Update
Fast-Track cities reaching the 90–90–90 targets
18 July 2016
18 July 2016 18 July 2016Fast-Track cities are making tangible progress towards the 90–90–90 targets of 90% of people living with HIV knowing their HIV status, 90% of people who know their HIV-positive status accessing treatment and 90% of people on treatment having suppressed viral loads.
Four signatories to the Paris Declaration on Fast-Track Cities released data today demonstrating significant progress towards achieving the 90–90–90 targets and confirming their commitment to ending AIDS in their cities. The announcement was made at a satellite meeting cohosted by the International Association of Providers of AIDS Care (IAPAC) and UNAIDS at the 21st International AIDS Conference, taking place in Durban, South Africa.
Amsterdam, Denver, Paris and Kyiv announced their 90–90–90 data as part of the Fast-Track approach by cities around the world to reach ambitious goals by 2020 in order to end the AIDS epidemic by 2030. Achieving these goals requires accelerated and focused action, innovation in service delivery and working in partnership with key stakeholders and affected populations.
IAPAC has launched a Fast-Track cities web portal with dashboards for five cities: Amsterdam, Netherlands; Denver, United States of America; Kyiv, Ukraine; Paris, France; and San Francisco, United States. The dashboards include data on cities’ progress in reaching the 90–90–90 targets for 2020 and their broader response to HIV. The dashboards can be seen at www.Fast-TrackCities.org.
Quotes
“People must be at the centre of the response to HIV in urban settings to reach the 90–90–90 targets. City health systems that are inclusive and accessible have the best chance of engaging people who might otherwise be left behind, including young women and adolescent girls and key populations—gay men and other men who have sex with men, transgender people, sex workers and their clients, people who inject drugs and prisoners.”
“Attaining the 90–90–90 and zero discrimination and stigma targets in high HIV burden cities is grounded in data-driven HIV care continuum optimization that aims to leave no one behind and holds stakeholders accountable.”
Resources
Related






Update
Call issued for global partnership to end paediatric AIDS
06 June 2016
06 June 2016 06 June 2016African health ministers, leaders of paediatric HIV treatment programme implementers, philanthropic foundations, civil society and private sector partners convened in New York, United States of America, on 6 June to celebrate successes in closing HIV treatment gaps for children and to call for an expanded global partnership to build on this momentum to end paediatric AIDS.
Many countries have made important strides towards ending paediatric AIDS, but major challenges persist. Even as the number of children newly infected with HIV continues to decline, only about half of HIV-exposed children are tested for HIV within the first two months of life and only 30% of children living with HIV are linked to HIV treatment in a timely manner. Because far too many children living with HIV begin treatment too late, children are far more likely than adults living with HIV to die of AIDS-related illnesses.
At a major global ministerial meeting in Abidjan, Côte d’Ivoire, in May, health ministers from Africa endorsed a Fast-Track approach for children. This approach calls for reaching a 95% coverage of antiretroviral therapy for both pregnant women and children living with HIV by 2018. By reaching this target, the world could effectively end paediatric AIDS by 2020—one decade earlier than the elimination goal for the epidemic as a whole.
To reach these ambitious targets, attendees at this week’s meeting in New York emphasized the importance of a renewed, expanded, inclusive global partnership to close the paediatric HIV treatment gap. During an interactive conversation among the meeting participants, speakers emphasized the importance of involving families, communities and civil society organizations. There was also agreement regarding the need to engage the private sector in efforts to develop new paediatric treatment tools and fund programmes to close gaps across the continuum of care for children. The Medicines Patent Pool, which has prioritized paediatric HIV treatment in its negotiations of licences for the generic manufacture of priority antiretroviral medicines, is an example of how innovative approaches to private sector involvement can contribute to improved access to essential treatments.
Meeting attendees stressed the need for improved coordination of the many efforts being undertaken to address various aspects of paediatric HIV treatment. At the Abidjan meeting, health ministers endorsed efforts to maximize coordination in the paediatric AIDS arena.
To achieve the Fast-Track Targets for children—and to sustain these gains over time—new resources will be needed. Several countries are taking steps to increase domestic allocations for paediatric HIV treatment. Namibia, for example, covers 60% of its national AIDS response with domestic resources, and Felix Kabange Numbi, Minister of Public Health for the Democratic Republic of the Congo, reported that his country is pledging to increase domestic resources for AIDS.
It was agreed that philanthropy offers a potentially important avenue to generate new resources for paediatric HIV treatment. ELMA Philanthropies, for example, is allocating US$ 12.5–15 million per year for at least the next three years to support HIV treatment programmes for children, with a comparable amount to be invested in supportive programmes for childhood development.
Quotes
"We must build on our momentum to finally end the AIDS epidemic once and for all. The outcomes across the continuum of care for children need to be strengthened."
“We need a new solidarity. We need a new movement that focuses on ending paediatric AIDS. This new movement is about ending inequities, it is about social justice.”
“One person, one country, one company can change the world. I know we are going to reach our global goals for ending paediatric AIDS.”
“There is no mystery about what we need to do. We need a resurgence of political will and to zero in on reaching the mothers, infants, children and adolescents who are being left behind.”
“It is unacceptable to deny children their right to a chance at life. If we fail to build on recent momentum in order to end paediatric AIDS, both history and the world’s children should judge us harshly.”
“We need more consistent communication among partners working on paediatric HIV treatment, and our sense of accountability needs to be aligned so that it is fit for our objective to end paediatric AIDS.”
“Governments can do many things well, but there are some things we don’t always do well. We can look to our private sector partners for the introduction of new technologies and for better ways to hold ourselves accountable.”








Update
Urgent need to strengthen community health systems to achieve the 90–90–90 treatment target
10 June 2016
10 June 2016 10 June 2016The 90–90–90 treatment target cannot be reached without a substantially greater involvement of a well-resourced and well-trained community health workforce, experts told a side event at the United Nations General Assembly High-Level Meeting on Ending AIDS, taking place in New York, United States of America, from 8 to 10 June.
Speakers at the side event, held on 9 June and entitled “90–90–90 and human resources for health,” emphasized that the 90–90–90 treatment target offers a road map towards the ultimate goal of ending the AIDS epidemic by 2030. However, shortages in human resources for health pose a grave threat to hopes for ending the epidemic as a public health threat.
Community health workers represent a potentially transformative mechanism for closing health workforce gaps and accelerating progress in scaling up HIV treatment and improving treatment outcomes. Kesetebirhan Admasu, Minister of Health of Ethiopia, described how the country’s health extension worker programme has substantially improved health-care access and helped make health services more sensitive to the needs of communities.
Community health systems are especially critical for ensuring access to essential health services among people who face challenges in accessing mainstream services, including members of key populations. Surang Janyam, of the Service Workers In Group in Thailand, explained how trained community health workers have expanded access to HIV services among sex workers, men who have sex with men and transgender people in Thailand and increased community ownership of the AIDS response.
Sigrun Mogedal, of the Global Health Workforce Alliance, said that the AIDS response should partner and coordinate closely with the many efforts already being undertaken to strengthen the health workforce. In 2016, the World Health Assembly approved a new global strategy for the health workforce, prioritizing the strengthening of community health systems. The Earth Institute of Columbia University is spearheading a global partnership to mobilize 1 million community health workers in Africa, and countries such as Ghana have taken important steps to train and deploy new cadres of community health workers.
However, the lack of growth in international HIV assistance potentially jeopardizes the world’s capacity to build a strong and durable health workforce to achieve the 90–90–90 treatment target, speakers in the session emphasized. Jeffrey Sachs, Director of the Earth Institute, and Stephen Lewis, Co-Founder of AIDS-Free World, called for urgent action to mobilize new resources for AIDS and to ensure that sufficient new funding is channelled to community systems.
Quotes
“We need to generate broad global commitment and action to ensure sufficient human resources to achieve 90–90–90.”
By moving from service client to service provider, communities can provide testing, antiretroviral therapy and pre-exposure prophylaxis for our members.”
“We need to consider task-shifting to patient groups and to patients themselves. These models are now being brought to scale in some provinces. We need more patient autonomy and more self-administered therapy. Treatment needs to fit into people’s lives, not the other way around.”
“Reaching 90–90–90 is absolutely vital and indispensable for turning the tide against the epidemic.”
“We know technically how to end the AIDS epidemic. 90–90–90 is especially important because it mobilizes our efforts not only for the decency and humanity of keeping people alive but also to end transmission of this disease and to bring this epidemic to a full close.”
“The vital role of community health workers has to be maximized if we hope to reach 90–90–90. The AIDS movement shows us what can be achieved through communities. We must work hand in hand with communities and provide them with the human and financial resources they need to fulfil their mission.”
“I appeal for the mobilization of all the people and resources and the implementation of large-scale resources to end paediatric AIDS. I ask you to give a voice to those who have no voice.”
"Ten to 15 years ago human resources for health was not on the table. Today, we have come a long way to create an agenda for the health workforce. As we now talk about what we can do in the AIDS movement to reach that extra step to those who are denied services, we have partners . . . We should not go alone.”
Related




Update
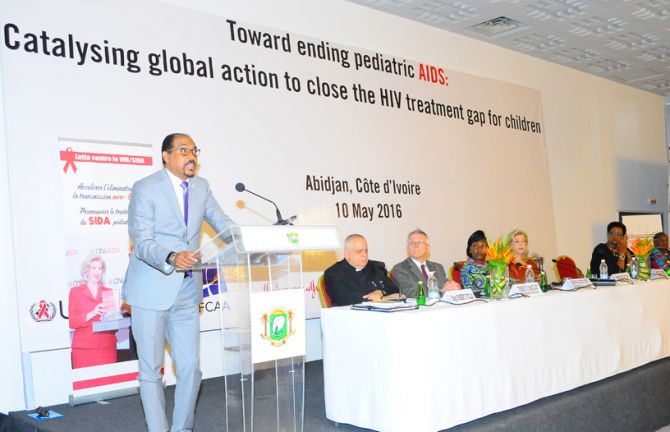
African ministers call for global effort to end paediatric AIDS
10 May 2016
10 May 2016 10 May 2016African ministers of health called on the international community to make ending the paediatric AIDS epidemic a global political priority. Meeting in Abidjan, Côte d’Ivoire, on 10 May, dignitaries called for the Political Declaration on Ending AIDS, to be agreed upon at the upcoming United Nations General Assembly High-Level Meeting on Ending AIDS, to include targets to scale up prevention of mother-to-child transmission of HIV services and paediatric HIV testing and treatment.
Participants included 11 national ministers, as well as deputy ministers and senior HIV programme officials from across Africa, which is home to nearly 90% of all children living with HIV.
In 2014, 2.6 million children were living with HIV and 32% had access to antiretroviral therapy. Without treatment, half of all children living with HIV will die before they are two years old.
“Ending paediatric AIDS requires action at two levels,” said the First Lady of Côte d’Ivoire, Dominique Ouattara, UNAIDS Special Ambassador for the Elimination of Mother-to-Child Transmission and the Promotion of Paediatric Treatment for HIV. “On the one hand, we must prevent new HIV infections among children, and, on the other hand, we must provide treatment and care to all children who are living with HIV.”
Continued progress in preventing new HIV infections among children has been made by ensuring all pregnant women are tested for HIV and women living with HIV receive treatment. This has established a strong foundation for ending paediatric AIDS. But to make it a thing of the past, substantially better results are needed across the HIV treatment cascade for children.
UNAIDS projects that it is possible to end the epidemic of paediatric AIDS by 2020 if prevention and treatment targets are met by 2018. These include reaching 95% treatment coverage for both pregnant women and children living with HIV.
Recent trends point towards the feasibility of achieving these targets. Major gains have been made in providing antiretroviral medicines to pregnant women living with HIV to prevent transmission of HIV to their babies. From 2010 to 2014, new HIV infections among children dropped by 58%. In the same period, HIV treatment coverage among children living with HIV more than doubled.
However, more needs to be done to ensure that no child is left behind. “Today we have effective treatment regimens, yet how many children are still dying in the age of antiretroviral therapy?,” asked Jeanne Gapiya Niyonzima, president of the Burundi Association Nationale de Soutien aux Séropositifs et aux Malades du SIDA and mother of a child who died of AIDS-related causes at 18 months of age.
“This is a question of social justice, a question of equality,” said UNAIDS Executive Director Michel Sidibé. “We have the opportunity to have a Political Declaration on Ending AIDS from the United Nations General Assembly High-Level Meeting on Ending AIDS to help us set concrete objectives so that treatment becomes universal for everyone, wherever they find themselves.”
The African ministers attending the Abidjan meeting called for the Political Declaration on Ending AIDS to include clear targets to scale up prevention and treatment services in order to end paediatric AIDS. To achieve these targets, the ministers endorsed the immediate front-loading of resources for paediatric HIV treatment and the elimination of mother-to-child transmission of HIV.
Scientific developments have the potential to dramatically improve treatment outcomes for children. Ministers noted the importance of fully leveraging and scaling up innovative tools, including point-of-care technologies for early infant diagnosis, paediatric treatment regimens recommended by the World Health Organization and family-centred service delivery approaches that improve retention in care and treatment adherence.
Ministers called for UNAIDS to coordinate initiatives on paediatric HIV treatment across all sectors. “We need to strengthen cooperation among stakeholders to get better results for children,” said Juliet Kavetuna, Deputy Minister of Health and Social Services of Namibia. “If we work in silos, we will never achieve our goal.”
The meeting generated considerable optimism regarding the potential to meet the 2018 targets for children. “We know what we have to do,” said David Parirenyatwa, Zimbabwe’s Minister of Health and Child Care. “The key is to do it in a systematic way and ensure that it is well-funded.”
Uganda’s Minister of State for Primary Health Care, Sarah Opendi, said, “Working together, we can end the AIDS epidemic among children, and also among adults.”
Prior to the closing remarks by the First Lady of Côte d’Ivoire, Mr Sidibé was presented with the Grand Officier de l'Ordre National de la République de Côte d'Ivoire, in recognition of his global leadership on behalf of children affected by HIV. In accepting the award, Mr Sidibé encouraged all participants to work towards the goal of ending paediatric AIDS.
Leading donors, programme implementers and civil society involved in paediatric HIV treatment, as well as private industry, also attended the ministerial meeting. The event was convened by UNAIDS, the Government of Côte d’Ivoire, ELMA Philanthropies, Funders Concerned About AIDS, the Children’s Investment Fund Foundation, Johnson & Johnson and Luxembourg. More than 150 people from 34 countries participated.
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025






Feature Story
UNAIDS joins forces with the One Million Community Health Workers campaign to achieve the 90–90–90 treatment target
02 February 2016
02 February 2016 02 February 2016UNAIDS and the One Million Community Health Workers (1mCHW) initiative have announced a major strategic partnership to support the achievement of the 90–90–90 treatment target and to lay the foundation for sustainable health and development.
The new partnership emerged at a high-level meeting of eight African health ministers and other stakeholders in Addis Ababa, Ethiopia, held on 1 February, which focused on the 90–90–90 treatment target and human resources for health. The participants of the meeting called for the world to leverage the aim of achieving the 90–90–90 treatment target to strengthen human resources for health.
In his opening address, Marc Angel, UNAIDS champion for the 90-90-90 treatment target, told participants that increased human resources for health would be essential.
“Achieving the 90-90-90 target requires health workers, specific expertise and laboratories equipped with the necessary materials,” said Mr Angel.
Jeffrey Sachs, director of the Earth Institute at New York’s Columbia University and founder of the 1mCHW initiative, emphasized his commitment to the 90–90–90 treatment target. As the United Nations Secretary-General’s Special Adviser on the Sustainable Development Goals (SDGs), Mr Sachs pledged to place 90–90–90 at the centre of advocacy for the SDGs.
“The 90–90–90 effort of UNAIDS is historic: a rigorous, scientific and bold approach to end the AIDS epidemic,” Mr Sachs said. “The end of AIDS is within reach, and community health workers will play a pivotal role in empowering communities to end deaths from AIDS and to break the transmission of the virus. The 1 Million Community Health Worker campaign is honoured to join UNAIDS in its path-breaking programme.”
Cosponsored by UNAIDS, the African Union and Ethiopia’s Ministry of Health, the meeting revealed both strong support for the 90–90–90 treatment target and agreement that it offers a unique opportunity to recruit and mobilize hundreds of thousands of community health workers.
“Ethiopia will spare no efforts to reach the 90–90–90 treatment target,” said Kesetebirhan Admasu, Ethiopia’s Minister of Health. “We are determined to relegate AIDS to the books of history.”
To reach the 90–90–90 treatment target, the number of people accessing antiretroviral therapy will need roughly to double over the next five years. While HIV programmes have pioneered innovative strategies to enhance the efficiency of service delivery, it is clear that reaching the target will require expanding the number of health workers available to deliver HIV services.
However, many African countries, as well as countries in other regions, have an acute shortage of health workers. Although Africa accounts for 25% of the global health burden, the region is home to only 3% of all health workers.
To ease health worker shortages, the meeting focused on the importance of training and employing trained, provisioned, supervised and remunerated community health workers to expand access to HIV services. “We must reinforce the interface between communities and the service provider,” said UNAIDS Executive Director Michel Sidibé. “We need to use communities and civil society organizations to reach people who are difficult to reach.”
The 1mCHW campaign unites more than 150 organizations worldwide in a major global effort to recruit and deploy trained, equipped, supervised and remunerated community health workers, with particular attention to especially underserved rural communities.
Countries such as Ethiopia, Ghana and Malawi have already taken major steps to train and deploy community health workers to deliver community-based health services. Ethiopia, for example, has trained tens of thousands of health extension workers, who have substantially increased access to good-quality health services. Creation of the community health worker programme in Ethiopia has been associated with a 19-year increase in life expectancy over two decades. Ghana is in the process of deploying 20 000 community health workers in a national scale-up effort.
Other countries are moving to emulate these successful national efforts to expand human resources for health. Lesotho, for example, is embarking on a national effort to create a cadre of health extension workers, with mentoring provided by Ethiopia and Malawi.
Much of the discussion during the one-day meeting focused on how the push to achieve the 90–90–90 treatment target can help drive a sustainable expansion of human resources for health. The global effort to achieve the 90–90–90 treatment target will involve the delivery of simplified, decentralized care to millions of healthy people living with HIV. Self-care, including through such innovations as peer-driven adherence clubs and community distribution of antiretroviral therapy, will play a vital role in the delivery of HIV chronic care management.
Community health workers will be essential for providing these simplified, decentralized services. The Fast-Track approach calls for a sharp increase in financing for community service delivery and an increase in the proportion of HIV services that are delivered through community channels from 5% currently to 30%.
The same community-centred models that will be critical for ending the AIDS epidemic as a public health threat also have a potentially key role to play in addressing the other health targets in the SDGs. Community health workers mobilized through the push to achieve the 90–90–90 treatment target can also help in the delivery of other important health services. Similarly, the chronic care models generated by HIV treatment scale-up are applicable to the management of the growing burden of noncommunicable diseases, such as hypertension and diabetes.
Although the road map for action is clear on 90–90–90 and the health workforce, financing remains a potential obstacle, as investments will be needed for training, supervision and compensation for community workers. There was agreement among health ministers and other participants that mobilizing the necessary investments for expanding the health workforce will require both increased domestic outlays and further increases in international assistance. Mr Sachs called for the creation of a fund for strengthening health systems.
“Here in Africa, we must commit our own domestic resources for health,” said Olawale Maiyegun, Director of Social Affairs for the African Union Commission. “We must live up to our commitments in the Abuja Declaration to dedicate at least 15% of our domestic budget to health.”
“Health is not a cost,” Mr Sidibé said. “Health is not expenditure. Health is an investment. If we scale up, we can bring the epidemic to an end. Yet if we don’t come up with the resources we need, AIDS will rebound, and all our investments in the last 30 years will be lost.”
In planning the meeting, the cosponsors worked with the World Health Organization, the African Society for Laboratory Medicine, the International Association of Providers of AIDS Care, the International Federation of Red Cross and Red Crescent Societies, the Office of the United States Global AIDS Coordinator, Columbia University, the Sustainable Development Solutions Network, the One Million Community Health Workers campaign and the Government of Luxembourg.
Region/country


Update
UNAIDS and Luxembourg promote the 90–90–90 treatment target
09 November 2015
09 November 2015 09 November 2015The ambitious HIV treatment target set for 2020 greatly influenced governments and partners in their approach to the AIDS response, said senior officials of Luxembourg and UNAIDS at a briefing for diplomatic missions in Geneva, Switzerland, on 9 November.
Efforts to scale up treatment in the next five years are crucial to ending the AIDS epidemic. The 90–90–90 treatment target for 2020 calls for 90% of people living with HIV to know their HIV status, 90% of people who know their HIV-positive status to access antiretroviral treatment and 90% of people on treatment to have suppressed viral loads.
Unlike earlier treatment targets, which focused solely on the number of people starting HIV treatment, 90–90–90 focuses on the ultimate aim of HIV treatment—viral suppression, which significantly reduces both the risk of HIV-related illness and death and the risk of HIV transmission.
At the briefing, speakers from UNAIDS and Luxembourg outlined priority areas to implement 90–90–90. They reiterated that the political will and the scientific tools exist to end the AIDS epidemic. Success has been achieved in different areas and regions of the world, but more needs to be done to ensure that no one is left behind and to close the treatment gap for children.
Luxembourg, a longstanding supporter of UNAIDS, became a strategic partner this year in the push to end the AIDS epidemic as a public health threat by 2030. The alliance between UNAIDS and Luxembourg aims to leverage the therapeutic and preventive benefits of antiretroviral therapy.
At the briefing, Marc Angel of Luxembourg was appointed as a UNAIDS champion for the 90–90–90 treatment target. He has been an AIDS advocate for more than 25 years.
As a member of the Chamber of Deputies of Luxembourg since 2004, Mr Angel serves as the Chairman of the Committee for Foreign and European Affairs, for Defence, for Cooperation and Development and for Immigration of the Luxembourg Parliament.
Quotes
“Luxembourg has been a champion in supporting and providing catalytic resources to the Fast-Track approach, which will be a reality first in Africa. Several countries are very close to achieving the target. The challenge today is to make the 90–90–90 treatment target a reality for the people who are being left behind, for key populations.”
“Luxembourg is leveraging political, technical and financial support to accelerate access to antiretroviral therapy.”
“The 90–90–90 target is much more than just a treatment target. It is about bringing hope and help to people to live healthy lives and creating a better future. That is why I am proud to champion this initiative and to partner with UNAIDS.”
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025


Feature Story
Global scientific leaders explore strategies to achieve the 90-90-90 target
22 July 2015
22 July 2015 22 July 2015Leading HIV researchers describing results from multiple clinical trials in sub-Saharan Africa report that innovative service delivery models are achieving results across the HIV treatment cascade that approach or exceed the 90–90–90 target.
Study results were presented at an all-day workshop hosted by the British Columbia Centre for Excellence in HIV/AIDS and the Division of AIDS at the University of British Columbia, prior to the opening of the 8th International AIDS Society Conference on HIV Pathogenesis, Treatment and Prevention in Vancouver, Canada. The studies are being undertaken in a number of high-burden countries in sub-Saharan Africa, including Botswana, Kenya, Malawi, South Africa, Swaziland, Uganda and Zambia.
“These exceptional clinical trial results show yet again how innovation is driving progress in the AIDS response,” said UNAIDS Executive Director Michel Sidibé. “The results demonstrate that the 90–90–90 target is more than a dream. It is entirely feasible.”
Diane Havlir, of the University of California, San Francisco, presented interim results from the Sustainable East Africa Research for Community Health (SEARCH) trial in more than 30 rural communities in Kenya and Uganda. Having enrolled more than 334 000 people, the SEARCH trial is evaluating a multicomponent programme, including use of community-centred, multidisease campaigns to provide HIV testing and link HIV-positive individuals to immediate initiation of antiretroviral therapy.
At a population level, the SEARCH programme has achieved 90% knowledge of HIV status. Among participants living with HIV, more than 90% of people in Uganda and 83% in Kenya are receiving antiretroviral therapy. At 24 weeks, 92% of trial participants who have initiated antiretroviral therapy have achieved viral suppression.
Similarly encouraging, although preliminary, results were reported from the PopART trial by Richard Hayes of the London School of Hygiene and Tropical Medicine. Working in 21 communities, the trial is evaluating a combination HIV prevention package that includes repeated rounds of community-level HIV testing and immediate initiation of antiretroviral therapy for all people who are diagnosed HIV-positive. Among more than 115 000 community members enumerated in the trial, 90% of all men living with HIV and 92% of all women living with HIV were aware of their HIV status following the PopART programme. Among people with an HIV diagnosis, 62% of men and 65% of women were receiving antiretroviral therapy, highlighting the need to further strengthen linkage to care for people living with HIV. Data on rates of viral suppression among PopART participations will be available next year.
Max Essex, of the Harvard University School of Public Health, presented baseline findings for the Botswana Combination Prevention Protocol. Mr Essex and his colleagues have found that 79% of all people living with HIV in Botswana knew their HIV status as of mid-2015, 86% of adults who have been diagnosed with HIV were receiving antiretroviral therapy and 96% of people receiving antiretroviral therapy had achieved viral suppression.
Comparably impressive results have been achieved by a Médicins Sans Frontières (MSF) programme in the District of Chiradzulu in Malawi, according to David Maman of MSF. In Chiradzulu, 77% of all people living with HIV know their HIV status, 84% of people with an HIV diagnosis are receiving antiretroviral therapy and 91% of people receiving antiretroviral therapy have achieved viral suppression.
François Dabis, of the Bordeaux School of Public Health, described preliminary results from a separate trial in the Hlabisa district in KwaZulu-Natal, South Africa, of a test-and-treat initiative that includes six-month rounds of community-level testing and establishment of antiretroviral treatment sites in all communities in the study. Among more than 26 000 people in the study communities, 85% know their HIV status. Among HIV-diagnosed people reached by the programme, 86% are receiving antiretroviral therapy. Study results indicate that linkage to care remains suboptimal and an important focus of further work and innovation.
Several important themes emerged from these study findings. Researchers emphasized the importance and value of engaging and collaborating with local communities in developing programme approaches tailored to local needs and circumstances. Most of the studies have also taken multidisciplinary approaches to the development, monitoring and evaluation of programmes, involving social scientists, economists and community representatives as well as clinicians and biostatisticians.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Documents
Diagnostics access initiative to achieve the 90-90-90 treatment target
22 April 2015
The world is uniting around an ambitious HIV treatment target to lay the groundwork to end the AIDS epidemic as a public health threat by 2030. Through national, regional and global-level consultations, diverse stakeholders are pledging to ensure that by 2020: 90% of people living with HIV know their HIV status; 90% of people who know their status receive treatment; 90% of people on HIV treatment have a suppressed viral load.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment
Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment

21 January 2025
UNAIDS data 2024
02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024