take transformative action to ensure that equitable access to health services is available to everyone.
“We have seen that for an effective response to HIV it is critical to remove inequalities, power imbalances, marginalization, and discrimination,” said Gunilla Carlsson, Executive Director a.i., of UNAIDS, one of four core partners of the Fast-Track Cities initiative. “Cities must use their advantages to leverage innovation, create social transformation, and build equitable societies that are inclusive, responsive, resilient, and sustainable,” she added.
Organized by the International Association of Providers of AIDS Care (IAPAC), in collaboration with the Joint United Nations Programme on HIV/AIDS (UNAIDS) and other partners, the Fast-Track Cities 2019 conference is being held from September 9-11, 2019, at the Barbican Centre. The conference’s aim is to highlight successes achieved across the Fast-Track Cities network, address cross-cutting challenges faced by local stakeholders, and share best practices in accelerating urban AIDS responses, inclusive of co-infectious diseases such as TB and viral hepatitis. The conference features plenary sessions, panel discussions, and abstract presentations by representatives from more than 300 Fast-Track Cities.
“Health inequalities are preventing people living with HIV, TB, and viral hepatitis, notably from disenfranchised and minority ethnic communities, from accessing the services they need to live longer, healthier lives," said Dr. José M. Zuniga, President/CEO of the International Association of Providers of AIDS Care (IAPAC), one of the core partners of the Fast-Track Cities initiative and the conference’s organizer. “We are convening in London because the city’s high level of political commitment, public health leadership, support from clinical and service providers, and engagement with affected communities have enabled the city to surpass the Fast-Track Cities’ programmatic HIV targets. We are here to shine a light on London’s efforts to reduce and eliminate health inequalities that contravene the principles of social justice.”
When London joined the Fast-Track Cities initiative in January 2018, the city had already met the UNAIDS 90-90-90 targets, which are defined as 90% of people living with HIV knowing their status, 90% of people who know their status accessing HIV treatment, and 90% of people accessing HIV treatment achieving viral suppression. FTC London, a pan-city group of stakeholders steering the city’s Fast-Track Cities engagement, has made outreach to the black, Asian, and minority ethnic (BAME) community a priority in their “London Getting to Zero” strategy.
The “High-Level Panel on Health Inequalities,” which was the official opening of the Fast-Track Cities 2019 conference, included the following elected officials:
- Kostas Bakoyannis (Mayor, Athens, Greece)
- Josefina Belmonte (Mayor, Quezon City, Philippines)
- Winston Ennis (Deputy Mayor, Kingston, Jamaica)
- Simone Kukenheim (Deputy Mayor, Amsterdam, Netherlands)
- Fernando Medina (Mayor, Lisbon, Portugal)
- Svante Myrick (Mayor, Ithaca, NY, USA)
- Robb Pitts (Chairman, Fulton County, Atlanta, GA, USA)
- Mykola Povoroznyk, (First Deputy Mayor, Kyiv, Ukraine)
- Gennadiy Trukhanov (Mayor, Odesa, Ukraine)
In addition to IAPAC’s Dr. Zuniga, and UNAIDS’ Ms. Carlsson, several global public health leaders also participated in the “High Level Panel on Health Inequalities,” including:
- Amb. Deborah L. Birx (US Global AIDS Coordinator, PEPFAR)
- Cary James (CEO, World Hepatitis Alliance)
- Suvanand Sahu (Deputy Executive Director, Stop TB Partnership)
- Maimunah Mohd Sharif (Executive Director, UN-Habitat)
- Trevor Stratton (Board Member, GNP+)
- Marijke Wijnroks (Chief of Staff, Global Fund to fight AIDS, TB and Malaria)
The panel was moderated by UK-based broadcaster and former BBC journalist Henry Bonsu.
Press passes for Fast-Track Cities 2019 are available by contacting IAPAC Director of Communications Zack Pesavento at zpesavento@iapac.org.
The conference program is available at: https://www.iapac.org/conferences/fast-track-cities/#program
About the International Association of Providers of AIDS Care (IAPAC)
With more than 30,000 members globally, IAPAC is the largest association of clinicians and allied health professionals working to end AIDS as a public health threat by 2030. For more information about IAPAC and our global activities, please visit: https://www.iapac.org/
About the Fast-Track Cities Initiative
Fast-Track Cities is a global partnership between almost 300 cities and municipalities, the International Association of Providers of AIDS Care (IAPAC), the Joint United Nations Programme on HIV/AIDS (UNAIDS), the United Nations Human Settlements Programme (UN-Habitat), and the City of Paris that are collaborating to end the epidemics of HIV, TB, and viral hepatitis by 2030. The initiative was launched on World AIDS Day 2014 in Paris. For more information please visit: https://www.iapac.org/fast-track-cities/about-fast-track/
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.

Feature Story
Mapping HIV laws and policies
31 July 2019
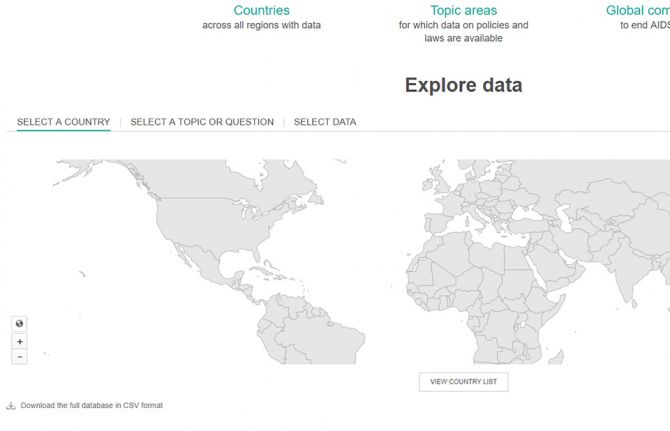
31 July 2019 31 July 2019A new website that enables people to identify national laws and policies related to the AIDS response has been launched by UNAIDS.
Covering areas as diverse as a country’s ability to diagnose HIV among young babies, the existence of laws that discriminate against transgender people and whether people are prosecuted for carrying condoms, the Laws and Policies Analytics website aims to give a full overview of a country’s laws and policies related to the HIV response. It also allows to view policy data jointly with other data on the HIV epidemic and response.
“We must better understand legal and policy environments to drive effective responses to the HIV epidemic. This new tool will provide access to data on national laws and policies and allow for joint analysis with data on the epidemic and response, so that we can drive more deeply-informed decision-making,” said Shannon Hader, UNAIDS Deputy Executive Director, Programme.
Under the 2016 United Nations Political Declaration on HIV and AIDS, countries committed to accelerate efforts to significantly increase the availability of high-quality data on HIV. The information used on the new website was reported since 2017 and most recently in 2019 through the National Commitments and Policy Instrument (NCPI), a part of the Global AIDS Monitoring mechanism through which countries report their progress against the commitments they made in the 2016 Political Declaration.
Data were provided by national authorities, civil society organizations and other nongovernmental partners engaged in the AIDS response. Data on HIV-related laws and policies compiled from other external official documents complement the nationally supplied data. UNAIDS carries out a thorough validation of all policy data included to ensure their accuracy. Data will be updated annually.
The website hosts data from over 140 countries. Users can search by country or region through an interactive map or can select a specific topic.
Through making policy data widely available, UNAIDS seeks to promote transparency and an increased use of policy data in analyses of the HIV epidemic and the response to HIV in countries worldwide.
The Laws and Policies Analytics website can be accessed at lawsandpolicies.unaids.org.
Laws and Policies Analytics website


Feature Story
Ukraine: government to fund publicly procured HIV services
18 June 2019
18 June 2019 18 June 2019Ukraine has announced that it is to allocate $16 million to the country’s AIDS response for 2019-20, which will sustain and expand HIV prevention and support services for key populations as well as care and support services for people living with HIV.
The procurement of HIV services for key populations and people living with HIV from suppliers, including non-governmental organizations, will be managed by the Ministry of Health’s Centre for Public Health, using public procurement procedures. The new process will begin in July.
The move is an important part of Ukraine’s transition from donor funding to a nationally funded AIDS response.
"Ukraine has taken an important step towards moving from international funding to a nationally coordinated policy and ownership,” said Vladimir Kurpita, director of the Centre for Public Health at the Ministry of Health.
The list of services covered by the new policy includes targeted HIV information services and consultations, harm reduction programmes, including needle exchange and distribution, the distribution of condoms and lubricants, HIV testing and screening for tuberculosis. Key populations prioritized include gay men and other men who have sex with men, sex workers, and people who inject drugs. HIV care and support services include strengthening treatment adherence and retention under medical supervision and the involvement of partners of people living with HIV in health care services.
Mr Kurpita promised a smooth transition and said that the government would procure quality-assured services from local non-governmental organizations with the relevant experience and capacity to deliver.
“Nobody who was reached through prevention, support and care services that were funded by external donors should ever be cut off from the transition to government support,” he said.
The head of the All Ukrainian Network of People Living with HIV, 100% Life, Dima Sherembey, encouraged everyone to engage in the process.
"If you are an NGO service provider, engage in bidding; if you are a representative of the donor community in Ukraine, motivate your partners and subcontractors on the ground; and if you have resources and knowledge, provide technical support and assistance to bidders so that they can be successful recipients and implementers of this important wave of government funding,” he said.
UNAIDS country director Roman Gailevich welcomed Ukraine’s commitment to increase domestic funding for the AIDS response.
“We are entering a new era of the national response to HIV in Ukraine,” he said. “We hope Ukraine will not only show that this new model of procurement of HIV services is viable, but that it will also serve as an example to other countries in the region.”
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025


Update
Out-of-pocket expenses hamper access to HIV services
06 May 2019
06 May 2019 06 May 2019User fees and other out-of-pocket expenses―defined as direct payments made by people to health-care providers at the time of service use―are a major barrier to people getting tested for HIV, to people living with HIV being treated and to people living with HIV being retained in treatment and care.
Even if antiretroviral medicines are available free of charge, fees for diagnostic tests, consultations and medicines for opportunistic infections have a huge impact on people living on a lower income. User fees have also been shown to reduce access to health services more broadly among the more vulnerable within society. Out-of-pocket payments make up substantial proportions of total health expenditure in all regions, and in some low- and middle-income countries private out-of-pocket spending is estimated to account for more than 60% of total health expenditure.
According to the World Bank, around 3.4 billion people globally who earn US$ 5.50 a day or less are just one medical bill away from sinking into poverty.
Related information
Related


Press Statement
Message on the occasion of Universal Health Coverage Day
12 December 2018 12 December 2018Health is everyone’s concern. The world has been striving for access to quality and affordable health services since the Declaration of Alma-Ata, which called for health for all more than 40 years ago.
We have come a long way since then—improvements in access to, and the quality of, health-care services have increased life expectancy globally from 62 to 72 years. Yet progress is far from equal. Today, more than half of the world’s population do not have full access to essential health services, because they are unaffordable, inadequate, inaccessible for certain groups or simply unavailable.
There is increasing inequity around the world, with the richest 1% of the population now owning half of the world’s wealth. Life expectancy in the poorest countries of the world is appreciably lower than in the wealthiest, and living in areas blighted by poverty can mean a shorter life span and a lost future. The disparity is observed between countries and between different communities within countries, with the most vulnerable, marginalized and stigmatized being left behind.
Making progress towards universal health coverage that is truly universal means making progress towards equity, inclusion and social justice. It means a people-centred, human rights-based approach and community-led service delivery, as well as a recognition of the need to address the social determinants of health, including necessary reforms of laws and policies and removing stigma and discrimination and gender inequity.
The global response to HIV has illustrated the critical measures—decisive political leadership and commitment, community engagement and a response informed by scientific evidence—that can change the course of a global epidemic.
Reaching time-bound HIV prevention and treatment targets will make an important contribution to achieving the universal health coverage targets, and together will significantly accelerate progress towards realizing the Sustainable Development Goals.
In recognition of the theme of this year’s Universal Health Coverage Day, “Unite for universal health coverage: now is the time for collective action”, I call on everyone to embrace and contribute to the universal health coverage movement. United, we can make universal health coverage a reality for all.
12 December 2018
Michel Sidibé
Executive Director of UNAIDS
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Press centre
Download the printable version (PDF)




Feature Story
Training the next generation of Russian doctors on HIV-related stigma and discrimination
30 October 2018
30 October 2018 30 October 2018Stigma and discrimination among health-care workers is among the most severe barriers that people living with HIV experience in accessing life-saving health services. In order to encourage a new generation of health-care workers in the Russian Federation to provide medical services in a non-stigmatizing and discrimination-free setting, 20 medical students from across the country are participating in a new week-long course at the Vera HIV Medical School.
“Medical students often only hear second-hand stories about how to treat or care for people living with HIV. But if they receive the right training and practical support, they can be a bridge between people at risk of HIV and access to life-saving services,” said Anton Yeremin, the course’s coordinator, who is also an infectious diseases doctor who specializes in HIV treatment and care. “If doctors unknowingly promote stigma or explicitly discriminate against people living with HIV, or people at risk of HIV, it can result in patients being denied access to treatment, or even avoiding contact with medical services," he added.
The course is designed to complement what students learn at university. “We encourage future doctors to develop skills specific to the HIV context, such as relating to patients and understanding some of the social and legal aspects of their diagnosis,” said Mr Yeremin. The course consists of lectures and workshops on non-discriminatory approaches to people living with HIV and meeting people living with HIV, doctors, lawyers, psychologists, HIV activists and representatives of nongovernmental organizations to hear their stories.
According to Dmitry Petrov, a peer counsellor at the Svetlana Izambayeva Charitable Foundation, his clients are often denied admission to hospital. “An ambulance will arrive and the ambulance crew will say we can drive him to a hospital, but they won't admit him,” he said. Not long ago, he was helping a client to be admitted to a hospital; two official referrals from the local AIDS centre made no difference, and the woman was denied admission. Only after formal complaints filed by the patient’s family to the local government did the client get admitted. When asked about the most recent time a client was refused hospital admission, Mr Petrov answered “Yesterday,” without hesitation.
The stories shared by the Svetlana Izambayeva Charitable Foundation’s staff are consistent with the findings published in a recent Human Rights Watch report, which notes that people living with HIV regularly face stigma and discrimination from health-care workers. The situation is said to be worse outside of the major cities.
The course was initiated and organized by the National Union of Medical Students and was featured on a crowdfunding platform called No One Left Behind, a joint project of the Russian AIDS Center Foundation and UNAIDS.
Vera Brezhnevа, UNAIDS Goodwill Ambassador for Eastern Europe and Central Asia, has sponsored the course. “Every doctor must expect to see a person living with HIV at some point. We want medical students to understand that people living with HIV are a large and diverse group of people and their diagnosis is not a reason to hold negative attitudes towards them,” said Ms Brezhnevа. "I hope these first graduates of the Vera HIV Medical School will be the beginning of the end of HIV-related discrimination in health-care settings,” she added.
No One Left Behind
Region/country
Related
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025

Feature Story
Global HIV prevention targets at risk
29 October 2018
29 October 2018 29 October 2018As the world grapples with how to speed up reductions in new HIV infections, great optimism is coming from the world of HIV prevention research with a slate of efficacy trials across the prevention pipeline. Major HIV vaccine and antibody efficacy trials are under way, as is critical follow-on research for proven antiretroviral-based prevention options.
However, a new report by the Resource Tracking for HIV Prevention R&D Working Group shows that rather than bolstering the new research by increasing investments into these exciting new advances, resources for HIV prevention research and development are actually slowing down.
In fact, in 2017, HIV research funding declined for the fifth consecutive year, falling to its lowest level in more than a decade. In 2017, funding for HIV prevention research and development decreased by 3.5% (US$ 40 million) from the previous year, falling to US$ 1.1 billion.
“Make no mistake, we are in a prevention crisis and we cannot afford a further funding crisis,” said Mitchell Warren, AVAC Executive Director. “It is unacceptable that donor funding for HIV prevention research continues to fall year after year even as research is moving new options closer to reality. We need continued and sustained investment to keep HIV prevention research on track to provide the new tools that will move the world closer to ending AIDS as a public health threat.”
The report warns that meeting the UNAIDS HIV prevention Fast-Track target of less than 500 000 new infections by 2020 (new HIV infections were at 1.8 million in 2017) will not only require the expansion of existing options such as voluntary medical male circumcision and pre-exposure prophylaxis, but also the development of innovative new products, including long-acting antiretroviral-based prevention options and a vaccine.
Indeed, sustained funding will be critical to keep the full gamut of HIV prevention research moving forward in a timely manner, as even small declines in funding could delay or sideline promising new HIV prevention options that are needed to end the AIDS epidemic.
“With 5000 people becoming infected with HIV every day, it is critical that we both scale up the effective HIV prevention programmes we currently have and invest in new technologies and solutions so that they can become a reality for the populations most affected by HIV,” said Tim Martineau, UNAIDS Deputy Executive Director, a.i. “Doing both will avert new infections, save lives and reduce the rising costs of life-long antiretroviral treatment.”
The Government of the United States of America continues to be the major funder of HIV prevention research, contributing almost three quarters of overall funding in 2017. However, this was also a decrease of almost 6%, bringing funding from the United States to a five year low of US$ 830 million. The report highlights that the uncertainty around continued political will to fund the AIDS response is a serious concern.
This week, researchers, implementers, advocates and funders are gathering at the HIV Research for Prevention (HIVR4P 2018) conference in Madrid, Spain, to review progress in HIV prevention research. There is much to be optimistic about in HIV science and in the accumulated knowledge of how to end the epidemic; however, the sobering changes in the funding and policy environments are raising some serious concerns about the future of the response to HIV and the world’s ability to respond to the continued challenges that HIV presents.
The report and infographics on prevention research investment are online at www.hivresourcetracking.org and on social media with #HIVPxinvestment.
Since 2000, the Resource Tracking for HIV Prevention R&D Working Group (formerly the HIV Vaccines & Microbicides Resource Tracking Working Group) has employed a comprehensive methodology to track trends in research and development investments and expenditures for biomedical HIV prevention options. AVAC leads the secretariat of the working group, which also includes the International AIDS Vaccine Initiative and UNAIDS.






