Community mobilization


Feature Story
UNAIDS supporting people stranded in Egypt to access HIV treatment
29 June 2020
29 June 2020 29 June 2020Hundreds of thousands of people around the world have been stranded abroad due to the bans on flights and border closures imposed to stop COVID-19. As elsewhere, thousands of non-nationals have been stranded in Egypt indefinitely.
Travel restrictions have had many repercussions on the daily lives of non-nationals, putting significant economic pressure on them and potentially putting their well-being at risk.
The UNAIDS Country Office for Egypt has been working on COVID-19 from the start of the pandemic in the country, establishing a direct line of communication with the National AIDS Program and working with it to ensure the continuation of HIV treatment by everyone on it and to help non-nationals in Egypt to get supplies of antiretroviral therapy.
Sophia Bianchi (not her real name) is an Italian tourist stranded in Sharm El Sheikh. “I ordered my antiretroviral treatment in late April from Italy via a courier service. Unfortunately, the shipment was stuck at the airport customs in Cairo for weeks. I contacted UNAIDS and they have been very helpful, following up daily with the Egyptian Ministry of Health and Population to get approval for releasing the shipment and checking on me and my health. They kept pushing through the Eid holidays and it all got resolved in two weeks. It was a stressful time but now I am relieved,” she said.
Antiretroviral therapy is available in Egypt free of charge to all nationals and registered refugees. However, as there is no community-based dispensing, nor private market purchase of antiretroviral medicines, gaps remain in ensuring that non-nationals can access treatment. For this reason, UNAIDS’ work during the COVID-19 pandemic has been essential in bridging the gaps.
There are strict rules on the dispensing of antiretroviral therapy in Egypt—only close family members are able to collect it from the dispensing centre. For Fatima Ahmed (not her real name), a refugee from Yemen who because of chronic illnesses that put her at higher risk from COVID-19 cannot leave her house, this was a significant barrier to accessing her HIV treatment. UNAIDS got in contact with the Egyptian Ministry of Health and Population to get an exceptional approval to dispense her medicine through a nongovernmental organization.
“I have not left the house for more than three months. My family has not been able to support me financially, so I was left without revenue. Thanks to the support of the National AIDS Program and MENA Rosa, a nongovernmental organization, peer supporters have delivered three months of antiretroviral treatment to my doorstep,” said Ms Ahmed.
However, much still remains to be done in reaching out to the most in need in Egypt. UNAIDS in Egypt has been advocating for the right to health and universal health coverage for everyone and is working in partnership with the Egyptian Ministry of Health and Population to ensure treatment for all nationals and non-nationals in the country.
“We believe in the absolute right of everyone to have access to their basic right to health. Ensuring access to antiretroviral therapy during these exceptional times is therefore our upmost priority. We are working relentlessly with our governmental and nongovernmental partners to build long-term policies to ensure treatment and care services for people living with HIV during times of emergency,” said Walid Kamal, the UNAIDS Country Director for Egypt.
Our work
Region/country
Related




Feature Story
Local skills and knowledge help Senegalese community-led organizations deliver
18 June 2020
18 June 2020 18 June 2020Face masks, sanitizers and soap. Food packages and money to pay the rent. Information about how to protect yourself and your loved ones from the virus—the list goes on.
The necessities of life during the COVID-19 pandemic can be hard to come by, but communities are organizing and delivering services and much needed commodities to the people that need them the most. And communities with experience of responding to other epidemics are turning their lessons learned to COVID-19.
“Organizations led by and for people living with HIV and key populations are now spearheading urgently needed programmes to combat COVID-19 and secure the health and well-being of their communities,” said Demba Kone, the UNAIDS Country Director for Senegal.
Like in many other countries around the world, face masks and other personal protective equipment are in short supply in Senegal. However, the Enda Santé nongovernmental organization had a quick and efficient solution—the many local tailors and dressmakers, who are highly skilled and had a ready access to supplies of fabric. Responding to the call of “come work with us”, the tailors and dressmakers produced thousands of high-quality masks in a record time, and at a very low cost. And the local production meant that the money stayed in the local economy, which had been badly affected by the pandemic.
Enda Santé has also begun negotiating with donors that fund HIV programmes. Funds that had been allocated to HIV-related activities that could not be carried out in the current context have been re-allocated to support COVID-19-related activities in the most-affected communities.
Focusing the right resources at the right place is crucial when responding to outbreaks that are travelling fast through communities. Enda Santé therefore went to work to identify the communities that were the most vulnerable and in the greatest need.
Drawing on statistics generated by the government, as well as their own knowledge about the demography and availability and accessibility of health services, Enda Santé looked at poverty levels among communities, the neighbourhoods where overcrowding was the worst and where people had difficulty in accessing health care. It was clear that the people who were the most vulnerable to HIV were also now very vulnerable to COVID-19.
Enda Santé focused on those communities, distributing prevention materials and mobilizing young and female leaders from the community, training them to go door to door explaining how people could protect themselves, how to identify cases and how to get people into treatment centres.
It was obvious that many of the people affected by HIV that Enda Santé worked closely with—people living with HIV, sex workers, people who inject drugs and young women and adolescent girls—had lost their incomes because of the lockdown and were now struggling with the triple impact of HIV, COVID-19 and poverty. In response, Enda Santé organized the delivery of food and cash transfers.
Daouda Diouf, the Executive Director of Enda Santé, reflected on the process. “We had already learned how to do all of this work in the context of HIV, so we were transferring the skills we learned in responding to HIV for 25 years, and we moved to apply them to COVID-19. The speed of action, engaging community members and putting them at the centre of the work, the door-to-door approach, pre-empting the risk of transmission, delivering prevention packages, and so on. We were able to act very quickly.”
Our work
Region/country


Feature Story
Remembering human rights activist Yves Yomb
17 June 2020
17 June 2020 17 June 2020Yves Yomb, a human rights activist from Cameroon, died on 15 June 2020.
His journey to becoming an activist began in his home country, in 2006. At the height of a media campaign targeting gay men and other men who have sex with men, Mr Yomb was a founding member of Alternative Cameroun, one of the first human rights organizations in western and central Africa to advocate for tolerance and social inclusion. “We told ourselves that if we didn’t act, no one would,” he once said.
For more than a decade, Mr Yomb was at the forefront of the fight for the rights of sexual minorities and human rights in Africa, and wherever else the struggle took him. Ahead of the 2018 International AIDS Conference, he spoke at the launch of UNAIDS’ global report in Paris, France, calmly and with determination, recalling that the response to HIV is an uncompromising struggle for human rights and international solidarity.
Mr Yomb was the spokesperson of Africagay against AIDS, the first network dedicated to promoting access to rights and support for lesbian, gay, bisexual and transgender people in francophone Africa, which in 2019 became the Global Alliance of Communities for Health and Rights (GACS PLUS), a member of Coalition Plus. Always at the forefront of the fight, he called on UNAIDS to renew its support for civil society, an initiative that led to the birth of the Civil Society Institute for West and Central Africa.
“Without rights, the people most affected by the AIDS epidemic cannot have access to health services. This is what feeds the hidden epidemic we are fighting against. This is what fuels the hidden epidemic we are fighting,” he said.
"Yves Yomb was a great voice and argued in a way that left no one indifferent. I remember him speaking in 2018 in the Kofi A. Annan Conference Room at UNAIDS headquarters in Geneva, Switzerland, surrounded by senior management, representatives of UNAIDS Cosponsors and others. With the same tenacity he displayed at home in Cameroon, he advocated for the respect of human rights. He argued tirelessly for increased support for civil society in all its diversity. Rest in peace, brother. We will continue the common fight,” said Helene Badini, UNAIDS Senior Regional Community Support Adviser.
Region/country


Feature Story
New HIV community group in Guinea fighting COVID-19
12 June 2020
12 June 2020 12 June 2020Communities have always played an important role in the fight against epidemics in Africa. In the response to HIV, community involvement has been illustrated by a key principle: nothing for us without us. Since the beginning of the AIDS response, civil society has been on the front line, demanding access to treatment, calling for respect for human rights and supporting community-led HIV services.
In Guinea, community engagement has resulted in the continuous improvement of HIV programmes and to considerable progress in testing, prevention, treatment adherence and psychosocial support. The promotion and defence of human rights is also central to communities, and community engagement has contributed to tackling stigma and discrimination and to monitoring the quality of services and addressing challenges.
From the lessons learned from the 2013–2016 Ebola outbreak in the country, the need for the active participation of communities, alongside the public, in the COVID-19 response is clear. This is why the National Platform of Civil Society Organizations on HIV and TB (PNOSC-HIV/TB) was recently set up. Established with technical and financial support from UNAIDS and bringing together 28 associations, PNOSC-HIV/TB played a central role in the development of the Ministry of Health’s contingency plan to reduce the impact of COVID-19 on health services, particularly HIV services.
Focusing on populations that include prisoners, people in refugee camps and solidarity cities— places where people with disabilities live—PNOSC-HIV/TB is active in helping to prevent COVID-19, raising awareness about the importance of physical distancing through community mediators, local artists, the media and door-to-door outreach.
Psychosocial help is being given through a hotline run by two networks of people living with HIV, one of which is focusing on key populations. PNOSC-HIV/TB is also working to promote and scale up nationwide the multimonth dispensing strategy for antiretroviral therapy.
“PNOSC-HIV/TB will enable us to speak with one voice, to assert ourselves even more, to organize and strengthen our contribution to defeating COVID-19 and to the elimination of AIDS in Guinea by 2030,” said Mahawa Diallo Sylla, President of PNOSC-HIV/TB.
PNOSC-HIV/TB also participates in the Community Treatment Observatory, which monitors respect for human rights in the context of COVID-19 and reports violations to the government and the National Institute of Human Rights.
“I am impressed by PNOSC-HIV/TB’s willingness to close the gap in terms of their participation in the national response to HIV. I am confident that the momentum and energy generated since its establishment will have a lasting impact on the responses to HIV and COVID-19 in Guinea,” said Dado Sy Kagnassy, UNAIDS Country Director for Guinea.
Our work
Region/country




Feature Story
UNAIDS and civil society helping stranded people living with HIV
22 May 2020
22 May 2020 22 May 2020A day before Deepak Sing (not his real name) planned to return to India, all international travel ground to a halt—he was stuck in Luanda.
Because of his frequent travel, he had extra HIV medicine, but his supplies started to run low.
“I visited more than 10 pharmacies and explored options of delivery of antiretroviral medicines from India to Angola, but without success,” he said.
He decided that reaching out to Indian colleagues would be his best bet.
“I contacted the Humsafar Trust in Mumbai, and they in turn contacted the UNAIDS India office,” he explained.
Bilali Camara, the UNAIDS Country Director for India, immediately followed up with his peer in Angola. The UNAIDS Country Director for Angola, Michel Kouakou, guided Mr Sing towards the national AIDS institute, which organized a conference call with a medical doctor because one of the medicines that Mr Sing took is not yet in use in Angola. The doctor proposed a substitute and in less than 24 hours he picked up his medication. “Due to the change of one medicine, Mr Sing received only a one-month supply, which will be renewed at his discretion,” explained Mr Kouakou, who has helped two other stranded foreigners in the past month.
“I now believe that humanity exists!" Mr Sing said with great relief.
Since the COVID-19 pandemic hit, UNAIDS has helped stranded people to obtain HIV medicine in countries as diverse as Canada, China, Latvia, Myanmar and Ukraine. Mr Camara said that UNAIDS set up a system so that 700 people from India who were living in Myanmar could access their medicine, since they could no longer access it in India because of the COVID-19 lockdown.
Jacek Tyszko, Senior Programme Adviser at UNAIDS’ Geneva headquarters, has never seen anything like this. So far, he has helped 100 people, mostly in eastern Europe, because of his experience in the region.
“Either I connect people to the local AIDS authority or ideally we link them up to civil society, because they usually have readily available treatment,” he explained. Because of demand, some grass-roots organizations have run out of supplies, which meant some readjusting.
“Overall, the response from local partners has been immediate,” Mr Tyszko said. In certain cases, if stranded people could not get treatment locally, UNAIDS helped them to get supplies from the person’s native country.
He cannot believe how people have had to overcome so many hurdles to obtain HIV medicine despite a clear need.
“In times of crisis like COVID-19 or other public emergencies, governments should waive restrictions to make it easier for people to obtain refills and life-saving care, regardless of their legal status, residency or citizenship,” he said.
UNAIDS has been advocating for the right to health and universal health coverage to alleviate problems like this. A better integration of HIV and other health services could help some of the gaps in the AIDS response to be addressed, which will ultimately make it easier for people to access life-saving medicines, care and support.
For now, Mr Tyszko feels that helping people is very satisfying. “It’s been such a boost to do something so concrete with immediate effect,” he said.
Our work
Related


Feature Story
Communities strengthening the AIDS response in Nepal
21 May 2020
21 May 2020 21 May 2020From the very beginning, communities were in the vanguard of the AIDS response in Nepal. Still playing a vital role in the response to HIV in the country, communities are making good-quality services more accessible for people living with HIV and key populations and standing up to HIV-related stigma and discrimination.
“Nepal made antiretroviral medicines accessible to all people living with HIV as a result of advocacy efforts led by communities, human rights activists and other national stakeholders,” said Gopal Shrestha, a prominent community leader living with HIV.
Discrimination towards key populations is still deeply rooted in Nepalese society. “Finding people who need services is difficult due to a lack of trust. We work with those communities that fear coming out because of discrimination,” said Simran Sherchan, Operation Head of the Federation of Sexual and Gender Minorities in Nepal (FSGMN).
Although antiretroviral medicines are available to everyone living with HIV in Nepal, a survey conducted in 2018 reveals that more than 30% of transgender people avoid seeking health care because of fear of stigma and discrimination—something that FSGMN is determined to end.
“Community-based organizations play an intricate role in reaching out to those hard to reach,” said Anjay Kumar KC, a community leader who advocates for harm-reduction in Nepal. Recovering Nepal, a community network of people who use drugs, is supporting harm reduction programmes and HIV prevention among young people who use drugs, including a peer-to-peer programme that provides sterile needles and syringes and a campaign that promotes HIV testing. It has also played a key role in advocating with the government to initiate opioid substitution therapy, which is now offered at 12 sites in five provinces in the country.
Community-based organizations mobilize communities to demand services and advocate for their right to health. Recently, the National Association of People Living with HIV/AIDS (NAP+N) successfully advocated to include people living with HIV in the country’s Health Insurance Programme in 57 districts across the country. “NAP+N also entered into an agreement with Prime Life Insurance Limited to guarantee people living with HIV can access life insurance services,” said Rajesh Didiya, President of NAP+N.
Despite these achievements, community-based organizations face challenges. “When I reach out to sex workers, I have to hide my identity, because sex work is still stigmatized by my family and society. That is why it is difficult to publicly raise awareness about sex workers’ rights,” said Bijaya Dhakal, Coordinator of the Nepal Federation of Female Sex Workers.
Parina Limbu, a community leader who advocates for engagement in decision-making by women who use drugs, said, “Being labelled as women who use drugs, women living with HIV and hepatitis and sex workers, we are not within the reach of programmes. Our needs should not be looked at through the lens of males who use drugs. Women who use drugs need more decision-making spaces to make sure that our voices are heard.”
Those challenges can be overcome through partnerships and joint efforts, however. The Right to Health Women’s Group, Right Here Right Now and FSGMN have created a platform to collect and monitor cases of human rights violations against people living with HIV, key populations and young people. They use the evidence that they collect to advocate for programmes on stigma and discrimination reduction in health facilities and raise awareness about the human rights of key populations with law enforcement officers.
UNAIDS in Nepal has played a key role in empowering communities. “The important role that the community plays in the country’s response to HIV should not be underestimated. The gains made are because communities are taking the initiative and acting in ways that ensure that people who need treatment, prevention and related HIV services can access them,” said Masauso Nzima, UNAIDS Country Director for Nepal and Bhutan.
Video
Region/country
Related


Press Statement
UNAIDS urges governments to ensure that HIV service providers from community-led organizations are recognized as essential service providers in the context of COVID-19
18 May 2020 18 May 2020GENEVA, 18 May 2020—A cornerstone of the response to HIV, community-led health service delivery has become even more critical in the context of COVID-19, as the needs of marginalized community members and the burden on the health sector are increasing, making it vital that continued provision of HIV, tuberculosis and other health services is secured. Community-led organizations are providing a lifeline to underserved, marginalized and hard-to-reach populations around the world.
Physical distancing restrictions have created significant challenges for those needing to access essential services, creating an increased burden on community organizations, which are at the centre of service delivery.
UNAIDS recognizes that community organizations have an unparalleled depth of experience in creating and delivering responses to health and human rights crises within their communities. The many community-led networks and groups that emerged to respond to HIV possess immense practical experience, organizational strength and unparalleled community access for facilitating the delivery of life-saving support, and for influencing people’s real-life practices to better protect their health.
Community-led networks and organizations have also developed important working relationships and roles within health and community systems, including in coordination and task-shifting functions. As evidenced in many countries, these capacities can, with proper support, be deployed to facilitate the provision of COVID-19 information, prevention, testing and linkages to care. Yet without formal recognition of the essential nature of their work, they face significant barriers to continuing to provide services. It is the view of UNAIDS that it is critical to the COVID-19 response and to mitigating broader health impacts of the pandemic that community-led organizations be supported to continue to provide essential services and have the protective equipment and safe policy environment necessary to do so.
The role of community-led organizations must be appropriately recognized and supported in the context of COVID-19. They must be factored into all aspects of planning, design and implementation of interventions to combat both COVID-19 and the efforts required to mitigate the impact of COVID-19 on other health areas, including HIV and tuberculosis. In particular, and as first steps in this effort, UNAIDS urges COVID-19 crisis committees at the national and district levels to:
- Include the workforce of community-led health care services into the lists of essential service providers and treat them as equivalent to health-care providers.
- Design physical distancing restrictions and policies in ways that allow community-led services to continue operating safely. Essential services include, but are not limited to, the physical provision of HIV, tuberculosis and COVID-19 and other health services that include prevention commodities, including condoms, lubricants, clean needles and opioid substitution therapy, contraceptives, hygiene kits, test kits, medication, triage and linkage to care, adherence support, packages of food and other essentials, the provision of legal services and protection for survivors of gender-based violence and other forms of violence and discrimination. Particular attention needs to be paid to people with physical disabilities.
- Provide special authorization to relevant community-led service providers to move freely, with appropriate personal protective equipment, to deliver the services when and where needed.
- Ensure that community-led organizations, networks and groups be provided with personal protective equipment and training in order to protect themselves and their clients in the course of service delivery.
- Take urgent measures to ensure the security, and expansion, of existing funding for community-led organizations, so that those organizations can continue to provide services.
- Ensure inclusive and transparent governance of COVID-19 responses, with decision-making bodies that include representatives of community-led organizations, including those focused on gender, equity and human rights, to ensure that COVID-19 policies are designed to support the range of service providers and activities necessary for an effective and equitable response.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work
Press centre
Download the printable version (PDF)



Feature Story
A tribute to Charles Domingo Noubissi
01 May 2020
01 May 2020 01 May 2020“Le baobab est tombé.” “The baobab has fallen,” was Francine Nganhale’s post against a black backdrop on her Facebook page on 30 April 2020.
Her husband, Charles Domingo Noubissi, had died.
Many couldn’t believe it, because Mr Noubissi had such a fighting spirit. He had health problems, but rarely missed a meeting to advocate for the response to HIV.
As President of the Board of Directors of the Cameroonian Network of Associations of People Living with HIV, he became a pillar of the AIDS response in his country and across the region.
We will miss him dearly and thank him for his years of leadership and commitment and for being a champion of the community-led response.
UNAIDS had the pleasure of interviewing Charles Noubissi and his wife in 2019, showcasing proud people living with HIV. Here is that story:
Region/country
Related


Feature Story
Talking about a revolution
24 March 2020
24 March 2020 24 March 2020It is no surprise that Birknesh Teferi’s first name means “revolution” in Amharic, the language spoken in Ethiopia. She exudes passion and self-pride; she’s the picture of health and well-being.
Her journey to this point in her life is indeed revolutionary—a story of resilience, hope and transformation. She has beaten tuberculosis (TB), survived cervical cancer and is living positively with HIV.
Ms Teferi was diagnosed with HIV and TB in 2003, a time when information about HIV, TB and sexual and reproductive health in Ethiopia was scarce and stigma and discrimination high.
According to the World Health Organization (WHO), Ethiopia is one of the 48 high-burden TB countries globally. In 2018 in the country, 165 000 people fell ill with TB and there were 27 000 deaths; 2200 of which were among people living with HIV.
After waiting 15 days for her test results, while the health-care worker went on leave, Ms Teferi was told that she was “positive”.
“I thought it was good news. I hugged the nurse in relief, only for her to tell me that being HIV-positive meant I had the virus,” she said.
Ms Teferi successfully underwent the WHO recommended treatment for TB—directly observed treatment short-course (DOTS)—which cured the TB but did not help her with her struggle to accept her HIV status.
“What followed was a period of hurt and heartbreak … Waiting for death,” she recalled of the aftermath of her diagnosis.
She describes herself then as a “drifter.” She did not disclose her HIV status because of stigma and worked as a sex worker to make ends meet.
“If a client had a condom, we would use it. If he didn’t, we didn’t. I tried to use them, but I had no money to buy them. That’s how I developed a sexually transmitted infection.”
During the treatment of the infection, Ms Teferi was diagnosed with cervical cancer and was referred from one health facility to the next, often in different towns.
She eventually found a “caring” doctor and had an operation to treat the cancer. “I was in so much pain, I couldn’t sit. I was miserable,” she remembers.
But when Ms Teferi started to take HIV treatment in 2008, her life slowly changed. She started to look after herself more. She insisted on condom use with her clients.
She met a group of women living with HIV from the Tilla Association of HIV-Positive Women in Hawassa, Ethiopia. The association focuses on capacity-building and training and support of women living with HIV. It runs an embroidery centre as an income-generating activity for women living with HIV, where Ms Teferi now works.
“I am now free of drifting. Life is so much better. If people feel that it is possible to live, possible to work, then life can change,” she said.
For the first eight months of her time at the centre, the manager assigned her a volunteer to help her with her physical recovery from her operation. For the first time, she had support from other women who understood what it was like to be her.
The women at the centre invited her to watch a film about living positively with HIV. “That movie gave me hope,” she says. “I started to learn more about HIV from my manager. I gradually got relief, better medical services and Tilla supported me financially and emotionally.”
While Ms Teferi is on HIV treatment and has been cured of TB, there are millions of people worldwide who still lack access to prevention and treatment for both conditions. TB is the leading cause of death among people living with HIV globally.
In 2018, there were an estimated 1.2 million TB deaths, 251 000 of which were among people living with HIV—this is a 60% reduction from 620 000 in 2000. Between 2000 and 2018, TB treatment alone averted an estimated 48 million deaths among HIV-negative people and TB treatment supported by antiretroviral therapy averted an additional 10 million deaths. However, progress is slow and needs to be accelerated in order to end TB by 2030 as part of the Sustainable Development Goals.
“TB is curable and preventable,” said Aeneas Chuma, the Director for the UNAIDS Regional Support Team for Eastern and Southern Africa, a.i. “It is critical in this moment of history, in the context of the global COVID-19 pandemic, that we ensure that people living with HIV who are diagnosed with TB have uninterrupted access to HIV and TB treatment. UNAIDS is working with governments and community partners to ensure that we adapt to a rapidly changing health context, with kindness, compassion and humanity.”
Resources
Region/country

Feature Story
Chains of solidarity and kindness during the COVID-19 outbreak
20 March 2020
20 March 2020 20 March 2020Getting calls at all hours of the day is not unusual for Liu Jie, the Community Mobilization Officer in the UNAIDS Country Office in China. Because of the COVID-19 outbreak in China, the whole office has been active in helping people living with HIV to continue to access treatment, especially in Hubei Province, where the pandemic was first reported. Recently, Ms Liu was surprised when she had a call from Poland.
"A Chinese man introduced himself, saying he is stranded and will run out of HIV medicine in two days,” Ms Liu said.
With travel restrictions closing down more and more countries, the man could neither return home nor access medicine. Not knowing what to do, he reached out to a Chinese community-based organization, the Birch Forest National Alliance, and through them contacted UNAIDS in Beijing, she explained.
He, like countless other people abroad, was caught in limbo by the fallout from the COVID-19 outbreak. Days earlier, the UNAIDS Country Office in China had helped another Chinese person living with HIV access medicine while stuck in Angola. In both cases, colleagues in Beijing reached out to UNAIDS country offices and the Community Mobilization Team in Geneva, Switzerland. The UNAIDS Country Director for Angola reached out to the Angolan Network of AIDS Service Organisations and the person accessed medicine in no time.
For the case in Poland, Jacek Tyszko, a Polish native and part of the UNAIDS Community Mobilization Team, knew exactly what to do. “Because we have been in touch with regional networks of people living with HIV in central and eastern Europe, I made one call,” Mr Tyszko said.
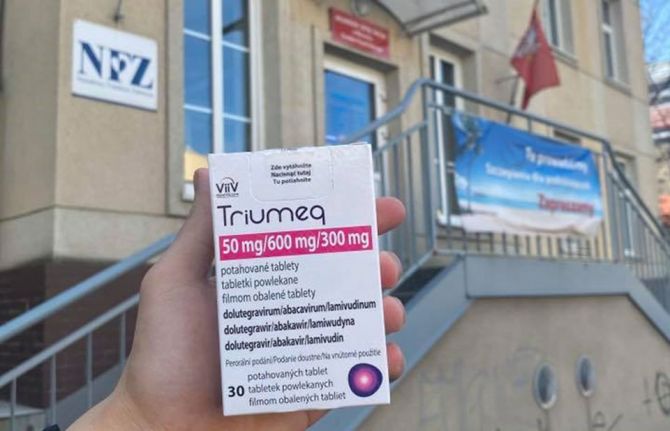
Anna Marzec-Boguslawska, head of the National AIDS Center in Poland, quickly agreed to follow up. She has always been very responsive, which allows us to move quickly on the ground. Twenty-four hours later, Ms Liu received a photo of a man holding up a box of medicine in front of a grey building. Minutes later her phone rang.
“It was the same Chinese guy calling again from Poland,” she said. “He was crying with joy, saying he had his medicine and that was a picture of him just now.”
She added, “He kept saying how he could not believe that we made the impossible possible.”
The Director of the Birch Forest National Alliance, Bai Hua, also thanked UNAIDS. “This case really reflects that UNAIDS is rooted among the communities,” he said.






