Health and development

Feature Story
WHO World health report: The road to universal coverage
22 November 2010
22 November 2010 22 November 2010
If countries are to guarantee a good quality of life and ensure socio-economic development for people then promoting and protecting health is crucial. Without greater emphasis on health systems financing, however, this goal will remain unattainable for the poor, says the World Health Organization’s (WHO) World Health Report 2010, launched today.
Subtitled Health systems financing: the path to universal coverage, the report provides a detailed analysis of how this can be achieved with the provision of timely access to high-quality, affordable health services.
The concept of universal coverage emerged from a commitment from WHO member states in 2005 to develop their health financing systems. As the report has it, in an era of “globalisation of diseases” and increasing demands for chronic care from, for example people living with HIV on long term antiretroviral treatment, universal coverage will be of paramount importance.
According to the World Health Report, the lack of universal coverage has consequences for the poor. In some countries, for instance, the proportion of births attended by a skilled worker can be as low as 10%. This figure is close to 100% for richer nations.
Attaining universal coverage is considered relatively straightforward in principle but difficult in practice, and among others these two key actions are highlighted in the report.
Raising sufficient resources for health
Firstly, countries must raise sufficient funds. For many lower-income nations this may prove impossible in the short-term and the international community will need to financially support their efforts. Such nations currently spend around $US 32 per capita on health. To provide universal coverage this should be raised to US$ 60 by 2015.
Recipient countries can also increase their own health funding by reprioritising their budgets. Few African countries, for example, spend the 15% of their government budget on health they committed to in the 2001 Abuja Declaration. In fact, 20 countries in the region who signed the commitment actually allocate less now than they did nine years ago; although several, including Tanzania and Liberia, have exceeded this goal.
Another example is Rwanda’s donation of US$ 1 million in this year’s replenishment round of the Global Fund to fight AIDS, Tuberculosis and Malaria and South Africa’s announcement earlier this year of a US$ 1.1 million domestic investment in the country’s AIDS response.
Investing for health must be shared responsibility between development partners and national government
Michel Sidibé, UNAIDS Executive Director.
“Investing for health must be shared responsibility between development partners and national government,” said Mr Michel Sidibé, UNAIDS Executive Director.
Innovative financing may also be explored. Increasing taxes on air tickets, foreign exchange transactions and tobacco could be used to augment health budgets. The report states that, for example, a 50% increase in tobacco excise taxes would generate $US 1.42 billion in additional funds in 22 low income countries for which data are available. In countries such as the Lao People’s Democratic Republic, Madagascar and Viet Nam, the extra revenue would represent a 10% increase or more in total health expenditure, and a more than 25% in crease in the government’s total health budget.
Promoting efficiency and eliminating waste
Finally, the report suggests that inefficiency and waste can be extremely damaging for healthcare systems. It is argued that some 20-40% of resources spent on health are wasted. A 5% saving in health expenditure can be made if unnecessary spending on medicines is reduced, they are more appropriately used and quality control is improved.
Other ways to increase efficiency include; getting the most out of technologies and health services; motivating health workers; reducing medical errors and eliminating corruption.
Related

Feature Story
2010 Human Development Report: 40-year trends analysis shows many countries making gains but some losing ground
05 November 2010
05 November 2010 05 November 2010A version of this story first appeared at undp.org

Most developing countries made dramatic yet often underestimated progress in health, education and basic living standards in recent decades, with many of the least developed countries posting the greatest gains. This is one of the key findings revealed in the United Nations Development Programme (UNDP) 2010 Human Development Report, released 4 November.
However, despite significant progress in some countries, patterns of achievement vary greatly, with some nations losing ground since 1970, the report shows. The 20th anniversary edition, which introduces three new indices for inequality, gender and poverty, documents wide inequalities within and among countries and deep disparities between women and men on a broad range of development indicators. It highlights the prevalence of extreme multidimensional poverty in South Asia and sub-Saharan Africa and the AIDS epidemic is also shown to have had a marked negative impact on progress in some countries.
The Human Development Reports have changed the way we see the world
UN Secretary General Ban Ki-moon
The report, called The Real Wealth of Nations: Pathways to Human Development, was launched by UN Secretary-General Ban Ki-moon, UNDP Administrator Helen Clark and Nobel laureate Amartya Sen who helped devise the HDI for the first Human Development Report in 1990 with the late economist Mahbub ul Haq, the series founder.
“The Human Development Reports have changed the way we see the world,” Ban Ki-moon said. “We have learned that while economic growth is very important, what ultimately matters is using national income to give all people a chance at a longer, healthier and more productive life.”
According to Helen Clark, “The report shows that people today are healthier, wealthier and better educated than before. While not all trends are positive, there is much that countries can do to improve people’s lives, even in adverse conditions. This requires courageous local leadership as well as the continuing commitment of the international community.”
The report shows that people today are healthier, wealthier and better educated than before.
Helen Clark, DP Administrator
Overall, as shown in the report’s analysis of all countries for which complete HDI data are available for the past 40 decades, life expectancy climbed from 59 years in 1970 to 70 in 2010, school enrolment rose from just 55 percent to 70 percent, and per capita GDP doubled to more than US$ 10,000. Several poorer countries have registered substantial gains in education and public health, including Benin, Cambodia and Ethiopia, which ranked 11th in progress over time.
The region with the fastest HDI progress since 1970 was East Asia, led by China and Indonesia. A number of countries in sub-Saharan Africa and the former Soviet Union lagged behind, however.
“We see great advances, but changes over the past few decades have by no means been wholly positive,” the authors write. “Some countries have suffered serious setbacks, particularly in health, sometimes erasing in a few years the gains accumulated over several decades... And the gaps in human development across the world, while narrowing, remain huge.”
Related
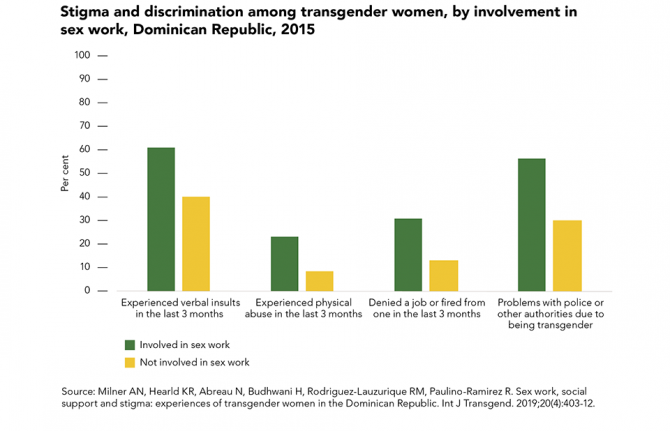
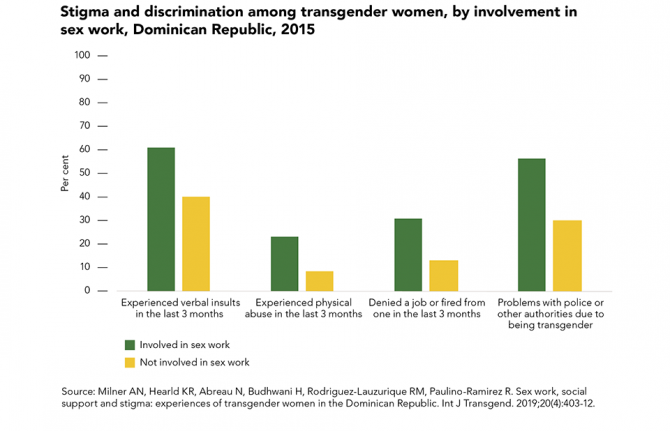 Transgender sex workers face frequent abuse
Transgender sex workers face frequent abuse
29 March 2022
 Many key populations avoid health services
Many key populations avoid health services

21 February 2022

Feature Story
Rethinking linkages between the MDGs: Botswana leads the way
21 September 2010
21 September 2010 21 September 2010
UNAIDS Executive Director Mr Michel Sidibé, 21 September, 2010. Credit: UNAIDS/Hamilton
There is now global recognition that one Millennium Development Goal cannot be achieved without the others. The health sector, in particular, has realized that responses to Millennium Development Goals 4, 5 and 6—to reduce child mortality, improve maternal health, and combat HIV malaria and other diseases—must be tackled together to improve people’s life.
At a side event of the UN Millennium Development Goals Review Summit taking place from 20 to 22 September in New York, Botswana shared its experiences in integrating health interventions and programmes in order to maximize resources and improve health outcomes.
Botswana, a country with an HIV prevalence of 23.9% in its adult population, has recently made progress in curbing the epidemic. Data shows that HIV prevalence among young people aged 15-24 years has been declining consistently since 2001. The country has also managed to tackle child mortality through expanded feeding programs for children under five together with near universal coverage of services to prevent mother-to-child transmission of HIV.
At the event, entitled “Toward an Integrated approach to Attaining Health Related Millennium Development Goals,” Mr Mompati S. Merafhe Vice President of Botswana, presented the country’s case to show what integrating health services means in practice.
According to Vice President Merafhe, Botswana was able to mount a credible response to AIDS, and strengthen health systems through an integrated approach. He stressed the importance of partnerships, including that of the United Nations.
“We have crated an enabling environment and we have closed gaps that take us on the road to reach the MDGs by 2015,” said Vice President Merafhe. “This has resulted in our success in preventing mother-to-child transmission of HIV.”
Research shows that countries with the highest incidence of HIV often have a high unmet need for family planning. Offering HIV services and contraceptives at the same facility, or even by the same health care worker, increases the opportunity to access services.

Mr Mompati S. Merafhe Vice President of Botswana, 21 September, 2010. Credit: UNAIDS/Hamilton
According to the panellist, the benefits of integrating services are many: combining interventions at point-of-care, as well as sharing a supply chain, and information systems are all examples of how resources can maximized. Importantly, they stressed the process also decreases out-of-pocket costs for the individual, through reducing the number of visits to health centres, thus minimizing travel time and cost, as well as fees associated with accessing services.
“As has been shown by Botswana’s leadership, the AIDS response can be the bridge that connects movements,” said Michel Sidibé, UNAIDS Executive Director. “Programmes advancing maternal and child health, sexual and reproductive health, gender equality, sexual violence all contribute to achieving the MDGs.”
To assess the way forward the session included a range of topics on health service integration. Mr Erik Solheim, Minister of Environment and International Development of Norway gave the donors perspective. UNAIDS, UNICEF and UNFPA discussed the benefits of integration from the bilateral outlook. The Elizabeth Glaser Paediatric AIDS Foundation (EGPAF) gave further insights from the implanting organizations point-of-view.
While there are many benefits of integrating health services, integration is not a “one-size-fits-all” strategy, according to the participants. For example, countries with a weak health system, integrating services may overburden an already stretched system. The process of planning and implementing integrated services also poses a number of technical challenges for governments, policy donors, program implementers, and health care workers.

Feature Story
Maternal deaths worldwide drop by a third
15 September 2010
15 September 2010 15 September 2010
The number of women dying due to complications during pregnancy and childbirth has decreased by 34% from an estimated 546 000 in 1990 to 358 000 in 2008, according to a new report, Trends in maternal mortality, released by the World Health Organization (WHO), the United Nations Children's Fund (UNICEF), the United Nations Population Fund (UNFPA) and the World Bank.
Despite this notable progress, the annual rate of decline is less than half of what is needed to achieve the Millennium Development Goal (MDG) target of reducing the maternal mortality ratio (the number of deaths per 100,000 live births) by 75% between 1990 and 2015. This will require an annual decline of 5.5%: the current average annual decline of just 2.3%.
"The global reduction in maternal death rates is encouraging news," says Dr Margaret Chan, the Director-General of WHO.”No woman should die due to inadequate access to family planning and to pregnancy and delivery care."
For nations with high HIV prevalence, AIDS has become a leading cause of death during pregnancy and after the birth. There is also some evidence that women living with HIV are at greater risk of maternal death. Overall, it was estimated that there were 42 000 deaths due to AIDS among pregnant women globally in 2008. About half of those are estimated to be maternal. The contribution of HIV was highest in sub-Saharan Africa where 9% of all maternal deaths were AIDS-related.
“Integrating HIV services with maternal and sexual and reproductive health services is imperative to stop mothers from dying and babies from being born with HIV,” said Mr Michel Sidibé, UNAIDS Executive Director. “The AIDS movement must be leveraged to achieve reductions in maternal and child mortality.
According to the report pregnant women die from four major causes: severe bleeding after childbirth, infections, hypertensive disorders, and unsafe abortion. Every day, about 1000 women died due to these complications in 2008, more than half in sub-Saharan Africa. The risk of a woman in a low-income country dying from a pregnancy- related cause during her lifetime is about 35 times greater than a woman living in a high-income country.
"To achieve our global goal of improving maternal health and to save women's lives we need to do more to reach those who are most at risk," says Anthony Lake, Executive Director of UNICEF. "That means reaching women in rural areas and poorer households, women from ethnic minorities and indigenous groups, and women living with HIV and in conflict zones."
The new estimates show that it is possible to prevent many more women dying. Countries need to invest in their health systems and in the quality of care.
"Every birth should be safe and every pregnancy wanted,” says Thoraya Ahmed Obaid, the Executive Director of UNFPA.The lack of maternal health care violates women's rights to life, health, equality, and non-discrimination.
UN agencies, donors and other partners have increasingly coordinated their assistance to countries, focusing on those with the greatest burden.
According to Tamar Manuelyan Atinc, Vice President for Human Development at the World Bank, “Given the weak state of health systems in many countries, we must work closely with governments, aid donors and agencies, and other partners to strengthen these systems.

Feature Story
National ownership pivotal to sustained HIV responses
02 July 2010
02 July 2010 02 July 2010 Family in Djibouti. Credit: UNAIDS/P. Virot
Family in Djibouti. Credit: UNAIDS/P. VirotNational ownership is central to sustainable AIDS responses and is beyond doubt a path to improved aid effectiveness. To set the stage for engaged debates on national ownership and actions to realize this, UNAIDS organized a consultation in Geneva on 21 June 2010 that brought together government representatives, civil society, representatives from regional political bodies, and development partners.
The dialogue resulted in a clear definition of national ownership which is:
“Inclusive multi-sectoral national leadership at all levels in managing the design of effective AIDS policy and strategy, its implementation, monitoring, reporting and sustainable resourcing as part of the national development agenda, and for assuring board result-based mutual accountability mechanisms and national capacities to strengthen the AIDS response”.
Participants also established indicators to measure progress. These indicators cover multi-sectoral AIDS coordination; non-discriminatory laws and regulations; inclusive process in the development of Strategy, work plan, operational plan and review; monitoring and evaluation and mutual accountability system; integration of HIV in national development plans and capacity development plans; sustainable HIV financing; mutual financial accountability mechanisms; alignment and harmonization; and capacity building.
Addressing the forum, Mr Michel Sidibé, executive director of UNAIDS, highlighted the need for countries and donors to move from short-term aid commitments to longer term financing that is both predictable and sustainable. According to Mr Sidibé key to achieving this is “understanding the interaction of ownership and external funding” which can happen by focusing on the ways that significant donors actually enable national ownership and empower country partners.
The US Global AIDS Coordinator Ambassador Eric Goosby stressed the importance of “mutual accountability.” He pointed out the imperative that donors “carry out their development work in such a way that engagements with country partners and priorities are mutually beneficial.”
The participants discussed strategic incentives to foster greater country partner ownership of national AIDS policies and programmes and to encourage production and use of evidence. In addition, how national ownership can be enhanced by mobilizing greater domestic resources and investments, and the roles and action that country partners and development partners can employ together to strengthen ownership.
Renewed approach to technical assistance and capacity building
Better and more sustainable articulation of countries’ needs, mentoring countries with counterparts from the North, coupled with the aggressive development of TA in the South and South-South cooperation would result in a renewed approach to technical assistance (TA). This could ensure that it is driven by demand rather than by supply. To strengthen national ownership, the inclusion of capacity building support as an integral part of joint operational planning would strengthen country’s responses. Zambia’s Minister of Health, H.E. Kapembwa Simbao, pointed out that “national ownership refers to the availability of in-country expertise to monitor their programmes.”
UNAIDS Secretariat, in collaboration with all stakeholders, will continue to foster national ownership so that countries can make evidence-informed decisions and invest funds where they are most needed in order to achieve better outcomes for the AIDS response as well as the countries’ wider health and development goals. UNAIDS also plans to continue to support country and regional consultations that include all constituents.
Right Hand Content
Feature stories:
Kenya’s experience informs new resource for increasing coordination on AIDS (21 November 2008)
Related
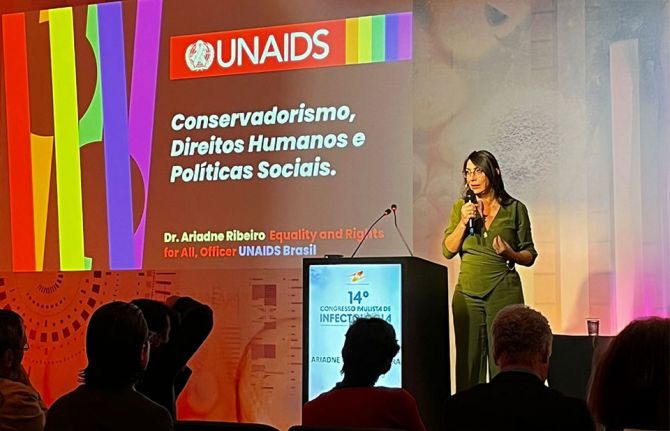 Upholding dignity for everyone: Ariadne Ribeiro Ferreira
Upholding dignity for everyone: Ariadne Ribeiro Ferreira
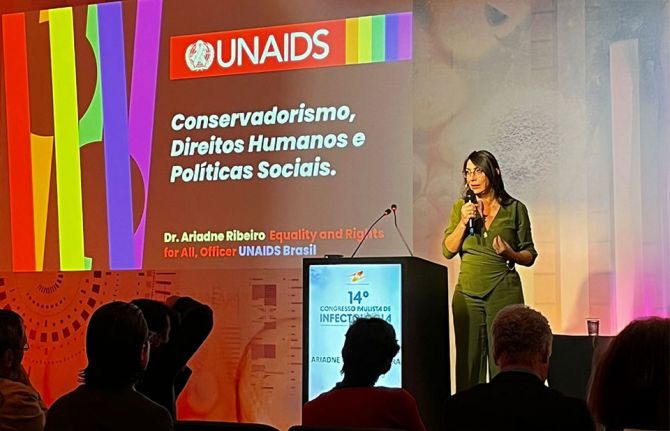
21 November 2024

Feature Story
Women Deliver conference focuses on MDG 5
08 June 2010
08 June 2010 08 June 2010 L to R: United Nations Secretary-General Ban Ki-moon, UNAIDS Goodwill Ambassador, Annie Lennox and UNAIDS Executive Director, Michel Sidibé. 07 June 2010. Credit: UNAIDS/S.Johnson
L to R: United Nations Secretary-General Ban Ki-moon, UNAIDS Goodwill Ambassador, Annie Lennox and UNAIDS Executive Director, Michel Sidibé. 07 June 2010. Credit: UNAIDS/S.JohnsonWith maternal and reproductive health as a global priority, a three-day conference, Women Deliver 2010, has kicked off in Washington DC under the theme "Invest in women. It pays." The event’s main focus is to highlight that the Millennium Development Goals (MDG) will not be achieved without investing in women and that there is just enough time, if the world commits funding now, to achieve the MDG’s fifth goal of improving maternal health.
UNAIDS Executive Director Michel Sidibé and newly appointed UNAIDS Goodwill Ambassador Annie Lennox gave the welcome address and opening plenary on the first day of the conference.
“If we integrate HIV into maternal health programmes, we can make huge progress on almost every global development goal. We can stop mothers from dying of HIV and dramatically reduce maternal mortality. Let’s join together,” said Mr Sidibé.
Ms Lennox, who spoke on the topic Women Need a World that Delivers added, "I believe that the AIDS response is an excellent entry-point to better invest in women and girls at all levels, and to advance women's sexual and reproductive rights. We need to empower women and girls so that they can better protect themselves and take control of their own sexual and reproductive health."
I believe that the AIDS response is an excellent entry-point to better invest in women and girls at all levels, and to advance women's sexual and reproductive rights
Annie Lennox, UNAIDS Goodwill Ambassador
About 16 million women over the age of 15 are living with HIV worldwide and in sub-Saharan Africa, women make up almost two-thirds of people living with HIV. In many parts of the world, women have a higher risk of HIV than men.
In cultures where gender inequality persists, women are likely to face barriers in accessing HIV, maternal and reproductive health services due to limited decision-making power, lack of control over financial resources, restricted mobility and child-care responsibilities.
A recent study published in the medical journal The Lancet projects that globally HIV has increased maternal mortality by 20%. While maternal mortality has been on the decline globally, it has been on the rise in many sub-Saharan Africa countries, because of HIV. In South Africa, it is estimated that more than 50% of all maternal deaths can be attributed to HIV.
Considerable progress, however, has been made on the treatment front. Over the years, more women have been able to access HIV treatment services. This is primarily due to the fact that more women are accessing antenatal services to prevent HIV transmission to their infants, and more women are coming forward for HIV counselling and testing.
 Former President of Chile Michelle Bachelet (left) meets with UNAIDS Executive Director Michel Sidibé during Women Deliver 2010 conference in Washington D.C. Credit: Sylvia Johnson
Former President of Chile Michelle Bachelet (left) meets with UNAIDS Executive Director Michel Sidibé during Women Deliver 2010 conference in Washington D.C. Credit: Sylvia JohnsonWith over 2,000 participants from 115 countries, including 100 government officials from more than 30 countries, the conference was also the platform to announce the initiation of the first trial among women in Africa testing a vaginal ring containing an antiretroviral drug that could one day be used to prevent HIV transmission during sex.
The technology, if successfully tested, would give women around the world a tool to protect themselves from HIV infection. The trial has been initiated by non-profit International Partnership for Microbicides (IPM).
Speaking on the trial, Mr Sidibe said, "Preventing HIV transmission is essential if we are to win the battle in the long-term and protect the health and safety of future generations. If successful, innovations, like microbicides, could have an extraordinary impact.”
The conference, which ends on 9 June 2010, includes over 300 speakers in 118 separate sessions over three days. Topics included “Modern Contraception Comes of Age”, “Strategies to Address Sexually Transmitted Infections” and “Girls Speak: Exploring the Girl Effect”.
Right Hand Content
Key populations:
Feature stories:
Celebrated artist and activist Annie Lennox appointed as International UNAIDS Goodwill Ambassador (02 June 2010)
Linking maternal and child health to AIDS ahead of G8 Summit (01 June 2010)
New study shows significant drop in maternal deaths (14 April 2010)
WHO report on the health of women: AIDS leading cause of death globally in women of reproductive age (09 November 2009)
External links:
Publications:
Joint Action for Results: UNAIDS Outcome Framework (2009–2011) (pdf, 930 Kb.)
Making HIV trials work for women and adolescent girls (pdf, 143 Kb.)

Feature Story
World Health Assembly to discuss International Health Regulations and MDG
17 May 2010
17 May 2010 17 May 2010
Credit: WHO/Jesse Hoffmann
The 63rd World Health Assembly, the gathering of the decision-making body of World Health Organization (WHO), opened in Geneva today. Health Ministers and officials from across the world will meet until 21 May 2010 to discuss the implementation of the International Health Regulations (IHR).
There are 194 countries across the globe, including all the member states of the World Health Organization (WHO) who are State Parties to the IHR, a binding, international legal instrument. The aim of these global rules is to help the international community prevent and respond to acute public health risks that have the potential to cross borders and threaten people worldwide.
The IHR, for example, require countries to report certain disease outbreaks and public health events to WHO and also to strengthen their existing capacities for public health surveillance and response.
This year’s World Health Assembly will also focus on monitoring the achievements of the health-related Millennium Development Goals. In the year 2000, 189 countries committed their nations to a new global partnership to reduce extreme poverty. They set out a series of targets to be reached by 2015. These have become known as the Millennium Development Goals (MDGs) and include halving extreme poverty, halting the spread of HIV and providing universal primary education.
The World Health Assembly is attended by delegations from all WHO member states yearly to focus on specific health agenda. Last year’s Assembly focused considerable attention on the widespread outbreak of influenza A (H1N1) and the most effective responses to the potential pandemic, including preparedness, access to vaccines and sharing of influenza viruses.
World Health Assembly to discuss International He
Cosponsors:
World Health Organization (WHO)
Feature stories:
UNAIDS calls for a virtual elimination of mother to child transmission of HIV by 2015 (21 May 2009)
Sixty-second World Health Assembly to be dominated by A(H1N1) (18 May 2009)
Publications:
Joint action for results: UNAIDS outcome framework, 2009 – 2011 (pdf, 931 Kb.)

Feature Story
Call for submissions Global Health Governance: Special Issue on “Governance and the AIDS Response”
01 March 2010
01 March 2010 01 March 2010
Global health Governance: The Scholarly Journal for the New Health Security Paradigm
The next issue of Global Health Governance will focus on Global Health Governance and the AIDS Response. Michel Sidibé, Executive Director of the United Nations Joint Programme on HIV/AIDS (UNAIDS) and Kent Buse, Senior Policy Advisor to the Executive Director, will serve as guest editors for this issue.
This special issue will explore the contributions of the global AIDS response over the last 30 years to innovations in governance principles, paradigms, and practice. It will outline present challenges, opportunities and future directions for improving both the global governance of the AIDS response and governance approaches to human development, security and dignity more generally. AIDS governance at global, national and community levels has not only transformed the nature of health systems governance, but also shed light on a number of socio-political issues with significant implications for human development. The editors seek a balance of theoretical/conceptual and empirical pieces from a wide variety of disciplinary perspectives including public health, political science and international relations, international law, philosophy, history, anthropology, business and public administration to better understand and improve this exciting area of practice and enquiry.
The focus of manuscripts must be on the governance of the AIDS response and/or lessons it offers for Global Health Governance. The range of possible article topics is vast and may include, but is not limited to, the following:
- Enhancing effectiveness and legitimacy of global governance mechanisms and institutions;
- Systems for inclusive policy-making as well as the engagement of civil society and the private sector in planning, accountability, oversight of national responses;
- Innovations, successes, failures and potential of transparency/accountability mechanisms—including within the multilateral system;
- Process of establishing/validating/disseminating/enforcing novel global norms—particularly concerning sexual and human rights, punitive laws, inclusive policy making, accountability, ethical trials, access; gender;
- Country institutions for governing national responses, such as NACs and CCMs;
- Tensions between concepts of national ownership and global cosmopolitan citizenship and social justice;
- Cross-border civil society interest group formation for policy change and supranational citizenship building;
- Politics of punitive laws—and the role of civil action, networks, partnerships in their repeal;
- Framing and discourse in relation to global priority setting;
- Innovations in communication technologies for global governance;
- AIDS in the context of global and national security as well as global solidarity and justice;
- Lessons from the AIDS response for realizing the right to health through development of novel norms and enforcement processes concerning universal access;
- Role of AIDS activists/networks in development of intellectual property rights discourse/regimes and practice and implications for access to essential health commodities;
- The politics of innovative financing and resource allocation;
- Governance implications of taking the AIDS response out of relative isolation and linking to other efforts to achieve the MDGs;
- Lessons from AIDS partnerships: governance, ethics, politics, public-private interplay.
In addition to academic papers, the Guest Editors will solicit commentaries from thought leaders on topical issues and future directions of global health governance.
Authors should alert the journal of their intention to submit a manuscript, including the proposed title of the paper, the names of the author(s) and an abstract of no more than 250 words no later than 15 March 2010. The abstract should include the research question(s), methods, findings, main argument and implications. The letter should be submitted to Sonja Tanaka, tanakas@unaids.org. The deadline for submissions is 15 June 2010. The provisional date of publication is October 2010.
Timeline
- February 15th—Call for Proposals
- March 15th—Deadline for submissions of Abstracts
- June 15th—Deadline for submission of Manuscripts
- August 10th—Accept/Reject decisions communicated to authors
- September 10th—Deadline for submission of revised Manuscripts
- October—Provisional publication of 2010 Fall issue
There are no submission fees.
More information about the Journal can be found at the Journal web site.
Call for submissions Global Health Governance: Sp

Feature Story
As global economy slows International Health Partners push for faster health progress
12 February 2010
12 February 2010 12 February 2010
Executive Director of UNAIDS Michel Sidibé addressed the Ministerial Review Meeting of the IHP+ which took place in Geneva 4-5 February 2009.
Credit: World Health Organization
Meeting in Geneva last week, participants in the first Ministerial Review Meeting of the International Health Partnership and related initiatives (IHP+) adopted a document laying out bold and concrete commitments to push forward the objectives of the Partnership.
The official communiqué notes that the current severe global economic downturn will put pressure on the development budgets of donor countries and make it difficult for developing countries to sustain domestic funding for health.
“We agreed that this increases the importance of our objectives to secure more effective and predictable financing, as well as additional resources to achieve the health MDGs.”
"We reaffirmed our commitment to maintaining levels of development aid and domestic health budgets. We also commit to delivering predictable financing, and ensuring the effective use of all domestic and external resources. This is critical to achieving results and attracting additional resources."
I see the Partnership as an important instrument to help achieve universal access and to stand by those in need of HIV services
UNAIDS Executive director Michel Sidibé
Addressing the meeting, the executive director of UNAIDS Michel Sidibé pledged UNAIDS’ full support to the IHP+ process. “I see the Partnership as an important instrument to help achieve universal access and to stand by those in need of HIV services,” said Mr Sidibé.
The Review Meeting of the IHP+ took place 4-5 February 2009 to take stock of progress, review lessons, and examine ways to maintain commitment and momentum.
The IHP+ is a partnership which includes partner countries, United Nations agencies including UNAIDS, bilateral donors, civil society and private sector partners. Launched in September 2007, the partners aim to increase coordination in health and to strengthen health system in order to make progress on achieving the health-related Millennium Development Goals.
Right Hand Content
Feature stories:
International Health Partnership launches new web site (07 May 2008)
International Health Partnership launch (05 September 2007)
External links:
International Health Partnership
Publications:
IHP+ Ministerial Review Communiqué (pdf, 108 kb)

Feature Story
UNAIDS and Economic Commission for Africa discuss innovative financing for health in Africa
09 November 2009
09 November 2009 09 November 2009 (from right) Executive Secretary of the UN Economic Commission for Africa Mr Abdoulei Janneh and Executive Director of UNAIDS Michel Sidibé, 9 November 2009.
(from right) Executive Secretary of the UN Economic Commission for Africa Mr Abdoulei Janneh and Executive Director of UNAIDS Michel Sidibé, 9 November 2009. Credit: UNAIDS
The Executive Director of UNAIDS Michel Sidibé met with the Executive Secretary of the Economic Commission for Africa (ECA) Mr Abdoulei Janneh earlier today in Addis Ababa, Ethiopia.
They held broad-ranging discussions on the relationship between health and development and the need to find innovative ways to generate financial resources to fund future HIV treatment for people in need. The importance of resource monitoring and evaluation of results for the Millennium Development Goals was also underlined.
Mr Abdoulei Janneh also updated Mr Sidibé on the Coalition for Dialogue in Africa (CoDA) which was launched earlier this year as a joint venture between the African Development Bank and the ECA to stimulate discussions on African socioeconomic issues and explore new ways for Africa development.

(from left) Executive Director of UNAIDS Michel Sidibé and the Executive Secretary of the UN Economic Commission for Africa Mr Abdoulei Janneh held discussions on health financing, 9 November 2009.
Credit: UNAIDS
The CoDA initial advisory board includes Dr Frene Ginwala, Former Speaker of the National Assembly of South Africa; Mr Mo Ibrahim, Chair, Mo Ibrahim Foundation; Dr. Spciosa Wandira Kazibwe, former Vice President of the Republic of Uganda; and The Right Honourable, Mr. Paul Martin, former Prime Minister of Canada.
While in Addis this week Mr Sidibé is attending the board meeting of the Global fund to Fight AIDS, TB and Malaria.